Comparison of the Accuracy between Denture Bases Produced by Subtractive and Additive Manufacturing Methods: A Pilot Study
Abstract
:1. Introduction
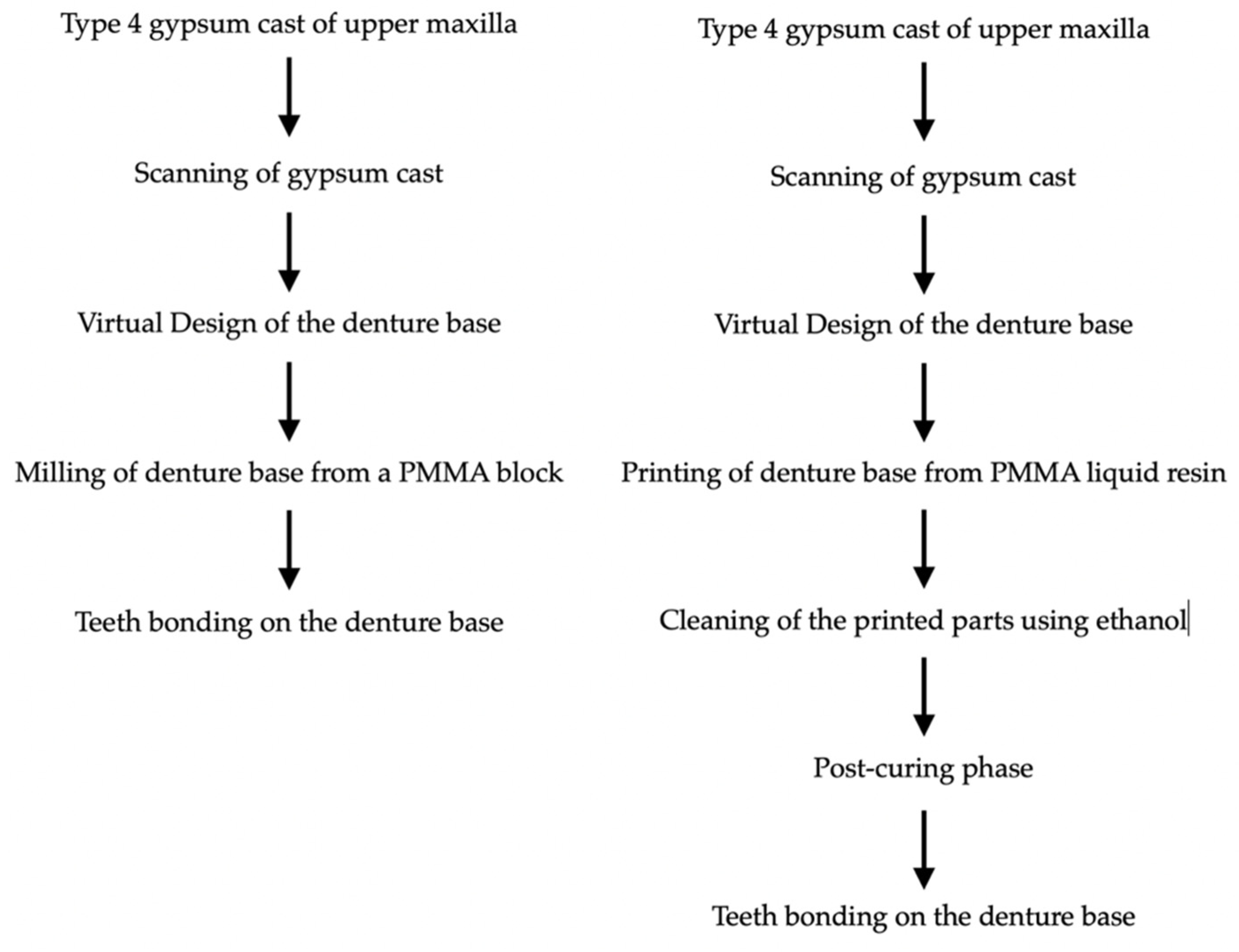
