1. Introduction
Socket fit is the most important issue affecting the capability of prosthetic limbs to meet users’ needs [
1,
2]. To accomplish a proper fit, suction and elevated vacuum sockets provide strong mechanical coupling between the residual limb and prosthesis. The vacuum pressure they apply is thought to pull limb soft tissues towards the socket wall, reducing limb-socket motion [
3]. Several studies have demonstrated that increasing vacuum pressure reduces limb-socket motion. Gershutz et al. in an in-lab structured protocol, demonstrated that the range of vacuum pressure was linearly related to the range of displacement during a step [
4]. Youngblood et al. found that introducing a vacuum pressure of 12 inHg eliminated 81% to 93% of the limb motion that occurred in a suction socket [
5]. Klute et al. [
6] used motion analysis to demonstrate that limb cyclic motion was less for elevated vacuum compared with locking pin suspension. Board et al. [
7] and Darter et al. [
8] used radiological imaging methods to demonstrate that bone motion was reduced using elevated vacuum compared with passive suction. Provided vacuum pressure is maintained, vacuum sockets may enhance gait stability and reduce skin injury compared with other types of suspension [
9,
10,
11,
12,
13].
Though they offer benefits, elevated vacuum sockets and to a lesser extent suction sockets can be challenging to use because of maintenance and cost issues [
6,
14]. In a survey of 155 prosthetic professionals, nearly 90% thought the use of elevated vacuum needed careful evaluation and maintenance [
14]. Klute et al. [
6] found that elevated vacuum prostheses required more check sockets and time to adequately fit compared to prostheses with pin suspension. Small leaks in the sealing sleeve, socket wall, vacuum pump, or pump-to-socket connection may cause a reduction or loss of vacuum pressure, leading to an increase in limb-socket motion and an elevated risk of injury. Users might not sense this change until residual limb skin breakdown occurs. A period of no prosthesis use is required until the damaged tissue heals.
Data collected using a sensing system that continuously monitors limb-socket motion during long study protocols or at-home use may provide information to improve performance of suction and elevated vacuum sockets. Researchers may be able to identify quantitative metrics indicative of a deterioration in suspension early before limb injury occurs. This data collection platform may help the prosthetics industry test new product ideas.
The purpose of this research was to determine in a small group of participants if a thin instrumented insert that monitored distal limb motion in suction and elevated vacuum sockets produced meaningful data during in-lab testing and take-home use, and if it warranted further clinical data collection on a larger group of participants. We were particularly interested in the range of cyclic vertical motion during walking, since increased cyclic motion is considered a precursor to a deterioration of socket fit.
2. Materials and Methods
An inductive sensing modality was used to monitor residual limb motion in the socket. The technique is briefly described below and in more detail in
Appendix A. Antenna coils printed on a flex-circuit (polyimide) and placed in the socket are powered using an inductive sensing chip. A trace amount of iron powder embedded in the participant’s liner serves as the antenna’s target [
15]. When the antenna and circuitry are powered, the presence of the magnetically permeable iron local to the antenna reinforces the inductor and lowered the sensor’s oscillation frequency in a distance-dependent manner. The change in frequency measured by the inductive sensing chip is a sensitive measure of distance between the antenna and target.
