Abstract
Conventional myoelectric prosthetic hands only offer a basic tri-digital pinch. Transradial amputees need to compensate for this lack of function with altered kinematics at the shoulder and trunk that might expose them to an increased risk of musculoskeletal injuries. A poly-articulated prosthetic hand may reduce the physical compensatory movements and close the gap between the sound and the prosthetic side. Six male transradial amputees completed four standardized reach-and-grasp activities with their tri-digital, poly-articulated and sound side hands. Trunk, shoulder girdle, scapula and humerus kinematics were measured with an optoelectronic system. Differences between hands were analyzed in terms of the amplitude of motion, the duration of the altered kinematics over the motion cycle, peak-to-peak amplitude and time to complete the activity. An overall score was defined, which assigned three points when the kinematics of a joint angle was altered for over 41% of the motion cycle, two points between 11 ÷ 40% and one point between 1 ÷ 10%; thus, a lower score indicates less variation from normal kinematics. Despite no changes in times, tri-digital vs. sound hand scored 93 points, tri-digital vs. poly-articulated hands scored 49 and poly-articulated vs. sound hand scored 28, supporting the hypotheses of the poly-articulated hand positively affects shoulder and trunk kinematics.
1. Introduction
Humans use their hands to learn and interact with the environment. A unilateral amputation is an irreparable damage to a person, compromising their life and forcing amputees to modify their strategy to perform activities of daily living (ADLs) [1]. Improvement in daily life can be influenced by the type of prosthesis [2]. The actual commercial solutions are typically driven with proportional or on/off control [3] with a limited number of grasping configurations. Usually, the prosthetic hand’s opening and closing are the only possible functions performed by using sEMG signals related to the flexion and extension of the wrist [4]. To overcome the restriction imposed by the artificial limb and facilitate task completion, amputees tend to introduce proximal compensatory movements in the residual joints [5,6].
Indeed, in most ADLs, the upper-limb and trunk function to position and orient the hand to reach/grasp a desired object and effectively and efficiently transport it to the aimed target. Commonly, transradial amputees using a myoelectric prosthesis need to compensate for the availability of a single “tri-digital” pinch and the loss of wrist function, resulting in non-physiological movements of the elbow, shoulder, trunk and neck [7,8]. This exposes the amputee to developing cumulative musculoskeletal disorders [9,10,11,12].
Over the last ten years, innovative prosthetic systems have become commercially available. With different technical solutions, these systems include a myoelectric hand capable of multiple grips and a passive wrist. Therefore, they have the potential to close the gap between the sound and the prosthetic side and decrease physical compensatory movements.
Nonetheless, at present, no studies are available to quantitatively support this statement, and the potential biomechanical advantage remains a matter of speculation.
In [13], a significant reduction in the upper limb and trunk compensatory movements in two out of nine common ADLs have been found. The sample was exclusively constituted of body-powered and myoelectric prostheses users. The lack of difference in compensatory movements resulted from the heterogeneity among study participants, particularly regarding the experience of using the artificial limb, correlated with the user motion strategy [6].
The literature lacks a within-subject comparison, which should highlight the modification in the compensatory strategy of expert prosthesis users concerning the type of artificial limb and quantify the improvement derived from using devices with different technology levels.
The present study aimed to fill this lack of knowledge, by comparing the compensatory movements at the shoulder and trunk when amputees performed standardized activities with a tri-digital myoelectric hand, a poly-articulated myoelectric hand, and the patient’s sound side hand. The results could help develop rehabilitation strategies and give useful information to design solutions and avoid compensatory shoulder movements.
2. Materials and Methods
2.1. Participants
Participants were recruited from inside the Centro Protesi Inail (Vigorso di Budrio, Bologna, Italy—hereafter CP). CP is the prosthetic center of the Italian workers’ compensation authority, which provides healthcare services to people with neuro-motor and musculoskeletal impairments, mainly acquired at work. The inclusion criteria were: (i) age 18–65 (working age), (ii) unilateral transradial amputation, (iii) active prosthesis user (based on the usual tear of gloves returned to CP), (iv) work-related traumatic amputation, (v) preserved function of the contralateral limb, (vi) stable stump, and (vii) presence of at least a single, usable EMG signal. The same patients participated in a separate functional and psychosocial assessment reported in [14]. The study was conducted following the Declaration of Helsinki and was approved by the Institutional Review Board of the Centro Protesi Inail (protocol: P6 2013).
2.2. Prosthetic Devices
The tri-digital prosthetic hand (MyoHand VariPlus, Ottobock—hereafter TD, left in Figure 1) is a standard mono-articulated myoelectric hand that allows the opposition grip. This configuration has been in use for the past 45 years and still is the standard of care [1]. All patients included in this study used the latest evolution of this type of hand, featuring a proportional control that allows for the modulation of hand speed.