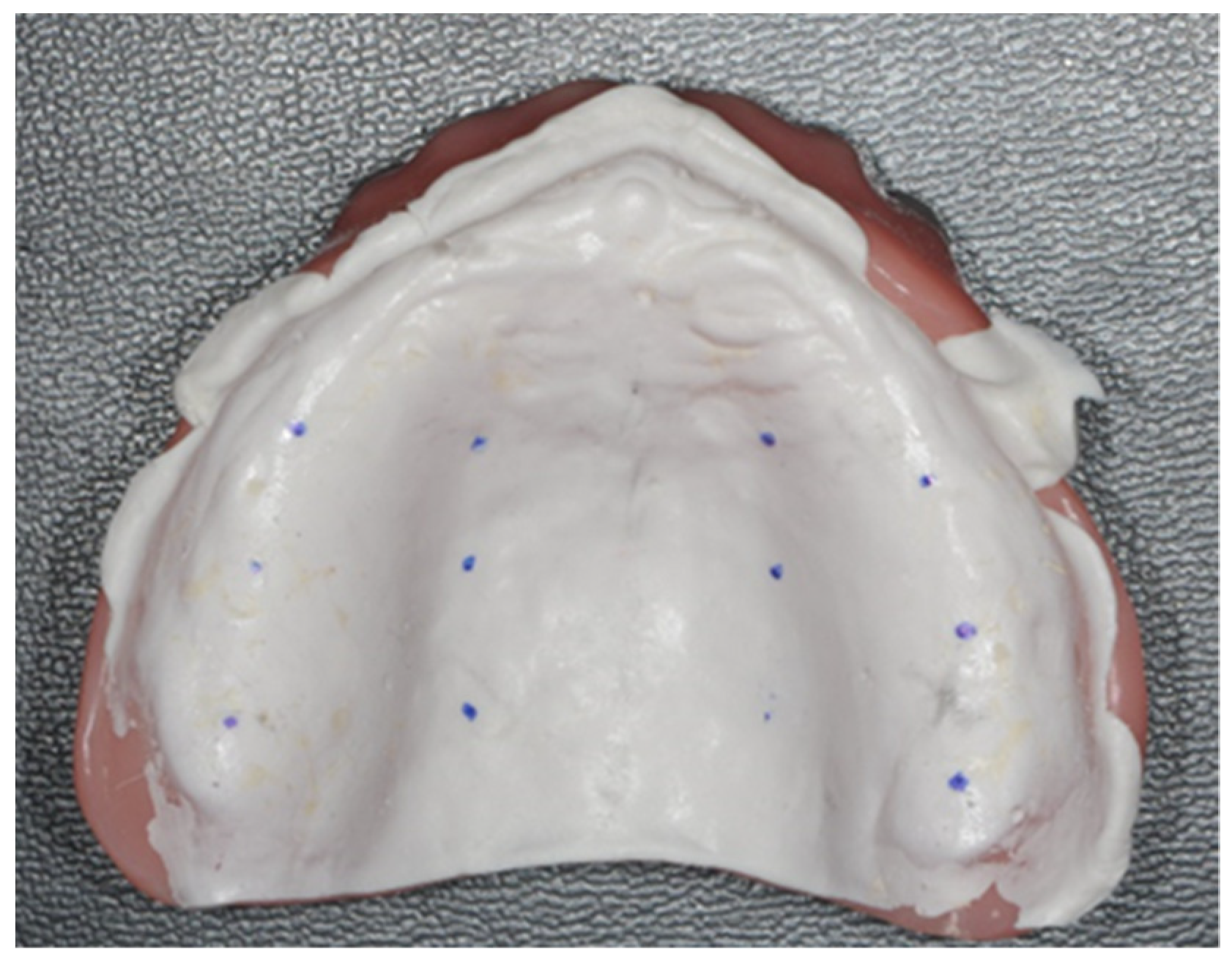
2. Materials and Methods
- Zone 1: one centimeters from the post-dam;
- Zone 2: two centimeters from the post-dam;
- Zone 3: three centimeters from the post-dam.
