Conceptualization of an Anthropomorphic Replacement Hand with a Sensory Feedback System
Abstract
1. Introduction
2. Materials and Methods
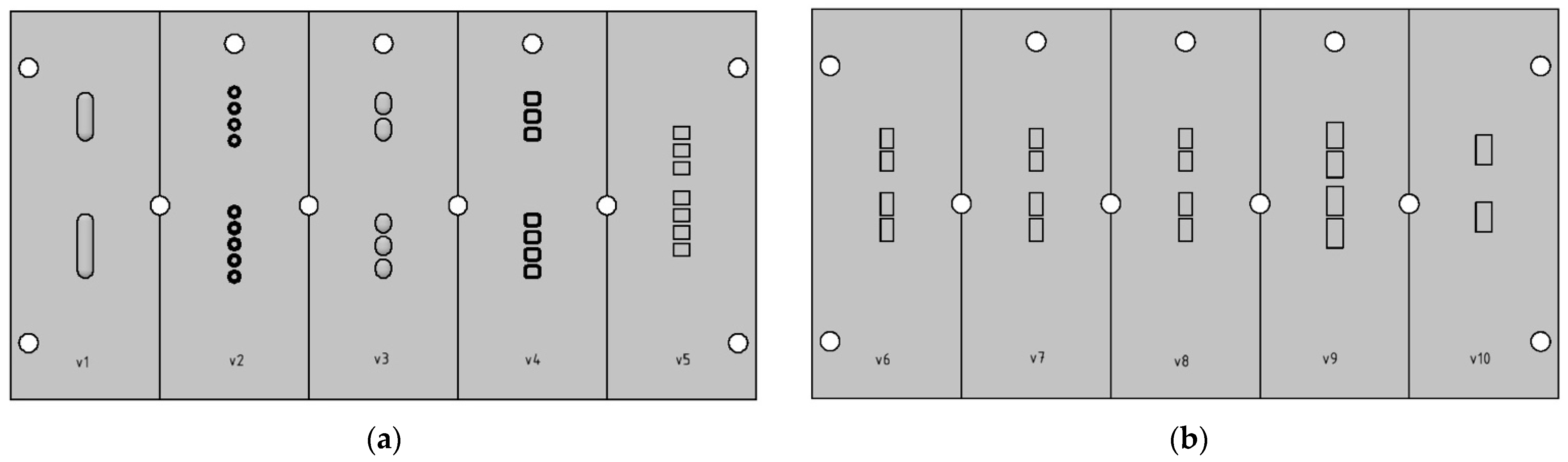
2.1. Finger Test Series I
- Two differently sized slotted holes (Figure 1a, v1);
- Four (distal) resp. five (proximal) cylinders (Figure 1a, v2);
- Two (distal) resp. three (proximal) ellipses (Figure 1a, v3);
- Three (distal) resp. four (proximal) rectangles with rounded edges (Figure 1a, v4);
- Three (distal) resp. four (proximal) rectangles (Figure 1a, v5).
2.2. Finger Test Series II
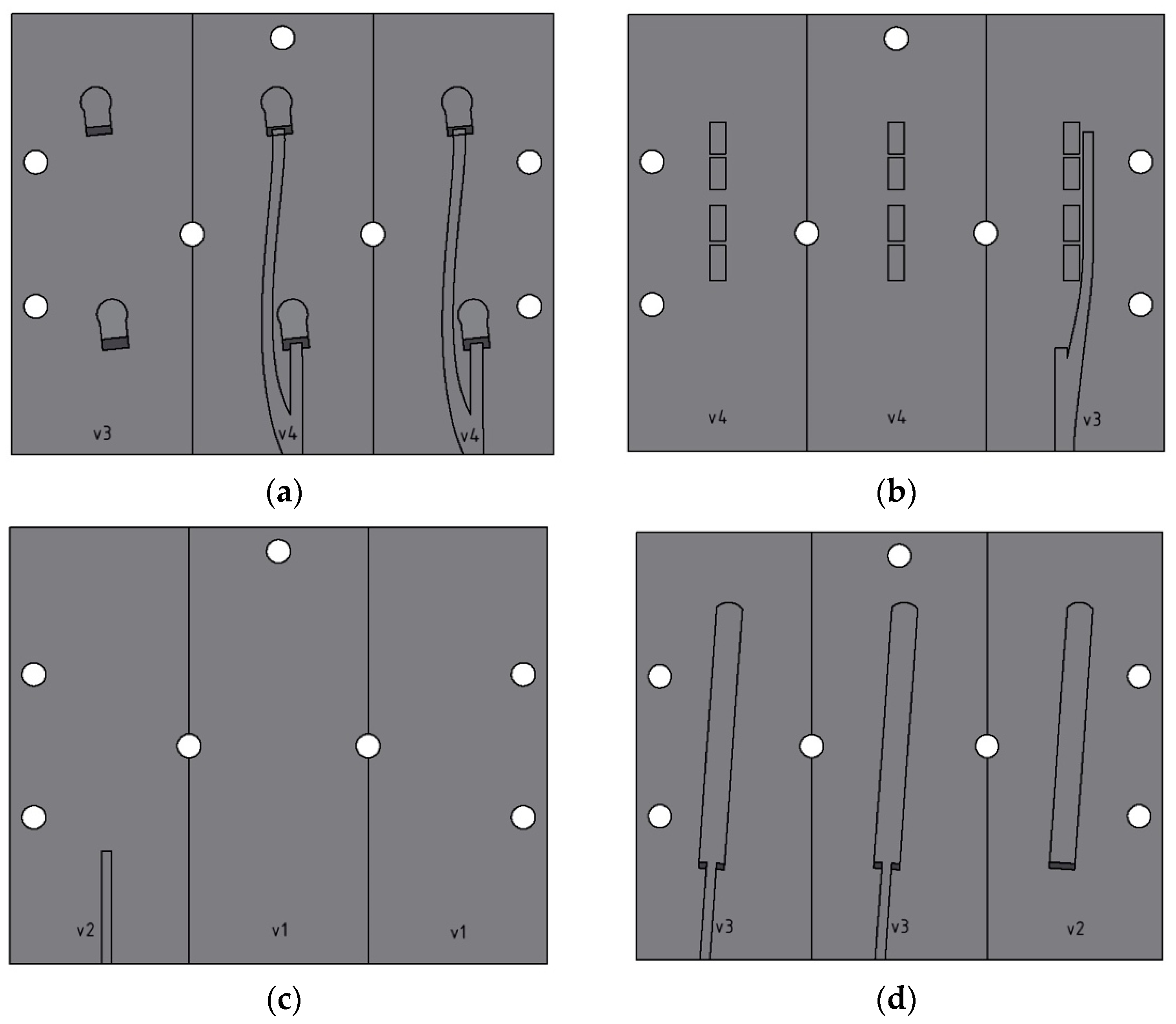
2.3. Finger Test Series III
2.4. Finger Test Series IV
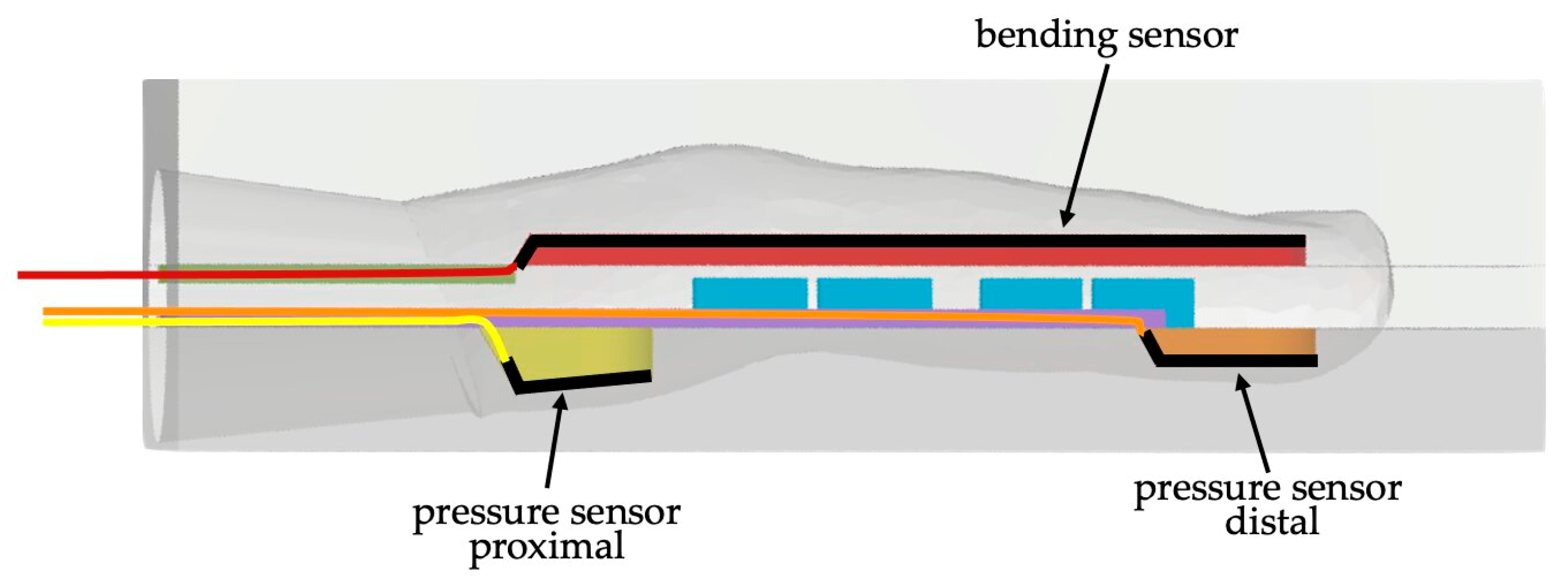
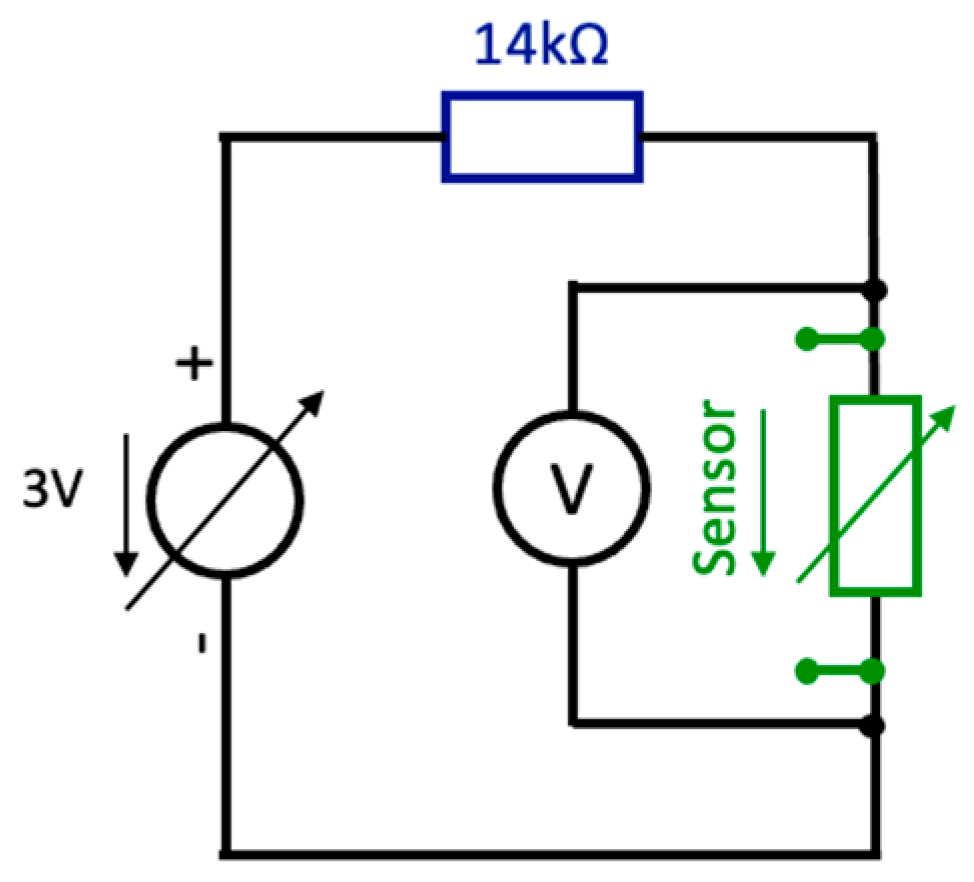
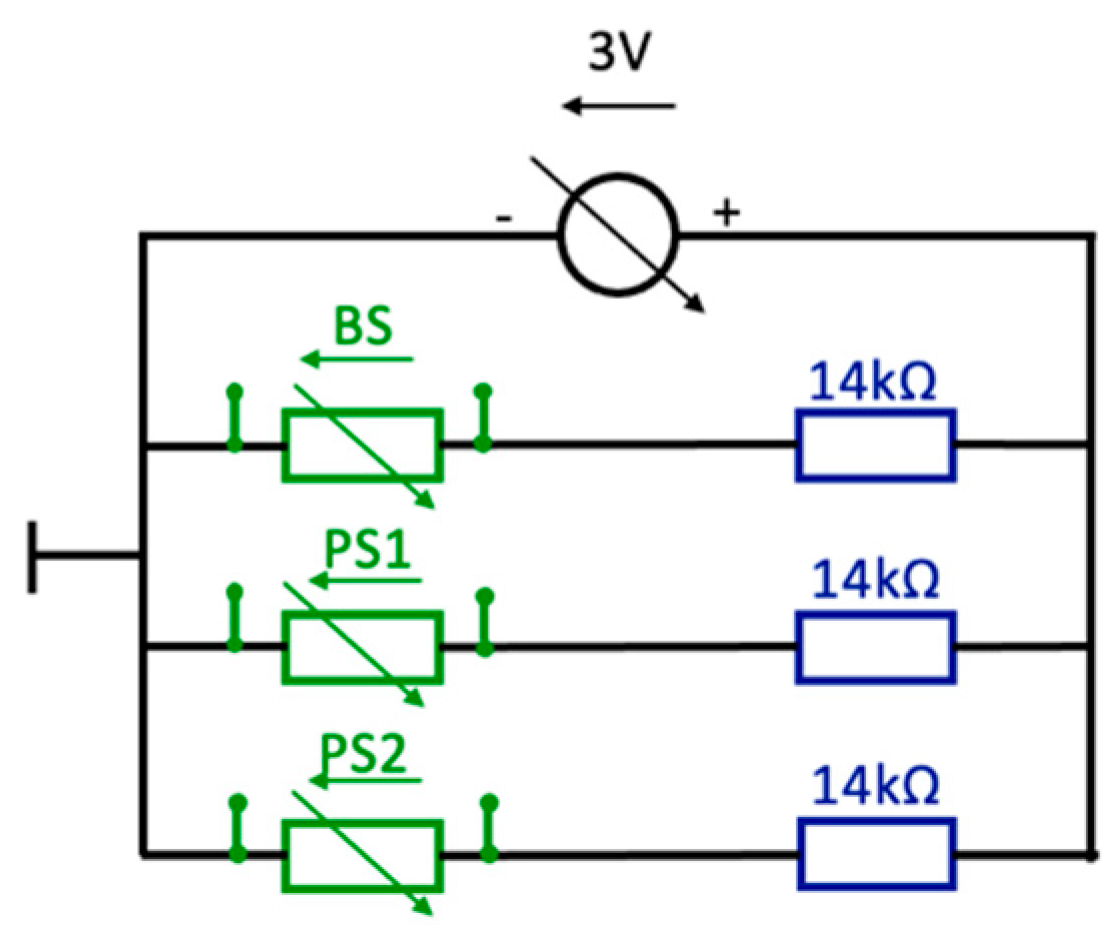
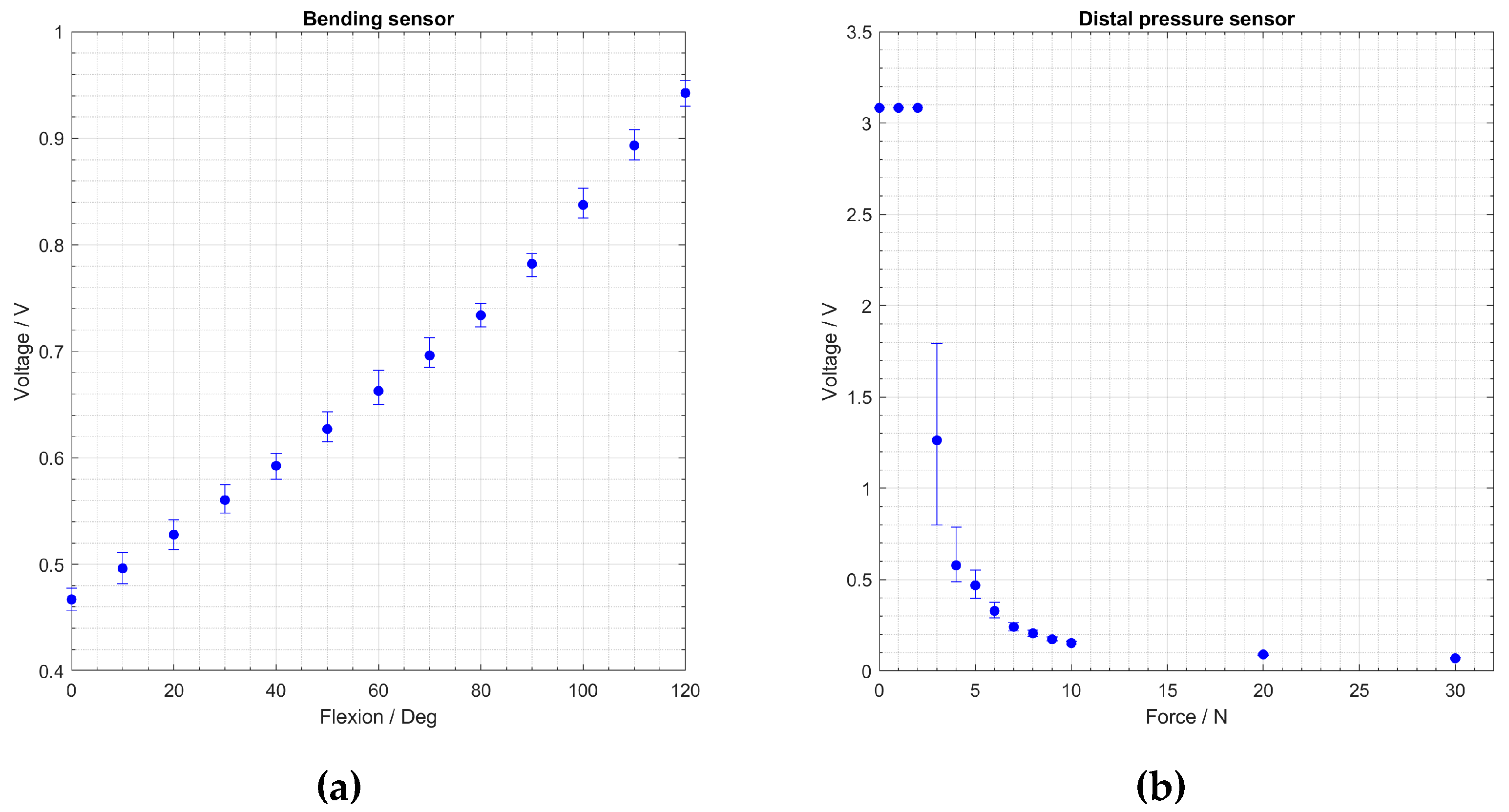
2.5. Evaluation of Molded Pressure and Bending Sensors
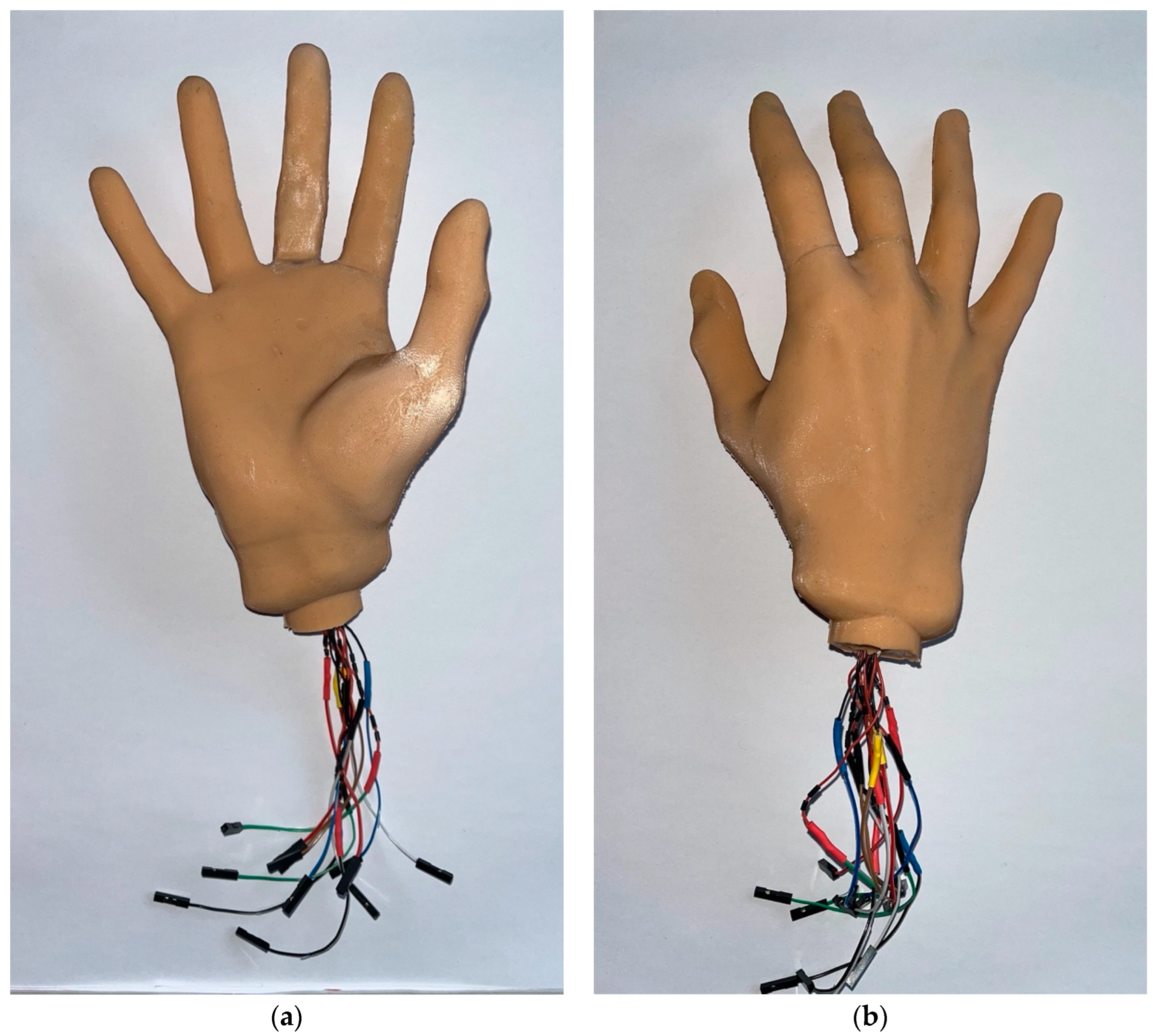
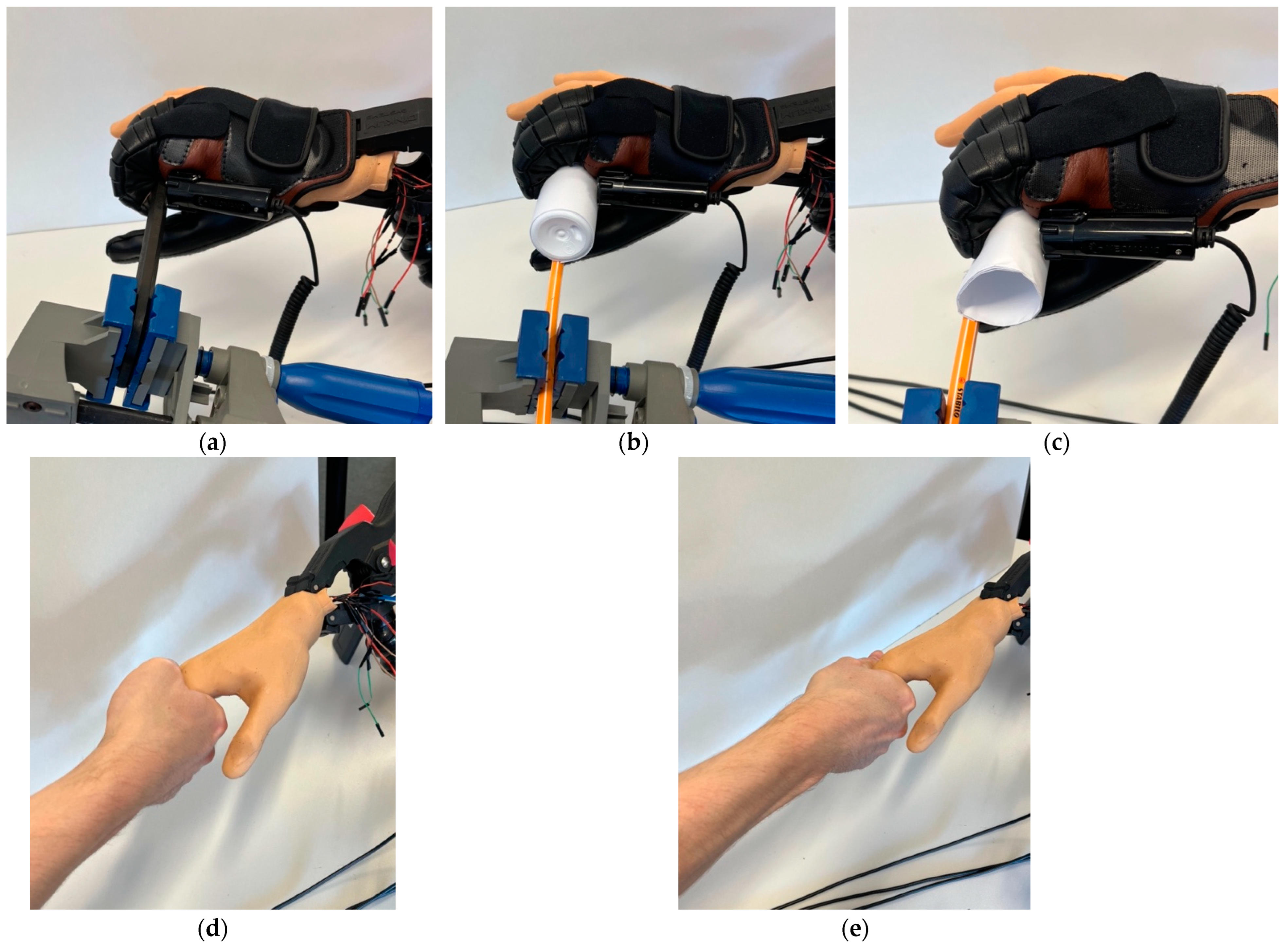
2.6. Final Replacement Hand
3. Results
3.1. Finger Test Series I
3.2. Finger Test Series II