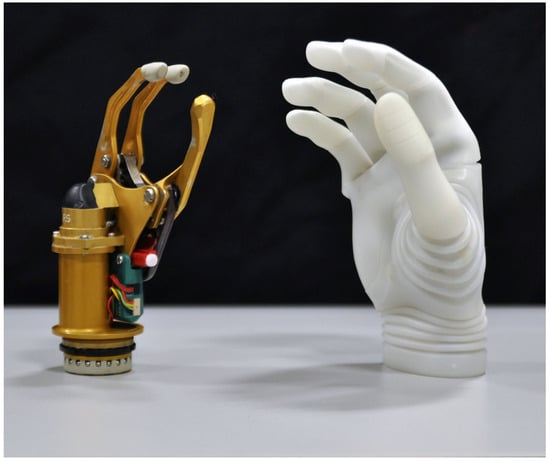
Figure 1.
Tri-digital prosthetic hand (MyoHand VariPlus, Ottobock) and poly-articulated hand (Michelangelo, Ottobock).
The poly-articulated hand (Michelangelo, Ottobock – hereafter M, right in Figure 1) is moved by using two electrodes and can perform seven grasping types. The opposition of the thumb ensures, in addition to the power and a tripod grasp, a lateral power grip. When not being used, the hand assumes a neutral position such as the human hand when relaxed. M is connected to a joint for the flexion–extension and pronation–supination movements. Both M and TD perform an “opposition grip”. However, the actual position of fingers in “opposition” is substantially different between the two prosthetic systems. The thumb position in TD is roughly parallel to the long axis of the forearm. On the contrary, the thumb in M is inclined at approximately 45° for the same long axis. In addition, when fully opened against a fixed surface, the thumb of M does not push the whole prosthesis upward as is the case with TD. TD’s opposition would be close to M’s opposition if the wrist in TD was flexed by 45°. The same word “opposition” identifies two visibly different postures in M and TD.
2.3. Study Design
All amputees used their prosthesis for more than 8h/day and had been using TD as a standard hand for at least 4 years by the time of enrollment. Following the subscription of informed consent, a motion analysis assessment was completed with TD. M was then fit, and a 5-day occupational therapy training program was completed. Subsequently, patients started using M as their primary prosthesis. After three months of home use, they completed a second motion analysis session with M. Finally, a third session with the sound side hand (S) was performed.
2.4. Activities
Within each session, the subjects performed four activities, starting from the same standardized reference position: seated on an adjustable chair with no armrests, in front of a height-adjustable table, with the knees flexed at 90°, wrists held on the edges of the table with the elbow flexed at 90°, hand closed. With the subject in the reference position, four areas (10 × 15 cm) were marked on the table and named ‘A0’, ‘A1’, ‘A2’, and ‘A3’ (Figure 2):
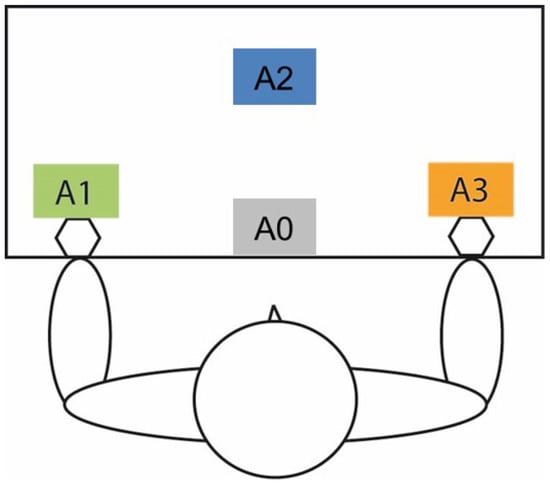
Figure 2.
Position of the standardized areas A0–A3 concerning the patient. A1 is in front of the hand under assessment, while A3 is in front of the contralateral side.
- A0—in front of the subject, aligned with the table edge, closest to the subject;
- A1—in front of the prosthetic hand;
- A2—in front of the subject trunk, at the maximum reachable distance of the arm under investigation, without moving the thorax;
- A3—in front of the sound side.
During each session, the subjects performed four standardized activities intended to elicit different grasps, three times each:
- 1.
- Fine manipulation:
- (a)
- Disk12: Starting at the resting position, (I) picked up a disk from A1; (II) move it to A2; (III) and return to the resting position; then, (IV) pick up the disk from A2, (V) move it to A1 and (VI) return to the resting position (six phases). The disk (3.7 cm × 1.7 cm) is the one used in the Minnesota Manual Dexterity Test (Lafayette Instrument Company, 1969). This task forces the subject to control the hand grasping in front of the body;
- (b)
- Disk13: as in Disk12, but using A3 instead of A2, to force the subject to control the hand grasping while the arm is on the opposite side of the body;
- 2.
- Power grip:
- (a)
- Jar: similar to Disk12, but moving an empty jar between locations A0 and A2. The jar is the one included in the SHAP kit [15];
- 3.
- Lateral grip:
- (a)
- Plate: a box (height 8.5 cm) is positioned on A2. A plate (diameter 22 cm, height 2 cm) is positioned on top of the box, protruding by 4.5 cm. A 0.5 kg plastic bottle is placed horizontally on the plate, free to move. The subject is instructed to carry the plate from A2 to A0 and back, preventing the bottle falling down.