2.1. Insert Design and Assembly
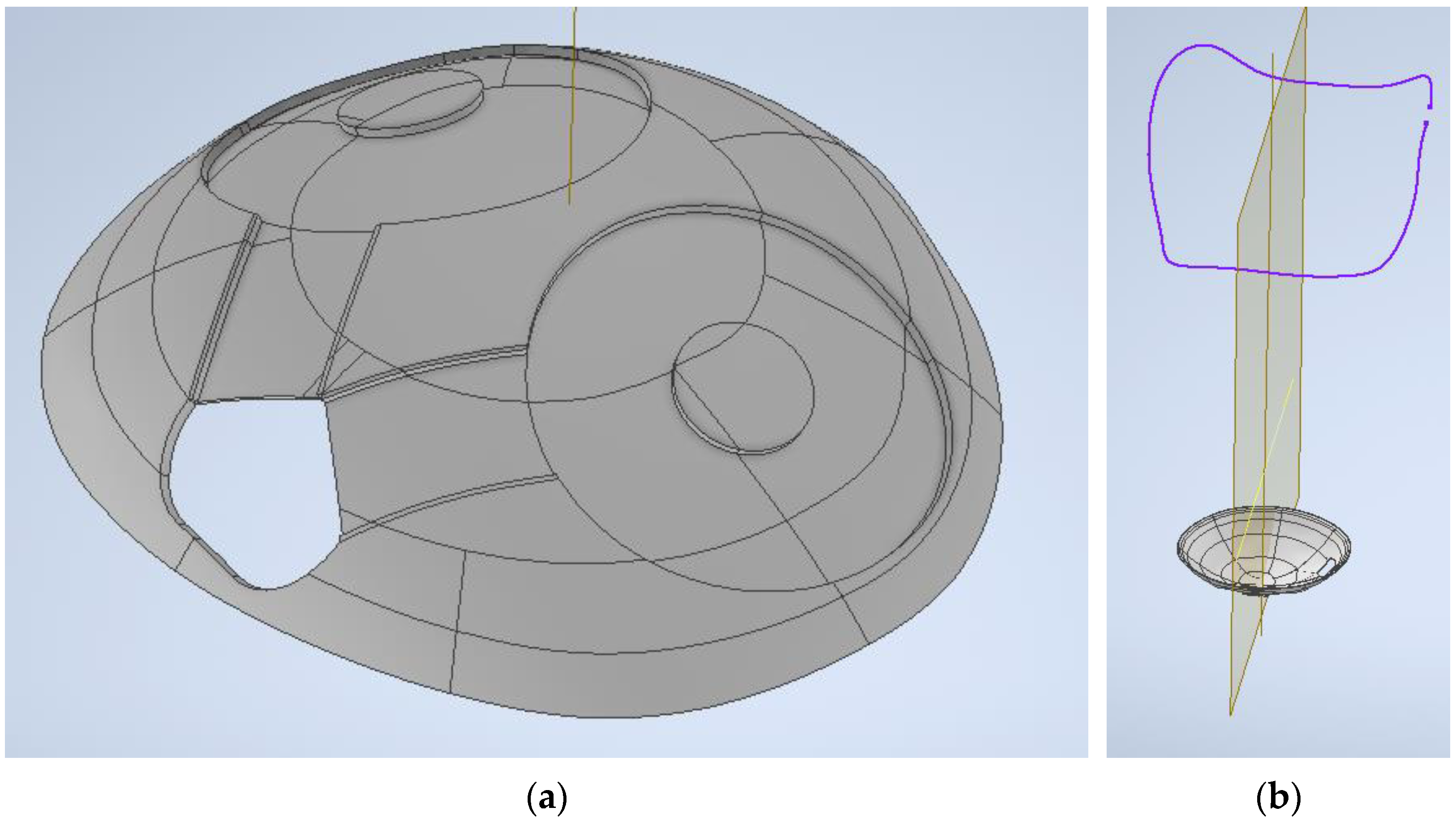
A custom 3D printed plastic insert was designed to hold two antennae (
Figure 1a). An insert was used rather than adhering the antennae directly to the inside of the socket because in prior research we found that the antennae were damaged within 1–2 weeks from the mechanical stress applied by the residual limb [
16]. The insert matched the shape of the distal portion of the socket. Similar to the full socket inserts we designed in previous work [
17], recesses and channels were cut out of the external surface. The recesses and channels held the custom inductive sensor antennae and leadwires. The insert was designed as thin as possible because the long-term objective was a technology to be placed into an existing socket with minimal distortion to socket shape or volume. This design strategy would allow clinical evaluation of an existing socket suspected of vacuum loss. In the present study, however, to ensure that the shape of the socket was not a variable in the study, we fabricated research prostheses where we adjusted the socket shape to accommodate the insert thickness. The insert was affixed to the inside of the socket using double-sided tape, and the cabling was routed through a small hole in the socket wall that was sealed to prevent leaks.
To design the insert, we used a coordinate measurement machine (FaroArm Platinum, FARO Technologies, Lake Mary, FL, USA) (accuracy setting 0.02 mm) to digitize the shape of the participant’s regular socket. The socket brim was also digitized so that the anterior and posterior directions were easily identified when placing the insert into the socket (
Figure 1b). A surface was made from the point cloud data using a computer-aided design software package (Geomagic, Design X, 3D Systems, Research Triangle Park, NC, USA). This surface was projected radially outward (perpendicular to the surface) 1.2 to 1.8 mm to create a solid model of uniform thickness. The amount depended on the desired insert thickness. Different thickness and materials were explored (
Appendix B,
Table A1) to achieve a mechanically durable insert that did not compress the sensors during use.