3.3. Finger Test Series III
3.4. Finger Test Series IV
3.5. Evaluation of Molded Pressure and Bending Sensors
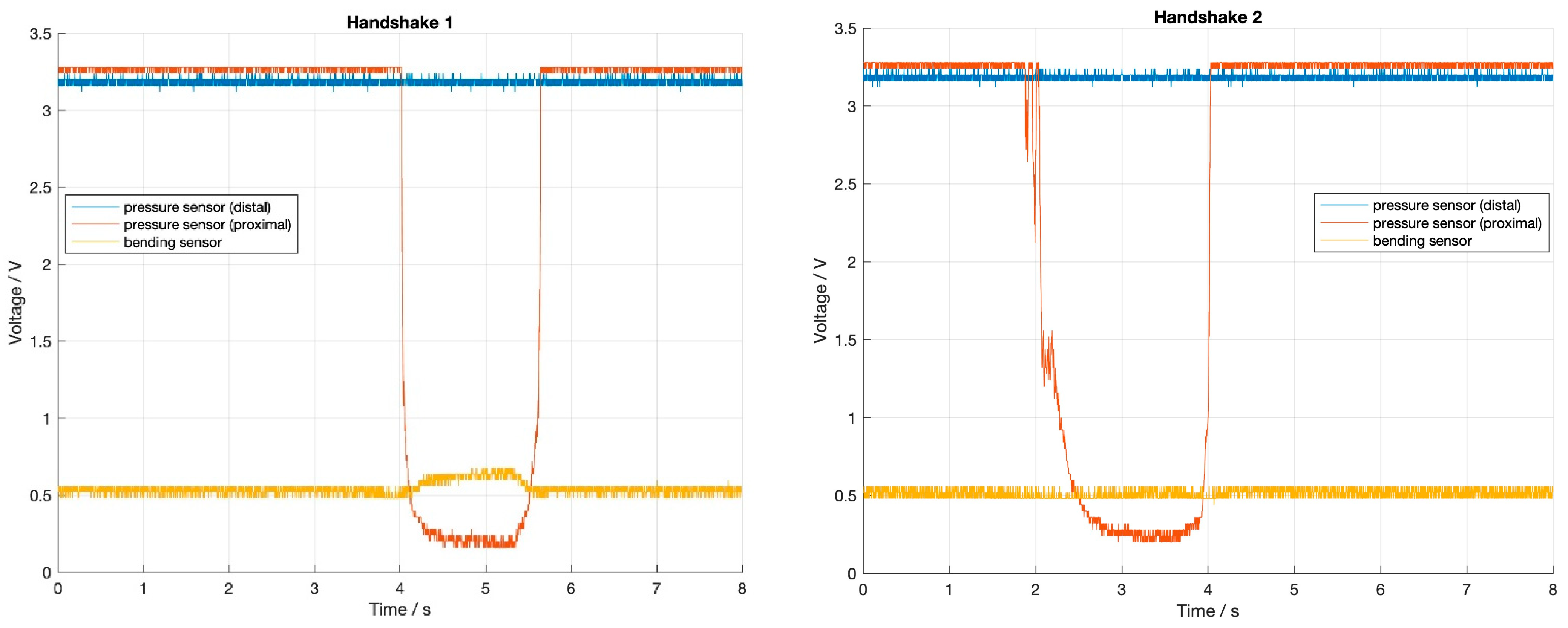
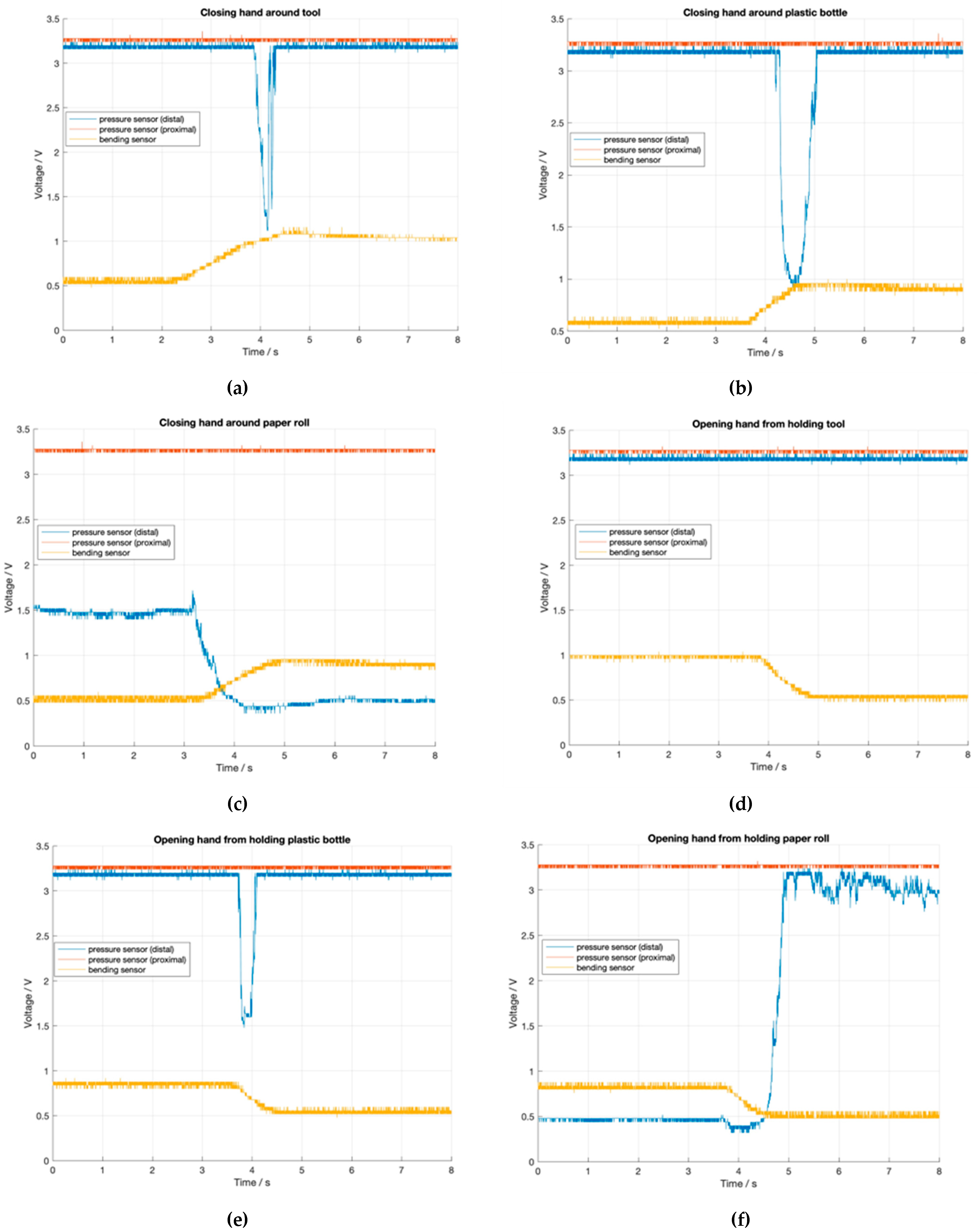
3.6. Final Replacement Hand
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siotos, C.; Ibrahim, Z.; Bai, J.; Payne, R.M.; Seal, S.M.; Lifchez, S.D.; Hyder, A.A. Hand Injuries in Low- and Middle-Income Countries: Systematic Review of Existing Literature and Call for Greater Attention. Public Health 2018, 162, 135–146. [Google Scholar] [CrossRef] [PubMed]
- Imbinto, I.; Peccia, C.; Controzzi, M.; Cutti, A.G.; Davalli, A.; Sacchetti, R.; Cipriani, C. Treatment of the Partial Hand Amputation: An Engineering Perspective. IEEE Rev. Biomed. Eng. 2016, 9, 32–48. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.M.; Powell, J.E.; Lacey, S.A.; Butkus, J.A.; Smith, D.G. Current and Emerging Prostheses for Partial Hand Amputation: A Narrative Review. PM R. 2022. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- D’Anna, E.; Petrini, F.M.; Artoni, F.; Popovic, I.; Simanić, I.; Raspopovic, S.; Micera, S. A Somatotopic Bidirectional Hand Prosthesis with Transcutaneous Electrical Nerve Stimulation Based Sensory Feedback. Sci. Rep. 2017, 7, 10930. [Google Scholar] [CrossRef] [PubMed]
- Silcox, D.H.; Rooks, M.D.; Vogel, R.R.; Fleming, L.L. Myoelectric Prostheses. A Long-Term Follow-up and a Study of the Use of Alternate Prostheses. J. Bone Jt. Surg. 1993, 75, 1781–1789. [Google Scholar] [CrossRef] [PubMed]
- Crandall, R.C.; Tomhave, W. Pediatric Unilateral Below-Elbow Amputees: Retrospective Analysis of 34 Patients Given Multiple Prosthetic Options. J. Pediatr. Orthop. 2002, 22, 380–383. [Google Scholar] [CrossRef]
- Schweisfurth, M.A.; Markovic, M.; Bentz, T.; Wüstefeld, D.; Farina, D.; Dosen, S. Sensorisches Feedback in der Handprothetik. Orthopädietechnik 2017, 68, 34–38. [Google Scholar]
- Brochier, T.; Boudreau, M.-J.; Paré, M.; Smith, A.M. The Effects of Muscimol Inactivation of Small Regions of Motor and Somatosensory Cortex on Independent Finger Movements and Force Control in the Precision Grip. Exp. Brain Res. 1999, 128, 31–40. [Google Scholar] [CrossRef]