3. Statistical Analysis
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Baat, C.; van Aken, A.A.; Kalk, W. “Prosthetic condition” and patients’ judgment of complete dentures. J. Prosthet. Dent. 1997, 78, 472–478. [Google Scholar] [CrossRef] [Green Version]
- Al-Ansari, A.; Tantawi, M.E. Patient-reported outcomes and efficiency of complete dentures made with simplified methods: A meta-analysis. Dent. Med. Probl. 2019, 56, 411–418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ceraulo, S.; Leonida, A.; Lauritano, D.; Baldoni, A.; Longoni, S.; Baldoni, M.; Caccianiga, G. Proposal for a Clinical Approach to Geriatric Patients with Anchor Need on Implant for Removable Denture: New Technique. Prosthesis 2020, 2, 185–195. [Google Scholar] [CrossRef]
- Ortensi, L.; Ortensi, M.; Minghelli, A.; Grande, F. Implant-Supported Prosthetic Therapy of an Edentulous Patient: Clinical and Technical Aspects. Prosthesis 2020, 2, 140–152. [Google Scholar] [CrossRef]
- Fueki, K.; Yoshida, E.; Igarashi, Y. A structural equation model relating objective and subjective masticatory function and oral health-related quality of life in patients with removable partial dentures: Mastication and oral health-related quality of life. J. Oral Rehabil. 2011, 38, 86–94. [Google Scholar] [CrossRef]
- Anadioti, E.; Musharbash, L.; Blatz, M.B.; Papavasiliou, G.; Kamposiora, P. 3D printed complete removable dental prostheses: A narrative review. BMC Oral Health 2020, 20, 343. [Google Scholar] [CrossRef]
- Wang, C.; Shi, Y.-F.; Xie, P.-J.; Wu, J.-H. Accuracy of digital complete dentures: A systematic review of in vitro studies. J. Prosthet. Dent. 2021, 125, 249–256. [Google Scholar] [CrossRef]
- Srinivasan, M.; Schimmel, M.; Naharro, M.; O’ Neill, C.; McKenna, G.; Müller, F. CAD/CAM milled removable complete dentures: Time and cost estimation study. J. Dent. 2019, 80, 75–79. [Google Scholar] [CrossRef] [Green Version]
- Wagner, S.A.; Kreyer, R. Digitally Fabricated Removable Complete Denture Clinical Workflows using Additive Manufacturing Techniques. J. Prosthodont. 2021, 30, 133–138. [Google Scholar] [CrossRef]
- Goodacre, C.J.; Garbacea, A.; Naylor, W.P.; Daher, T.; Marchack, C.B.; Lowry, J. CAD/CAM fabricated complete dentures: Concepts and clinical methods of obtaining required morphological data. J. Prosthet. Dent. 2012, 107, 34–46. [Google Scholar] [CrossRef]
- Kattadiyil, M.T.; Goodacre, C.J.; Baba, N.Z. CAD/CAM complete dentures: A review of two commercial fabrication systems. J. Calif. Dent. Assoc. 2013, 41, 407–416. [Google Scholar] [PubMed]
- Bidra, A.S.; Taylor, T.D.; Agar, J.R. Computer-aided technology for fabricating complete dentures: Systematic review of historical background, current status, and future perspectives. J. Prosthet. Dent. 2013, 109, 361–366. [Google Scholar] [CrossRef]
- Steinmassl, O.; Dumfahrt, H.; Grunert, I.; Steinmassl, P.-A. CAD/CAM produces dentures with improved fit. Clin. Oral. Investig. 2018, 22, 2829–2835. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalberer, N.; Mehl, A.; Schimmel, M.; Müller, F.; Srinivasan, M. CAD-CAM milled versus rapidly prototyped (3D-printed) complete dentures: An in vitro evaluation of trueness. J. Prosthet. Dent. 2019, 121, 637–643. [Google Scholar] [CrossRef]
- ISO 5725. Accuracy (Trueness and Precision) of Measuring Methods and Results. Part-I: General Principles and Definitions. Available online: https://www.iso.org/obp/ui/#iso:std:iso:5725:-1:ed-1:v1:en (accessed on 1 August 2019).