Parametric modeling software (Inventor, Autodesk, San Francisco, CA, USA) was used to create recesses and channels in the external surface of the insert to hold two custom-designed flexible coil antennae (32.0 mm diameter, 0.15 mm thickness) (
Figure 1a). Material from the center of the antenna was removed to enhance the flexibility so that the insert well conformed to the socket shape (
Figure 2a). The flex-circuit antenna was designed and fabricated to include a 16 mm × 10 mm “tail” with two pairs of exposed solder tabs near the ends of the trace. The solder tabs were used to hold surface mount electronics (0.22 μF capacitor; 10 k
thermistor) and connected the leadwires to the inductive sensing chip. Each antenna was positioned within a 0.8 mm deep spherical ring-shaped recess in the insert and held in place along the inside edge using hot melt adhesive (3779, 3M, St. Paul, MN, USA). The center island of the recess, which projected through the center of the antenna, provided structural support to avoid mechanical pressure on the antenna. Recesses 0.8 mm deep were also made for the antenna tail, and a through hole was made in the insert at the location the two tails met, which was right over a 9.0 mm diameter hole (described below) where the leadwires exited through the socket wall. This design created sufficient space to allow 1.0 mm diameter leadwire to be used to connect from the solder tabs through the socket wall to a signal conditioner/data logger fastened to the pylon of the prosthesis. A data logger from our previous work was used [
16]. A thin piece of ferrite (Würth Elektronik, Niedernhall, Hohenlohe) (0.33 mm thickness) was adhered over the outside of the antenna to reduce radio frequency interference and to provide electromagnetic interference shielding from the carbon fiber socket. A series of slits were cut in the ferrite to improve flexibility (
Figure 2b). A bottom view of a fabricated insert ready for attachment of two antennae and leadwires is shown in
Figure 2c.
Three insert materials were considered—Veroclear (Stratsys, Golden Valley, MN, USA); Nylon PA12 40% glass filled; and Somos PerFORM (DSM Functional Materials, Elgin, IL, USA). Two thicknesses of the PerFORM were tested—1.8 mm and 1.2 mm. Mechanical property information provided by the manufacturer and the thickness of each insert fabricated in this research are listed in
Appendix B,
Table A1 and
Table A2.
Additional steps were taken to prepare the insert and socket. Hot melt was placed over the surface mount capacitor and thermistor. A 7.0 mm hole was drilled in the center distal end of the insert and socket to allow air to pass to the suction valve immediately beneath the socket. Hot melt was placed to cover the connection between the leadwires and the antenna tail. A 9.0 mm diameter hole (for the leadwires) was drilled through the socket wall underneath the cutout (
Figure 3a–c).
2.2. Installation in the Prosthetic Socket
Sockets were fabricated using materials commonly used in clinical practice. The socket includes 4 layers of resin/carbon fiber and 2 layers of Nyglass.
In preparation for installation, the external surface of the insert that was not covered by antennae or leadwires was covered with double-sided adhesive tape (SpeedTape, FastCap, Ferndale, WA, USA) (0.05 mm thickness). The insert was carefully positioned inside the socket while pulling the leadwires through the 9.0 mm hole. Marks previously inked on the anterior and posterior aspects of the insert and socket during test assembly facilitated alignment. An abrasion-resistant expandable sleeve was used to protect the bundle of leadwires exiting the socket. The 7.0 mm and 9.0 mm holes were sealed with epoxy (PLU Series Composite 1, FabTech Systems, Everett, WA, USA). A vacuum bag was placed over the socket to test for leaks. If the socket held at least 25 inHg for at least a 30 s duration, the seal was considered acceptable.