2.5. Biomechanical Model and Motion Analysis Measures
The motion analysis protocol was defined and is described herein, following the recommendations reported in [16].
2.5.1. Segment and Angles of Interest
Since this study aimed to analyze compensatory movements, the attention was primarily focused on the thorax orientation relative to the global frame (also referred to as trunk kinematics), and on the orientation of the shoulder girdle, scapula and humerus relative to the thorax. For an improved tracking of humerus motion, the forearm’s long axis was also tracked.
The global frame was aligned with the table edges. The anatomical coordinate systems (Table 1) for the thorax, scapula and humerus followed the ISG/ISB standard [17]); the definition for the shoulder girdle followed [18].

Table 1.
Anatomical coordinate systems.
Segment angles were obtained from the relative orientation of the anatomical frames, using Euler decomposition, as described in Table 2.

Table 2.
Sequence of Euler angles for each joint/segment kinematics of interest.
2.5.2. Marker-Set and Calibration Trials
Data were captured through an optoelectronic system (Vicon Motion Systems, Vicon, UK) at 100 frames/second. To track the anatomical landmarks required by the anatomical frames, a CAST-like approach was used. Clusters of 4 markers were positioned on the thorax (on its 4 anatomical landmarks), on a 3D-printed acromion cluster and elastic bands wrapped around the humerus and forearm (Figure 3) [19,20]. Moreover, 2 markers were placed on the index and thumb, and one marker was positioned on each of the objects to detect the beginning/end of each activity and its phases. Three markers were placed on the palm but were not used for data processing.
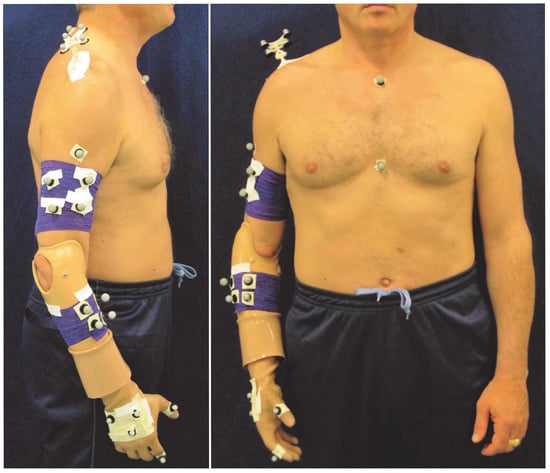
Figure 3.
Marker-set used with the Vicon system for measuring upper-limb kinematics. The same marker set was used for the sound side, but the forearm cluster was placed distally, just above the wrist.
Once the marker set was set-up on the subject, anatomical landmark calibrations were completed using a pointer with three markers at a known distance [21]. For the prosthetic side, EL and EM were identified by palpation during a static trial after removing the prosthesis. RS and US were palpated on the socket at opposite sides, to replicate the anatomical standard. In addition, subjects were asked to complete an upper-arm circumduction with a maximum elevation of 45°. This task was subsequently used to estimate the position of the center of the glenohumeral head in the acromion cluster frame using the functional method of Gamage and Lasenby [22].
2.6. Data Processing
For each hand (TD, M and S) and activity, data processing was completed at the subject- and group-level.
At the subject-level, Woltring filtering was applied to the trajectory data. Then, joint angles were calculated. Based on the hand/objects relative position and video recordings, each activity repetition was identified and further segmented into 6 phases (as described in Section “Activities”). The total time taken to complete each of the three repetitions was noted and their median duration was extracted and saved for the group-level analysis. Subsequently, each phase was time normalized as suggested in [23], assuming 100 samples for the whole repetition. Finally, for each joint angle, a median curve over the repetitions was calculated, and the peak value of this median curve was saved for the group-level analysis.
At the group-level, the group median curve was extracted from the median curves of the 6 subjects (Figure 4). Similarly, a group median value was extracted for the time to complete the activity, and for the peak value of each joint angle.
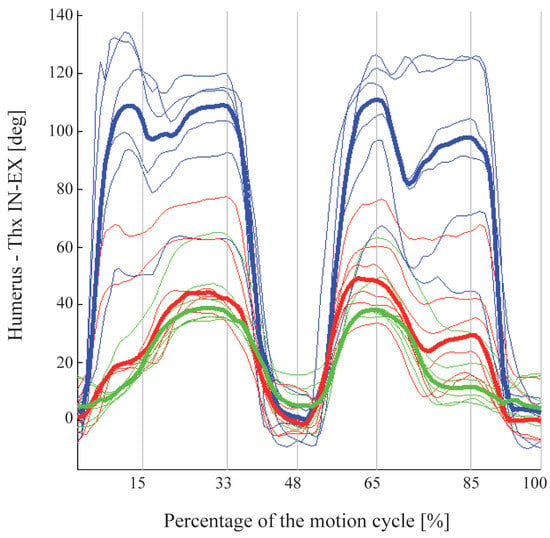
Figure 4.