- Mobilio, N.; Fasiol, A.; Catapano, S. Survival Rates of Lithium Disilicate Single Restorations: A Retrospective Study. Int. J. Prosthodont. 2018, 31, 283–286. [Google Scholar] [CrossRef]
- Mobilio, N.; Catapano, S. The use of monolithic lithium disilicate for posterior screw-retained implant crowns. J. Prosthet. Dent. 2017, 118, 703–705. [Google Scholar] [CrossRef]
- Mobilio, N.; Stefanoni, F.; Contiero, P.; Mollica, F.; Catapano, S. Experimental and numeric stress analysis of titanium and zirconia one-piece dental implants. Int. J. Oral. Maxillofac. Implant. 2013, 28, e135-42. [Google Scholar] [CrossRef] [Green Version]
- Mobilio, N.; Borelli, B.; Sorrentino, R.; Catapano, S. Effect of fiber post length and bone level on the fracture resistance of endodontically treated teeth. Dent. Mater. J. 2013, 32, 816–821. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mobilio, N.; Fasiol, A.; Franceschetti, G.; Catapano, S. Marginal Vertical Fit along the Implant-Abutment Interface: A Microscope Qualitative Analysis. Dent. J. 2016, 4, 31. [Google Scholar] [CrossRef] [Green Version]
- Ceruti, P.; Mobilio, N.; Bellia, E.; Borracchini, A.; Catapano, S.; Gassino, G. Simplified edentulous treatment: A multicenter randomized controlled trial to evaluate the timing and clinical outcomes of the technique. J. Prosthet. Dent. 2017, 118, 462–467. [Google Scholar] [CrossRef]
- Corsalini, M.; Barile, G.; Catapano, S.; Ciocia, A.; Casorelli, A.; Siciliani, R.; Di Venere, D.; Capodiferro, S. Obturator Prosthesis Rehabilitation after Maxillectomy: Functional and Aesthetical Analysis in 25 Patients. Int. J. Environ. Res. Public Health 2021, 18, 12524. [Google Scholar] [CrossRef] [PubMed]
- Corsalini, M.; Di Venere, D.; Pettini, F.; Stefanachi, G.; Catapano, S.; Boccaccio, A.; Lamberti, L.; Pappalettere, C.; Carossa, S. A comparison of shear bond strength of ceramic and resin denture teeth on different acrylic resin bases. Open Dent. J. 2014, 8, 241–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, W.; Li, Y.; Zhang, Y.; Lv, Y.; Zhang, Y.; Hu, P.; Liu, H.; Ma, Z.; Shen, Y. Design and fabrication of complete dentures using CAD/CAM technology. Medicine 2017, 96, e5435. [Google Scholar] [CrossRef] [PubMed]
- Hwang, H.-J.; Lee, S.J.; Park, E.-J.; Yoon, H.-I. Assessment of the trueness and tissue surface adaptation of CAD-CAM maxillary denture bases manufactured using digital light processing. J. Prosthet. Dent. 2019, 121, 110–117. [Google Scholar] [CrossRef]
- Gibbs, S.B.; Versluis, A.; Tantbirojn, D.; Ahuja, S. Comparison of polymerization shrinkage of pattern resins. J. Prosthet. Dent. 2014, 112, 293–298, Erratum in J. Prosthet. Dent. 2015, 114, 872. [Google Scholar] [CrossRef]
- Mojon, P.; Oberholzer, J.P.; Meyer, J.M.; Belser, U.C. Polymerization shrinkage of index and pattern acrylic resins. J. Prosthet. Dent. 1990, 64, 684–688. [Google Scholar] [CrossRef]
- Collard, S.M.; Karimzadeh, A.; Smith, L.T.; Parikh, U. Polymerization shrinkage, impact strength and roughness of montmorillonite-modified denture base resins. Am. J. Dent. 1991, 4, 285–290. [Google Scholar]
- Ling, L.; Taremi, N.; Malyala, R. A Novel Low-Shrinkage Resin for 3D Printing. J. Dent. 2022, 118, 103957. [Google Scholar] [CrossRef]
- Chavali, R.; Nejat, A.H.; Lawson, N.C. Machinability of CAD-CAM materials. J. Prosthet. Dent. 2017, 118, 194–199. [Google Scholar] [CrossRef]
- Molinero-Mourelle, P.; Gómez-Polo, M.; Gómez-Polo, C.; Ortega, R.; del Río Highsmith, J.; Celemín-Viñuela, A. Preliminary Study on the Assessment of the Marginal Fit of Three-Dimensional Methacrylate Oligomer Phosphine Oxide Provisional Fixed Dental Prostheses Made by Digital Light Processing. Prosthesis 2020, 2, 240–245. [Google Scholar] [CrossRef]