- Liang, Z.; Cheng, J.; Zhao, Q.; Zhao, X.; Han, Z.; Chen, Y.; Ma, Y.; Feng, X. High-Performance Flexible Tactile Sensor Enabling Intelligent Haptic Perception for a Soft Prosthetic Hand. Adv. Mater. Technol. 2019, 4, 1900317. [Google Scholar] [CrossRef]
- Anwer, A.H.; Khan, N.; Ansari, M.Z.; Baek, S.-S.; Yi, H.; Kim, S.; Noh, S.M.; Jeong, C. Recent Advances in Touch Sensors for Flexible Wearable Devices. Sensors 2022, 22, 4460. [Google Scholar] [CrossRef] [PubMed]
- Panescu, D. MEMS in Medicine and Biology. IEEE Eng. Med. Biol. Mag. 2006, 25, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Farserotu, J.; Baborowski, J.; Decotignie, J.-D.; Dallemagne, P.; Enz, C.; Sebelius, F.; Rosen, B.; Antfolk, C.; Lundborg, G.; Bjorkman, A.; et al. Smart Skin for Tactile Prosthetics. In Proceedings of the 2012 6th International Symposium on Medical Information and Communication Technology (ISMICT), La Jolla, CA, USA, 25–29 March 2012; IEEE: La Jolla, CA, USA, 2012; pp. 1–8. [Google Scholar]