Example of the dataset available for a single joint angle. Blue lines refer to TD, red to M and green to S. For each hand, thin lines are the median curves of the six subjects, while the thick line is the group median. The motion cycle is reported in percentage from the start to the end of the movement. In addition, the six sub-phases of the movements were identified and normalized based on Vicon and video recordings.
2.7. Statistical Analysis and Hypotheses
Firstly, an analysis was performed to identify statistically significant differences among hands. Then, a second analysis was applied to select the differences in potential clinical interest among the statistically relevant ones. In this work, the following two hypotheses were formulated:
- 1.
- TD leads to clinically relevant alterations in shoulder and trunk kinematics when compared to S, extending over 1/3 of the duration of the motion cycle;
- 2.
- M decreases the alterations compared to TD, both in magnitude and extension over time, thus closing the gap between the sound and the prosthetic side.
2.7.1. Statistically Relevant Differences
The analysis was completed independently for each activity. Firstly, the median duration among S, TD and M was assessed to understand the statistical differences using the Friedman test and post hoc comparisons “TD vs. S”, “M vs. S” and “TD vs. M” (significance level = 0.05). The Mann–Whitney U test was used given the small sample size. With the same approach, each joint angle was also tested to determine whether:
- 1.
- The median peak values were different among hands;
- 2.
- The median curves were different among the hands, running the analysis at each percentage of the motion cycle (herein “sample”).
2.7.2. Clinically Relevant Difference
Samples can feature angles with a statistically significant difference between two hands (briefly “statistically significant samples”), but still differences might not be “large enough” to be of clinical interest [24]. A combination of three criteria or “filters” was assumed to identify the samples of possible clinical relevance for each joint angle (“clinically relevant samples” in short). The filters on the statistically relevant sample are presented for the general comparison of HandA vs. HandB, considering the median curve of each hand:
- 1.
- “Three-in-a-row”: Only samples grouped in 3 or more were considered; this condition filters isolated samples;
- 2.
- “Minimal required movement”: a sample is discarded if both the angles for HandA and HandB are below the 30% of the maximum value of S for that joint angle (threshold); this condition filters samples featuring an overall limited joint excursion;
- 3.
- “Minimum difference”: a sample is discarded if the angle for HandA is within ±30% of the value of HandB; this filters differences that appear too small to be potentially relevant. For instance, given a sample in which the value for HandB is 20°, differences in the angle of HandA falling between 14° and 26° are considered irrelevant, despite a pre-classification as statistically significant.
After applying the three filters, the percentage of samples with clinically relevant differences was counted, and the following coding was assumed to quantify the “exposure to the altered kinematics”, possibly leading to an increased risk of injury:
- 1.
- Red: when differences extend for over 41% of the movement;
- 2.
- Orange: from 11 to 40%;
- 3.
- Yellow: from 1 to 10%;
- 4.
- Green: 0%.
Conditions were “summed up” to gain a total score, by assigning 3 points to the red condition, 2 to orange and 1 to yellow.
A clinical filter was also applied to the statistical differences between the median peak values: a minimal difference of 30% was set for this purpose.
3. Results
3.1. Participants
Six transradial amputee volunteers were recruited (Table 3). The participants’ median age was 47 years (range 35 ÷ 65) and the median time since amputation was 15 years (range 4.5 ÷ 48.0). Three of them reported phantom limb sensation and pain experiences which did not affect prosthesis use.

Table 3.
Characteristics of the selected sample. All patients were right-side dominant.
3.2. Clinical Differences in Joint Kinematics and Exposure to the Altered Kinematics
- Disk12
As shown in Figure 5 and Figure 6, the use of TD leads to relevant alterations of shoulder kinematics compared to S. The shoulder is in subacromial impingement position, with the humerus in forward flexion (90° vs. 60°) and internal rotation (approximately 110° vs. 40°), the scapula rotated laterally (22° vs. 8°) the girdle highly elevated (16° vs. 2.5°). This is a position of high stress for the shoulder complex. Alterations extend to trunk kinematics, in particular to AB-AD (20° vs. 2.5°), stressing the spine.