2.3. Calibration
Calibration was performed using the liner to be worn by the participant. For this study, liners for research purposes with a trace amount of iron powder embedded in the elastomer beneath its surface were purchased (Alpha Classic, WillowWood, Mt. Sterling, OH, USA). We used a procedure similar to that in our prior work calibrating sensors in pin-lock sockets [
18]. First, the anterior and posterior surfaces of the liner over the sensor locations were calibrated in a benchtop test jig that allowed an antenna to be moved at incremental distances perpendicular to the liner. This procedure generated the shape of the calibration curve. To establish the zero reference position (liner flush with the insert), the liner was placed in the participant’s research socket while vacuum pressure was applied through the 7.0 mm hole in the distal end of the socket. The setup shown in
Figure 4a–d was used. A silicone balloon in the shape of a residual limb was placed inside a sock, and that assembly was placed inside the liner. A gaitor sleeve was slid into position, and the proximal end of the liner was folded over it. A gaitor was used because during preliminary take-home tests, we found that the sealing sleeve was prone to mechanical damage from the socket brim. The gaitor protected the sealing sleeve. The sealing sleeve was pulled into place to seal both the proximal and distal ends of the socket. The balloon was held at a pressure of approximately 3.4 kPa, and the sensor data acquisition system was started. A 3.4 kPa pressure was used because this was sufficiently high to push the liner against the socket wall but not so high that the balloon was forced out the top of the socket. Five vacuum pressures were applied for 45 s each (5, 10, 15, 20, 25 inHg). Vacuum pressure was returned to 0 inHg for 15 s after each setting. Sensor data at the 10 inHg setting was used as the reference (0 distance) for calibration because it best achieved the objective of the liner flush with the insert without distortion of the liner shape.
2.4. Participants
Participants were included in this study if they had a transtibial amputation at least 18 months prior, were at a Medicare functional classification level (K-level) of 2 or higher (community ambulator who has the ability to transverse most environmental barriers such as curbs, stairs, or uneven surfaces) [
19], and regularly used a prosthesis with suction or elevated vacuum suspension. Participants were excluded if they were currently experiencing skin breakdown, used a walking aide (e.g., cane), or were incapable of walking for 2 min continuously. University of Washington institutional review board approval (IRB #00006874) was obtained before any study procedures were initiated, and written informed consent was obtained before a participant started in the study.
2.5. Study Protocol
The participant visited the lab three times. At the first visit, the research prosthetist conducted a clinical evaluation to determine if inclusion criteria were met. A full inspection of the person’s residual limb was conducted. Demographic information, etiology, medical history, presence of co-morbidities, regularly conducted activities, smoking status, and the design of the currently used prosthesis were recorded while the participant’s socket was scanned with the high-resolution coordinate measurement machine. Body mass index (BMI) was calculated using the formula for people with transtibial limb loss [
20].
A carbon-fiber/resin socket duplicate in shape to the participant’s regular socket was fabricated as described above and the instrumented insert installed. Care was taken to ensure that tight seals were achieved at the suction port and at the sensor cable exit from the socket. Participants wore the socket for several hours to ensure that the insert adhesive compressed to a consistent thickness, as learned in our prior research using socket inserts in clinical studies [
17].
During the second visit, participants conducted an in-lab structured protocol wearing the research prosthesis. Participants donned the research socket, and the research prosthetist made any necessary adjustment to ensure a proper fit. This was the optimal sock thickness and was termed sock opt. Sensor data collection was initiated. Participants executed three activity cycles four times for a total of twelve activity cycles. Each cycle included: standing (10 s); walking on a treadmill (2 min); standing (10 s); and sitting (2 min). After the first three activity cycles (3 of the 12 cycles), participants doffed the research socket and increased their sock ply by adding a sock or changing a current sock to a thicker ply. Participants chose among 1, 2, 3, and 5 ply socks (1–2 ply: 95.5% Tertra-Channel polyester, 4.5% Lycra; 3 ply: 70% wool, 30% tetra-channel polyester; 5-ply: 60% wool, 40% Tertra-Channel polyester, Royal Knit, Inc., Lee’s Summit, MO, USA). They conducted three activity cycles at this sock ply. Participants sat and doffed their prosthesis, increased their sock play again, and conducted three additional activity cycles at this sock ply. Participants sat and doffed, returned to their starting configuration (sock opt), which was a low ply sock or no sock, and conducted three additional activity cycles. After the twelve activity cycles were completed, participants sat in a chair and the researchers prepared them for the take-home part of the study. Participants were asked to wear the research prosthesis at home for at least 3 d, conducting their daily routine and monitoring their comfort via notes or verbal correspondence with the research team. They returned to the lab for their third visit after approximately 1 week to return the research prosthesis. Participants were encouraged to provide comments on their experience during take-home use wearing the research prosthesis.
Collected data were thermally compensated and converted to units of distance (mm) using the calibration data, implementing methods similar to those used previously [
16] and summarized in
Appendix C. For the in-lab structured protocol data, only the walking sections were analyzed. The maxima (which occurred during swing phase) and minima (which occurred during stance phase) for the last ten steps in each cycle were extracted and medians calculated. Anterior and posterior sensor results were calculated separately. The last ten steps were used because in some cycles we observed a change in sensed distance during the initial steps, in part because the vacuum pressure had yet to stabilize.