- Sensinger, J.W.; Dosen, S. A Review of Sensory Feedback in Upper-Limb Prostheses From the Perspective of Human Motor Control. Front. Neurosci. 2020, 14, 345. [Google Scholar] [CrossRef] [PubMed]
- Antfolk, C.; D’Alonzo, M.; Controzzi, M.; Lundborg, G.; Rosen, B.; Sebelius, F.; Cipriani, C. Artificial Redirection of Sensation From Prosthetic Fingers to the Phantom Hand Map on Transradial Amputees: Vibrotactile Versus Mechanotactile Sensory Feedback. IEEE Trans. Neural Syst. Rehabil. Eng. 2013, 21, 112–120. [Google Scholar] [CrossRef]
- Antfolk, C.; Björkman, A.; Frank, S.; Sebelius, F.; Lundborg, G.; Rosen, B. Sensory Feedback from a Prosthetic Hand Based on Air-Mediated Pressure from the Hand to the Forearm Skin. J. Rehabil. Med. 2012, 44, 702–707. [Google Scholar] [CrossRef]
- Childress, D.S. Closed-Loop Control in Prosthetic Systems: Historical Perspective. Ann. Biomed. Eng. 1980, 8, 293–303. [Google Scholar] [CrossRef]
- Jabban, L.; Dupan, S.; Zhang, D.; Ainsworth, B.; Nazarpour, K.; Metcalfe, B.W. Sensory Feedback for Upper-Limb Prostheses: Opportunities and Barriers. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 30, 738–747. [Google Scholar] [CrossRef] [PubMed]
- Stephens-Fripp, B.; Alici, G.; Mutlu, R. A Review of Non-Invasive Sensory Feedback Methods for Transradial Prosthetic Hands. IEEE Access 2018, 6, 6878–6899. [Google Scholar] [CrossRef]
- Cabibihan, J.-J.; Alkhatib, F.; Mudassir, M.; Lambert, L.A.; Al-Kwifi, O.S.; Diab, K.; Mahdi, E. Suitability of the Openly Accessible 3D Printed Prosthetic Hands for War-Wounded Children. Front. Robot. AI 2021, 7, 594196. [Google Scholar] [CrossRef]
- Hazubski, S.; Bamerni, D.; Otte, A. Conceptualization of a Sensory Feedback System in an Anthropomorphic Replacement Hand. Prosthesis 2021, 3, 415–427. [Google Scholar] [CrossRef]
- Cacucciolo, V.; Shintake, J.; Kuwajima, Y.; Maeda, S.; Floreano, D.; Shea, H. Stretchable Pumps for Soft Machines. Nature 2019, 572, 516–519. [Google Scholar] [CrossRef]