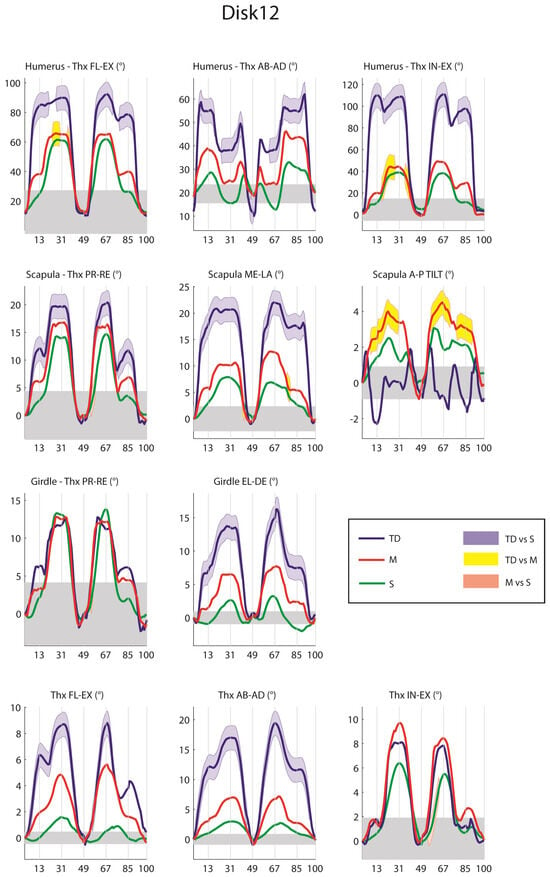
Figure 5.
Joint kinematics for Disk12, from distal to proximal. The median values of TD (blue line), M (red line) and S (green line) are reported, as well as the differences in potential clinical interest between them, illustrated as shaded areas following the median curves: blue for TD vs. S, yellow for M vs. S and magenta for M vs. S. The gray band represents the minimal movement required (30% of maximal value of S).
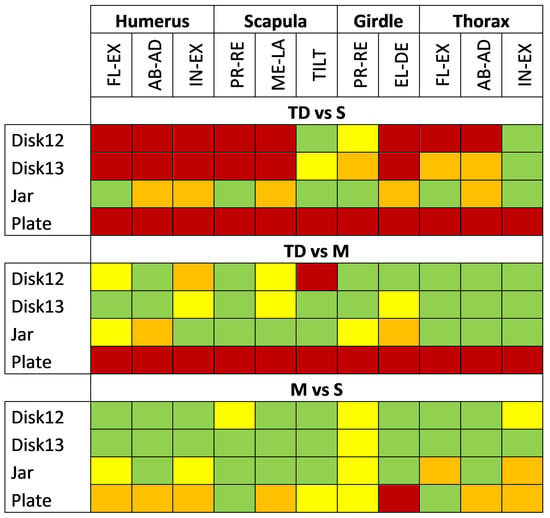
Figure 6.
For each pairwise comparison (TD vs. S, TD vs. M and M vs. S), the table summarizes the “exposure to the altered kinematics” considering each activity and joint angle. Red condition: when clinically relevant samples are over the 41% of the motion cycle; orange: from 11 to 40%; yellow: from 1 to 10%; green: 0%.
S and M have no abnormal values for humerus FL-EX and IE, and the shoulder is far away from any impingement position. The only differences between the two hands were reported for scapula and girdle PR-RE and thorax IE, but they are due to a different steepness of the curves, ending in almost identical ROMs (2° difference), with potentially no detrimental effect.
The differences between TD and M are concentrated in the area of the subacromial impingement position, with substantial improvements in favor of M (humerus FL-EX, IN-EX, scapula ME-LA). A difference was also reported for scapula TILT, but limited to 5° with a position of the scapula that is away from known impingement positions. The percentage of the motion cycle (Figure 6) where there are differences between M and S (0 reds, 3 yellows) is substantially smaller than that for TD vs. S (8 reds and 1 yellow). Of notice, M leads to reductions in the compensatory movement, despite the grip used by the patient: indeed, three patients opted for opposition and three for lateral grip.
- Disk13
Overall, the differences in the kinematics for the Disk13 confirm the trend shown in Disk12 with a subacromial impingement position only for TD (see Supplementary Material). As reported in Figure 6, alterations in TD vs. S sum up to 6 red, 3 orange and 1 yellow levels of exposure, which reduce for M vs. S to just 1 yellow. Improvements exist for M compared to TD with 3 yellows, concentrated in important angles for shoulder impingement, namely humerus IN-EX, scapula ME-LA and girdle EL-DE.
- Jar
The jar task shows the least amount of clinical differences throughout all the tasks and is not related to shoulder impingement (see Supplementary Materials). Noticeably, the differences between TD and M or S are mostly due to a more adducted and externally rotated humerus while approaching or releasing the jar. At the same time, scapula ME-LA and girdle EL-DE are increased. This combination of factors is probably needed to orient the relatively small opening grip of TD (9 cm) toward the jar, avoiding the thumb to impinge the jar itself. The increased thorax FL-EX with M might serve the same purpose but appears to be a more natural approach.
Exposure to altered kinematics is higher for TD compared to S (5 orange) and reduces for M vs. S (2 orange and 3 yellow).
- Plate
Five out of six subjects were unable to complete the plate task with TD. Therefore, only M and S are compared with each other (see Supplementary Material). Due to the different approach to the plate with M, girdle EL-DE is highly increased, and ME-LA follows: the lack of wrist radio-ulnar deviation requires an increased overall shoulder elevation to approach the plate with a horizontal thumb. The different approach is confirmed by Figure 6.