Take-home data were processed to identify the start and end of prosthesis use each day and to classify user activity as walking, weight shift (standing or sitting), stationary (standing or sitting), or doffed (partial or full). Walks were further categorized into either bouts (≥5 steps) or low commotion (2–4 steps). Computational processing techniques summarized in
Appendix D were implemented. The percentage time for each prosthesis use across all prosthesis day durations was calculated, and the number of steps per day was computed. The median peaks, valleys, and amplitudes (range) were calculated for all steps within each hour of wear and plotted. To visually investigate trends in the data over time, we plotted the data for each step and a 21-point moving average. Histograms were generated to characterize the distribution of the peaks, valleys, and amplitudes in the steps for each day of use.
4. Discussion
Monitoring distal limb motion in sockets that use suction and elevated vacuum suspension could help improve performance of lower-limb prostheses. Research studies using this technology may characterize how variables under practitioner and patient control (e.g., vacuum pressure, sealing sleeve material) or prosthesis use variables (e.g., type of activity, duration of use) affect a meaningful outcome variable, limb motion. Results may help guide prosthesis prescription, and they may stimulate development in the prosthetics industry of more effective and reliable limb suspension products. Continuous distal limb sensing has the potential to be part of an auto-adjustable socket that changes both socket size and vacuum pressure to maintain proper suspension [
21].
We chose to monitor cyclic vertical motion at a distal location in the socket since the suction valve or elevated vacuum pump port is typically located at this position. This location is clinically meaningful to monitor for a loss of vacuum pressure. Further, we sought to position the sensing system in such a way that it introduced minimal disruption to the normal prosthesis, avoiding introducing additional hardware on the outside of the socket. Inductive sensing offers advantages over other techniques reported in the literature to monitor distal limb motion in transtibial prosthesis users. An optical sensing unit positioned underneath the socket to track distal limb motion demonstrated less cyclic vertical motion when a participant used a supracondylar strap compared with no strap, but it required a hole to be cut through the user’s Pelite™ liner to take the measurement [
22]. Radiographic methods implemented to track bone position while participants transitioned to weight-bearing showed less tibia motion under elevated vacuum compared with passive suction, locking pin, patellar tendon bearing, and supra-condylar suspension [
7,
8,
23,
24], but the method required large equipment and exposed participants to radiation. Both techniques would be difficult to implement in a take-home socket. Optical techniques to monitor motion between the liner and side of the socket have been developed [
25,
26,
27], but the need for either a clear socket material or a small hole through the wall make these methods difficult to implement at a distal location. A dipole magnet disk affixed to the liner and tracked with a sensor mounted outside of the socket achieved sub-millimeter resolution [
28], but the technique would need to be modified to measure perpendicular instead of tangential motion for use in the present application. A distal pressure sensor was shown to distinguish sock addition and removal during a structured protocol [
29], though no suction or elevated vacuum sockets were tested. Thin piezoresistive pressure sensors placed at the limb-socket interface did not assess limb cyclic motion since loss of socket contact causes them to sense zero pressure or vacuum pressure during swing phase [
30].
In-lab test results in the present study demonstrated that all participants moved further away from the socket at both the anterior and posterior sensor sites when socks were added and moved closer when socks were removed. Given the short time course of this test, this result is consistent with expectation and verified proper sensor performance. Sock changes distributed over a longer time period, for example during regular at-home use, might not show such consistent results because the residual limb may change volume over time, and limb-socket alignment may change. The complexity of interface stress distribution changes over time has been studied [
31].
When sock ply was reduced (cycles 10 to 12) the people who regularly used elevated vacuum sockets returned closer to baseline than the participant who regularly used a suction socket. It is possible that the soft tissues of the regular elevated vacuum users had adapted differently than suction users. Possibly, the continually applied higher vacuum pressure caused residual limb tissues to change their volume quickly in response to a change in interface pressure. This interpretation is conjecture and would need to be tested through rigorous scientific investigation. Residual limb tissue adaptation to regular use of elevated vacuum has been discussed [
12].