- D’Arienzo, L.F.; D’Arienzo, A.; Borracchini, A. Comparison of the suitability of intra-oral scanning with conventional impression of edentulous maxilla in vivo. A preliminary study. J. Osseointegr. 2018, 10, 115–120. [Google Scholar]
- Quante, K.; Ludwig, K.; Kern, M. Marginal and internal fit of metal-ceramic crowns fabricated with a new laser melting technology. Dent. Mater. 2008, 24, 1311–1315. [Google Scholar] [CrossRef] [PubMed]
- Jahangiri, L.; Estafan, D. A method of verifying and improving internal fit of all-ceramic restorations. J. Prosthet. Dent. 2006, 95, 82–83. [Google Scholar] [CrossRef] [PubMed]
- Habib, S.R.; Ansari, A.S.; Bajunaid, S.O.; Alshahrani, A.; Javed, M.Q. Evaluation of Film Thickness of Crown Disclosing Agents and Their Comparison with Cement Film Thickness after Final Cementation. Eur. J. Dent. 2020, 14, 224–232. [Google Scholar] [CrossRef] [Green Version]
- Nagy, Z.; Simon, B.; Mennito, A.; Evans, Z.; Renne, W.; Vág, J. Comparing the trueness of seven intraoral scanners and a physical impression on dentate human maxilla by a novel method. BMC Oral Health 2020, 20, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Control | Milled DMG Saver | Printed NextDent 5100 3D | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Section | Mapping | Point | Candulor Aesthetic Hot | Model (A) | Model (B) | Model (C) | Model (D) | Model (E) | Model (F) |
| Zone 1 | Hard palate | 1 | 0.36 | 0.25 | 0.19 | 0.22 | 0.24 | 0.14 | 0.31 |
| 2 | 0.31 | 0.29 | 0.14 | 0.16 | 0.19 | 0.13 | 0.36 | ||
| Alveolar Ridge | 3 | 0.35 | 0.29 | 0.15 | 0.21 | 0.13 | 0.16 | 0.20 | |
| 4 | 0.27 | 0.50 | 0.14 | 0.16 | 0.17 | 0.17 | 0.39 | ||
| Zone 2 | Hard palate | 1 | 0.30 | 0.19 | 0.19 | 0.23 | 0.19 | 0.12 | 0.17 |
| 2 | 0.24 | 0.20 | 0.11 | 0.16 | 0.14 | 0.11 | 0.22 | ||
| Alveolar Ridge | 3 | 0.32 | 0.24 | 0.20 | 0.24 | 0.12 | 0.18 | 0.18 | |
| 4 | 0.28 | 0.34 | 0.16 | 0.15 | 0.12 | 0.10 | 0.17 | ||
| Zone 3 | Hard palate | 1 | 0.24 | 0.05 | 0.16 | 0.16 | 0.12 | 0.01 | 0.08 |
| 2 | 0.14 | 0.10 | 0.06 | 0.04 | 0.02 | 0.03 | 0.12 | ||
| Alveolar Ridge | 3 | 0.38 | 0.31 | 0.27 | 0.32 | 0.11 | 0.20 | 0.18 | |
| 4 | 0.34 | 0.35 | 0.15 | 0.24 | 0.15 | 0.15 | 0.17 | ||
| Mean | 0.29 | 0.26 | 0.16 | 0.19 | 0.14 | 0.13 | 0.21 | ||
| Standard deviation | 0.07 | 0.12 | 0.05 | 0.07 | 0.05 | 0.06 | 0.09 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grande, F.; Tesini, F.; Pozzan, M.C.; Zamperoli, E.M.; Carossa, M.; Catapano, S. Comparison of the Accuracy between Denture Bases Produced by Subtractive and Additive Manufacturing Methods: A Pilot Study. Prosthesis 2022, 4, 151-159. https://doi.org/10.3390/prosthesis4020015
Grande F, Tesini F, Pozzan MC, Zamperoli EM, Carossa M, Catapano S. Comparison of the Accuracy between Denture Bases Produced by Subtractive and Additive Manufacturing Methods: A Pilot Study. Prosthesis. 2022; 4(2):151-159. https://doi.org/10.3390/prosthesis4020015
Chicago/Turabian StyleGrande, Francesco, Fabio Tesini, Mario Cesare Pozzan, Edoardo Mochi Zamperoli, Massimo Carossa, and Santo Catapano. 2022. "Comparison of the Accuracy between Denture Bases Produced by Subtractive and Additive Manufacturing Methods: A Pilot Study" Prosthesis 4, no. 2: 151-159. https://doi.org/10.3390/prosthesis4020015
APA StyleGrande, F., Tesini, F., Pozzan, M. C., Zamperoli, E. M., Carossa, M., & Catapano, S. (2022). Comparison of the Accuracy between Denture Bases Produced by Subtractive and Additive Manufacturing Methods: A Pilot Study. Prosthesis, 4(2), 151-159. https://doi.org/10.3390/prosthesis4020015