3.3. Overall Differences among Tasks
Table 4 summarizes the exposure to the altered kinematics. TD vs. S presents 25 red conditions, which drop to 1 red for M vs. S. Furthermore, TD vs. M features improvements toward M with 12 red. The total score shows TD vs. S = 93 points, TD vs. M = 49 and M vs. S = 28. M is thus closing the gap between the sound and the prosthetics side kinematics.

Table 4.
Counting the red, orange, yellow and green conditions reported in Figure 6 for each pairwise comparison between hands.
3.4. Peak-to-Peak Differences
The clinically relevant peak-to-peak differences are reported in Figure 7. Among the 22 reported values, 16 concentrate in TD vs. S. For activities Disk12 and Disk13, differences reach 30° and 73° for the humerus AB-AD and IE, 16° and 13° for scapula ME-LA and girdle EL-DE and 18° for thorax AB-AD, indicating the level of deviation.
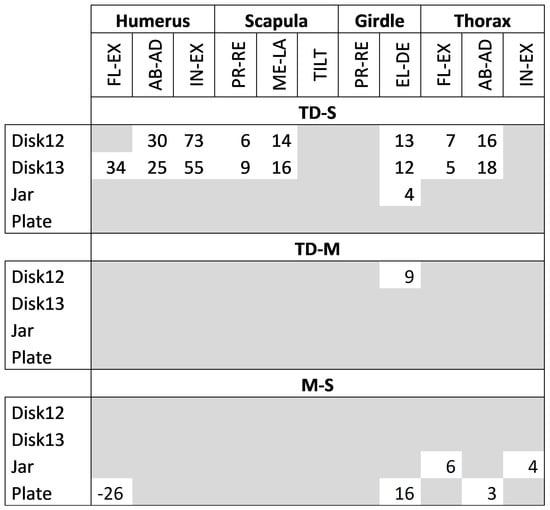
Figure 7.
Peak-to-peak differences between hands, passing the tests of statistical significance and possible clinical relevance.
For M vs. S, differences are limited to the jar and plate activities and concentrate on the trunk to ease the approach to the object (with maximum deviations of 6° for FL-EX), and EL-DE in the girdle, which is needed to complete the activity in absence of the wrist deviation, as discussed previously.
3.5. Duration of the Activities
The duration analysis did not show any significant improvement between TD and M: differences between hands were within 2 s at most, with durations for S being typically 4 s shorter (40% of the total time). The exception was the plate activity, where the difference in the median was within 2 s. S was significantly quicker than TS for Disk12, Disk13 and Jar, while it was quicker than M for Disk13 and Jar (see Supplementary Materials).
4. Discussion
This work aimed to report, for the first time, the kinematic differences in the shoulder (scapula, shoulder girdle and humerus) and trunk of unilateral transradial patients performing the same set of activities with a standard myoelectric hand (TD), a multi-articulated myoelectric hand (M) and the sound side (S).
The results support the hypothesis that TD has led to clinically relevant alterations in shoulder and trunk kinematics when compared to S, extending over 1/3 of the motion cycle. During Disk12 and Disk13, amputees were forced in the subacromial impingement position, with alterations extending over 40% of the motion cycle for most joint angles (14 red conditions over 22). Moreover, peak-to-peak differences reached 73° for humerus IE and 16° and 13° for scapula ME-LA and girdle EL-DE. These results describe the stressful condition of the shoulder during these activities. Alterations also exist during the jar activity, with the shoulder adducted, externally rotated and elevated, and the plate task was impossible to complete for 5 out of 6 subjects.
The common reason for all these alterations was the specific position of the thumb in TD, which is parallel to the long axis of the forearm as illustrated in Figure 1, in combination with the absence of wrist flexion. This statement is supported by the results for M, which presents an opposition grip with the long fingers perpendicular to the palm and the thumb inclined to 45°, i.e., similarly to a TD with the flexed wrist. This different opposition grip, combined with the lateral grip, allows patients to substantially reduce differences compared to S during all activities, avoiding the subacromial impingement position: Red cells in Figure 6 drop from 25 with TD to 1 with M. Moreover, no significant peak-to-peak differences are reported for the humerus and scapula. The activity still presenting differences is plate, completed by all subjects but with relevant compensatory movements elevating the shoulder while approaching the plate, substituting for the lack of wrist radio-ulnar deviation. However, advantages in kinematics do not translate into an increased speed in completing the activities. Durations are still larger with the prosthetic side by almost 40%.
These results confirm the validity of the second hypothesis, i.e., that M decreases the alterations compared to TD, both in extension and magnitude, closing the gap between the sound and the prosthetic side. However, M does not still replicate S.
The literature on compensatory movements in upper-limb amputees is limited and diverges in terms of performed tasks, motion analysis protocols and the reporting of data [7,8,25]. No previous results are available regarding scapula and shoulder girdle movements, particularly with respect to a within-subject analysis of transradial amputees using both mono-articulated and poly-articulated myoelectric hands. However, the results of this work support previous conclusions on the increased shoulder AB-AD and trunk compensatory movements, in all degrees of freedom but mostly AB-AD and FL-EE, which can potentially increase the metabolic cost, fatigue and back pain [6,8,13].