The result that cyclic vertical motion increased when socks were added to a properly fitting socket (
Figure 5) is consistent with clinical experience. Socks may increase the slip between the liner and the socket, and may also introduce air, a compressible medium, to that interface. Air presence may increase cyclic vertical motion because the air compresses during stance phase and expands during swing phase. Participants 3 and 4, who wore no socks for the optimal sock (sock opt) condition during the in-lab test, showed less limb cyclic vertical motion (length of the bars in
Figure 5) for the sock opt condition than participants 1 and 2, who did wear socks for the sock opt condition. During take-home use, participant 3, the only person who did not wear socks, experienced lower and more consistent limb motion amplitude than the other participants (
Figure 6 and
Figure 8c compared with
Supplement S5, Figure S3a–c and
Figure 8a,b,d). The results suggest that adding socks negates part of the intent of suction, to reduce limb motion, and should be avoided. As described in comments collected after completing take-home use (
Supplement S3, Table S1), participants added socks because they usually used a sock (participant 1) or because the extra weight of the research prosthesis compared to their traditional caused them to feel that sock addition was necessary (participants 2 and 4). The results from the present study provide incentive for prosthetics researchers and the industry to investigate sockets that allow size change while maintaining vacuum. Using adjustable-size sockets or providing participants with various thickness custom plastic inserts may accomplish this design objective. Results from a benchtop model of elevated vacuum suggest that the effect of vacuum pressure on the residual limb is primarily determined by air gap distance [
32].
Results from this study do not support the hypothesis that the effectiveness of suspension in suction sockets is reflected as a bimodal distribution of motion, i.e., that there is one amplitude reflecting good suspension and another amplitude reflecting slip. It is clear from the tight distribution of the data during the in-lab test (
Figure 5 and
Supplement 2, Figure S2) compared with that during take-home use (
Supplement S6, Figure S4a–d) that there may be considerable fluctuation in at home environments for how hard participants push into their socket during stance phase and how forceful they pull out during swing phase. Inspection of the histograms in the present study suggests that it is the peaks during swing phase that caused the high variability in the amplitude measurement since their distributions were wider than those of the valleys (
Supplement S6, Figure S4a–d). Participant 3 showed a bimodal distribution for the valleys on day 6, because of either lower weight bearing or less swing pull out during some of his bouts of low commotion activity. The result is consistent with moving about in a workshop, which this person reported as an activity (
Supplement S3, Table S1).
The insert materials used in this study were much stiffer and more durable than the larger thicker instrumented inserts we used in prior studies [
17,
33]. The PerFORM material, with its low elongation at break (1.1%), did not crack, demonstrating it as the best choice of the materials tested here. The thinnest insert that we could fabricate was 1.2 mm, which is too thick to add to a participant’s regular socket because the reduced socket volume may cause discomfort. We believe that the inserts are more appropriate to put into new sockets, enlarging the distal end in the computer-aided design file as done in this study or by placing a dummy insert over the positive mold during the layup. Care must be taken to smooth the insert edge so that it does not cause irritation. An alternative design is to eliminate the insert and place the sensor antennae directly in the layup during fabrication, a procedure that we have described [
34]. Placement within 3D printed sockets may be possible, once the industry advances and printed materials sufficiently strong for this application are available.
The most meaningful limitation in this study that affected socket use in take-home testing was the weight of the research prosthesis compared with participants’ regular prosthesis. This was not a limitation of the inserts, but instead the lack of available blade prostheses to laminate to participants’ research sockets. A comparatively heavy pylon and energy storage and return foot were used instead. An interesting next step would be to match participants’ regular componentry in an investigational prosthesis to achieve comparable weight to the traditional, and to conduct testing for weeks instead of days. One participant felt that the research liner, which had a trace amount of iron powder in the elastomer next to the fabric backing, was stiffer and not as comfortable as his regular liner. However, the research liner was a different product than the participant’s normal liner, which may have contributed to this statement.
Because only distal locations were monitored in the present study, we were not able to distinguish standing from sitting nor a partially doffed from a fully doffed prosthesis in our prosthesis use characterization. In our prior research, we effectively used four sensors to accomplish these distinctions, two distal and two proximal [
16]. If the sit-stand distinction had been available, it would have been possible to determine if there was a greater increase in cyclic vertical motion after sitting than after standing, suggesting a greater loss of suction during sitting. The addition of a vacuum pressure sensor during data collection would allow evaluation of the relationship between vacuum pressure and displacement. A linear relationship was found by Gerschutz et al. using a structured protocol in the lab [
4]. It would also be interesting to simultaneously monitor motion on the side of the socket, as pursued by several research groups [
25,
26,
27,
28], to gain insight into how the magnitude of motion changes from the proximal to the distal end of the socket.