- Fishel, J.A.; Santos, V.J.; Loeb, G.E. A Robust Micro-Vibration Sensor for Biomimetic Fingertips. In Proceedings of the 2008 2nd IEEE RAS & EMBS International Conference on Biomedical Robotics and Biomechatronics, Scottsdale, AZ, USA, 19 October 2008; pp. 659–663. [Google Scholar]
- Hari M., A.; Rajan, L. Advanced Materials and Technologies for Touch Sensing in Prosthetic Limbs. IEEE Trans. NanoBioscience 2021, 20, 256–270. [Google Scholar] [CrossRef] [PubMed]
- Engeberg, E.D.; Meek, S. Enhanced Visual Feedback for Slip Prevention with a Prosthetic Hand. Prosthet Orthot. Int. 2012, 36, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.; Walter-Walsh, K.; Preißler, S.; Hofmann, G.O.; Witte, O.W.; Miltner, W.H.R.; Weiss, T. Sensory Feedback Prosthesis Reduces Phantom Limb Pain: Proof of a Principle. Neurosci. Lett. 2012, 507, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Allmendinger, L. Konzeptionierung einer anthropomorphen Ersatzhand mit sensorischem Feedback. Master’s Thesis, Offenburg University, Offenburg, Germany, 2022. [Google Scholar]



| Distal | Proximal | |||
|---|---|---|---|---|
| Palmar | Dorsal | Palmar | Dorsal | |
| v6 | ||||
| v7 | ||||
| v8 | ||||
| v9 | ||||
| v10 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Allmendinger, L.; Hazubski, S.; Otte, A. Conceptualization of an Anthropomorphic Replacement Hand with a Sensory Feedback System. Prosthesis 2022, 4, 695-709. https://doi.org/10.3390/prosthesis4040055
Allmendinger L, Hazubski S, Otte A. Conceptualization of an Anthropomorphic Replacement Hand with a Sensory Feedback System. Prosthesis. 2022; 4(4):695-709. https://doi.org/10.3390/prosthesis4040055
Chicago/Turabian StyleAllmendinger, Lea, Simon Hazubski, and Andreas Otte. 2022. "Conceptualization of an Anthropomorphic Replacement Hand with a Sensory Feedback System" Prosthesis 4, no. 4: 695-709. https://doi.org/10.3390/prosthesis4040055
APA StyleAllmendinger, L., Hazubski, S., & Otte, A. (2022). Conceptualization of an Anthropomorphic Replacement Hand with a Sensory Feedback System. Prosthesis, 4(4), 695-709. https://doi.org/10.3390/prosthesis4040055