The present study has limitations. The most relevant is the limited number of subjects, due to the cost of the prosthetic components. Results should therefore be viewed as indications, to be confirmed over a larger study.
5. Conclusions
The results indicate an increase in the risk of injury of the rotator cuff using a standard mono-articulated myoelectric hand forcing amputees into a subacromial impingement position during relatively simple manipulation activities. Moreover, the position of the thumb requires further compensatory movements at the humerus, scapula and girdle and trunk during reaching activities, which may lead to an increase in fatigue and may contribute to the further degradation of physical performance and further injury. For the same reason, simple activities such as picking up a plate while seated are impossible for 5/6 subjects. The availability of a poly-articulated myoelectric hand allows all amputees to complete this activity and avoid the subacromial impingement position during reaching and grasping due to lateral grip and/or thumb alignment in opposition. Despite the limited number of subjects due to the cost of the prosthetic components, the results are promising. Indeed, tri-digital vs. sound hand scored 93 points, tri-digital vs. poly-articulated hands scored 49 and poly-articulated vs. sound hand scored 28—demonstrating that the poly-articulated hand enhances shoulder and trunk kinematics. These results could help develop rehabilitation techniques for individuals who cannot have a poly-articulated hand, helping them perform certain actions with specific strategies. Furthermore, they could provide input to design and control a prosthetic wrist with more degrees of freedom to further decrease compensatory movements.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/prosthesis5010014/s1, Figure S1: Kinematics for the task Disk13; Figure S2: Kinematics for the task Jar; Figure S3: Kinematics for the task Plate; Figure S4: Results for the duration of movement.
Author Contributions
A.G.C. designed the paper, analyzed the literature, performed the experiments, acquired and analyzed the experimental data and wrote the paper; C.G. and F.M. designed the paper, supervised the writing and wrote the paper; L.D.M. wrote and reviewed the paper; E.G. and G.T. supervised the writing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted following the Declaration of Helsinki and was approved by the Institutional Review Board of the Centro Protesi Inail (protocol: P6 2013), approval date: 14 November 2012.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
This work was supported by the Italian Institute for Labour Accidents (Inail) with PR19-PAS-P1 project.
Conflicts of Interest
The authors declare no conflict of interest. The founders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Sample Availability
Not applicable.
Abbreviations
List of abbreviations:
| TD | Tri-digital myoelectric hand |
| M | Michelangelo hand–wrist system |
| S | Sound-side hand |
| FL-EX | Flexion–extension angle |
| AB-AD | Abduction–adduction angle |
| IN-EX | Internal–external rotation |
| ME-LA | Medio-lateral rotation of the scapula |
| TILT | Posterior–anterior tilting of the scapula |
| EL-DE | Elevation–depression angle |
| PR-RE | Protraction–retraction (applies to scapula and shoulder girdle) |
References
- Gentile, C.; Cordella, F.; Zollo, L. Hierarchical Human-Inspired Control Strategies for Prosthetic Hands. Sensors 2022, 22, 2521. [Google Scholar] [CrossRef]
- Resnik, L.; Borgia, M. Reliability, validity, and responsiveness of the QuickDASH in patients with upper limb amputation. Arch. Phys. Med. Rehabil. 2015, 96, 1676–1683. [Google Scholar] [CrossRef]
- Scott, R.N.; Parker, P.A. Myoelectric prostheses: State of the art. J. Med. Eng. Technol. 1988, 12, 143–151. [Google Scholar] [CrossRef]
- Markovic, M.; Schweisfurth, M.A.; Engels, L.F.; Farina, D.; Dosen, S. Myocontrol is closed-loop control: Incidental feedback is sufficient for scaling the prosthesis force in routine grasping. J. Neuroeng. Rehabil. 2018, 15, 81. [Google Scholar] [CrossRef]
- Metzger, A.J.; Dromerick, A.W.; Holley, R.J.; Lum, P.S. Characterization of compensatory trunk movements during prosthetic upper limb reaching tasks. Arch. Phys. Med. Rehabil. 2012, 93, 2029–2034. [Google Scholar] [CrossRef]
- Valevicius, A.M.; Boser, Q.A.; Chapman, C.S.; Pilarski, P.M.; Vette, A.H.; Hebert, J.S. Compensatory strategies of body-powered prosthesis users reveal primary reliance on trunk motion and relation to skill level. Clin. Biomech. 2020, 72, 122–129. [Google Scholar] [CrossRef]
- Carey, S.L.; Highsmith, M.J.; Maitland, M.E.; Dubey, R.V. Compensatory movements of transradial prosthesis users during common tasks. Clin. Biomech. 2008, 23, 1128–1135. [Google Scholar] [CrossRef]
- Major, M.J.; Stine, R.L.; Heckathorne, C.W.; Fatone, S.; Gard, S.A. Comparison of range-of-motion and variability in upper body movements between transradial prosthesis users and able-bodied controls when executing goal-oriented tasks. J. Neuroeng. Rehabil. 2014, 11, 1–10. [Google Scholar] [CrossRef]
- Greitemann, B.; Güth, V.; Baumgartner, R. Asymmetry of posture and truncal musculature following unilateral arm amputation—A clinical, electromyographic, posture analytical and photogrammetric study. Z. Orthop. Grenzgeb. 1996, 134, 498–510. [Google Scholar] [CrossRef]
- Jones, L.; Davidson, J. Save that arm: A study of problems in the remaining arm of unilateral upper limb amputees. Prosthetics Orthot. Int. 1999, 23, 55–58. [Google Scholar] [CrossRef]
- Flood, K.M.; Huang, M.E.; Roberts, T.L.; Pasquina, P.F.; Nelson, V.S.; Bryant, P.R. Limb deficiency and prosthetic management. 2. Aging with limb loss. Arch. Phys. Med. Rehabil. 2006, 87, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Postema, S.G.; Bongers, R.M.; Brouwers, M.A.; Burger, H.; Norling-Hermansson, L.M.; Reneman, M.F.; Dijkstra, P.U.; Van der Sluis, C.K. Musculoskeletal complaints in transverse upper limb reduction deficiency and amputation in the Netherlands: Prevalence, predictors, and effect on health. Arch. Phys. Med. Rehabil. 2016, 97, 1137–1145. [Google Scholar] [CrossRef]
- Engdahl, S.M.; Lee, C.; Gates, D.H. A comparison of compensatory movements between body-powered and myoelectric prosthesis users during activities of daily living. Clin. Biomech. 2022, 97, 105713. [Google Scholar] [CrossRef]
- Luchetti, M.; Cutti, A.G.; Verni, G.; Sacchetti, R.; Rossi, N. Impact of Michelangelo prosthetic hand: Findings from a crossover longitudinal study. J. Rehabil. Res. Dev. 2015, 52, 605–618. [Google Scholar] [CrossRef]
- Light, C.M.; Chappell, P.H.; Kyberd, P.J. Establishing a standardized clinical assessment tool of pathologic and prosthetic hand function: Normative data, reliability, and validity. Arch. Phys. Med. Rehabil. 2002, 83, 776–783. [Google Scholar] [CrossRef] [PubMed]
- Kontaxis, A.; Cutti, A.G.; Johnson, G.R.; Veeger, H. A framework for the definition of standardized protocols for measuring upper-extremity kinematics. Clin. Biomech. 2009, 24, 246–253. [Google Scholar] [CrossRef]
- Wu, G.; Van der Helm, F.C.; Veeger, H.D.; Makhsous, M.; Van Roy, P.; Anglin, C.; Nagels, J.; Karduna, A.R.; McQuade, K.; Wang, X.; et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion—Part II: Shoulder, elbow, wrist and hand. J. Biomech. 2005, 38, 981–992. [Google Scholar] [CrossRef] [PubMed]
- Garofalo, P.; Cutti, A.G.; Filippi, M.V.; Cavazza, S.; Ferrari, A.; Cappello, A.; Davalli, A. Inter-operator reliability and prediction bands of a novel protocol to measure the coordinated movements of shoulder-girdle and humerus in clinical settings. Med. Biol. Eng. Comput. 2009, 47, 475–486. [Google Scholar] [CrossRef]
- Duprey, S.; Billuart, F.; Sah, S.; Ohl, X.; Robert, T.; Skalli, W.; Wang, X. Three-dimensional rotations of the scapula during arm abduction: Evaluation of the acromion marker cluster method in comparison with a model-based approach using biplanar radiograph images. J. Appl. Biomech. 2015, 31, 396–402. [Google Scholar] [CrossRef]
- Lempereur, M.; Brochard, S.; Leboeuf, F.; Rémy-Néris, O. Validity and reliability of 3D marker based scapular motion analysis: A systematic review. J. Biomech. 2014, 47, 2219–2230. [Google Scholar] [CrossRef]
- Cutti, A.G.; Paolini, G.; Troncossi, M.; Cappello, A.; Davalli, A. Soft tissue artefact assessment in humeral axial rotation. Gait Posture 2005, 21, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Gamage, S.S.H.U.; Lasenby, J. New least squares solutions for estimating the average centre of rotation and the axis of rotation. J. Biomech. 2002, 35, 87–93. [Google Scholar] [CrossRef]
- Stergiou, N. Innovative Analyses of Human Movement: Analytical Tools for Human Movement Research; Human Kinetics: Champaign, IL, USA, 2004; Available online: https://ccd.ucam.edu/index.php/revista/article/view/272 (accessed on 27 December 2022).
- Hayat, M.J. Understanding statistical significance. Nurs. Res. 2010, 59, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Bertels, T.; Schmalz, T.; Ludwigs, E. Objectifying the functional advantages of prosthetic wrist flexion. JPO J. Prosthetics Orthot. 2009, 21, 74–78. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).