Triple Synchronous Colorectal Cancer: An Extremely Rare Case Underscoring the Need for Careful Perioperative Evaluation
Abstract
1. Introduction
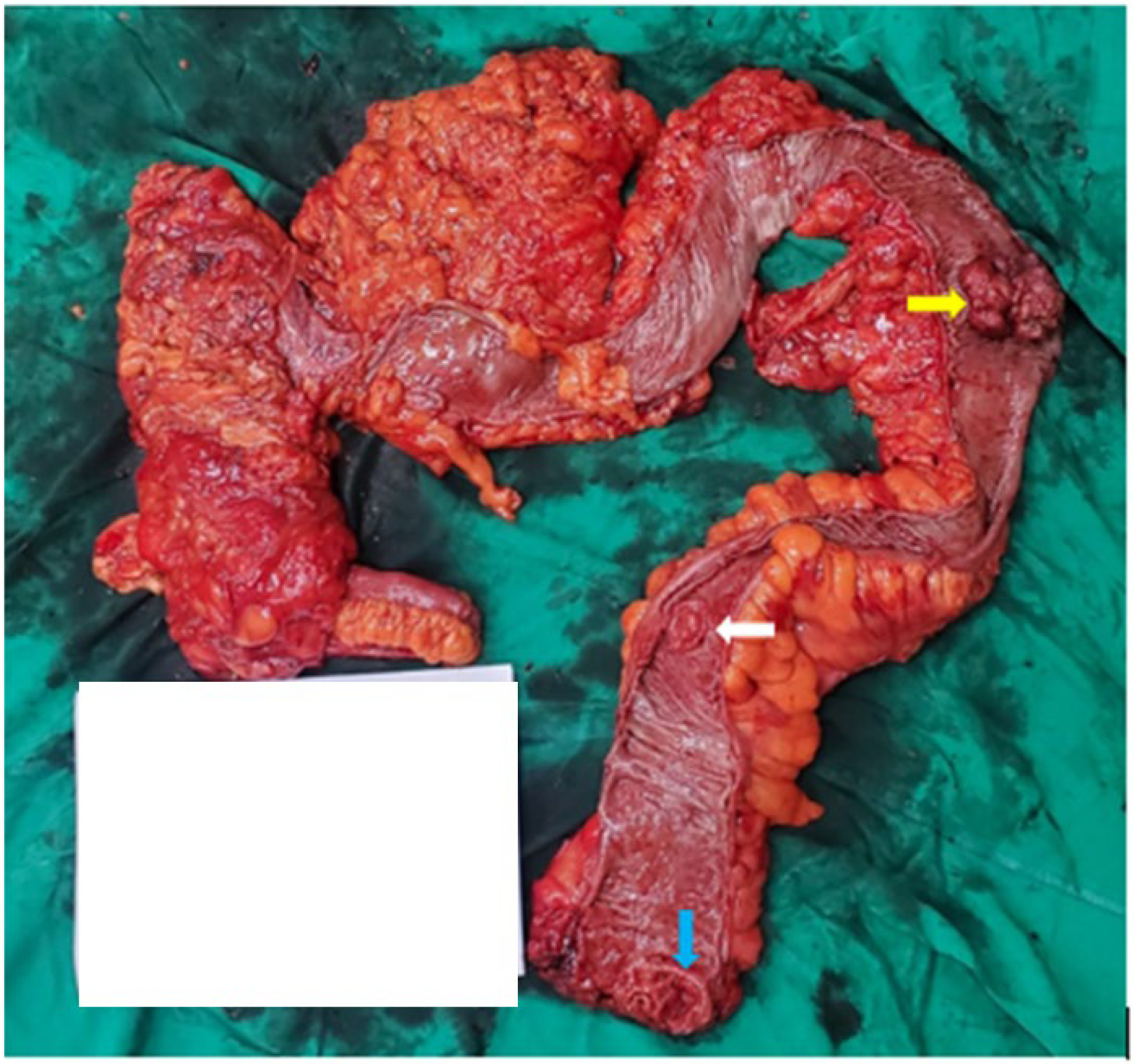
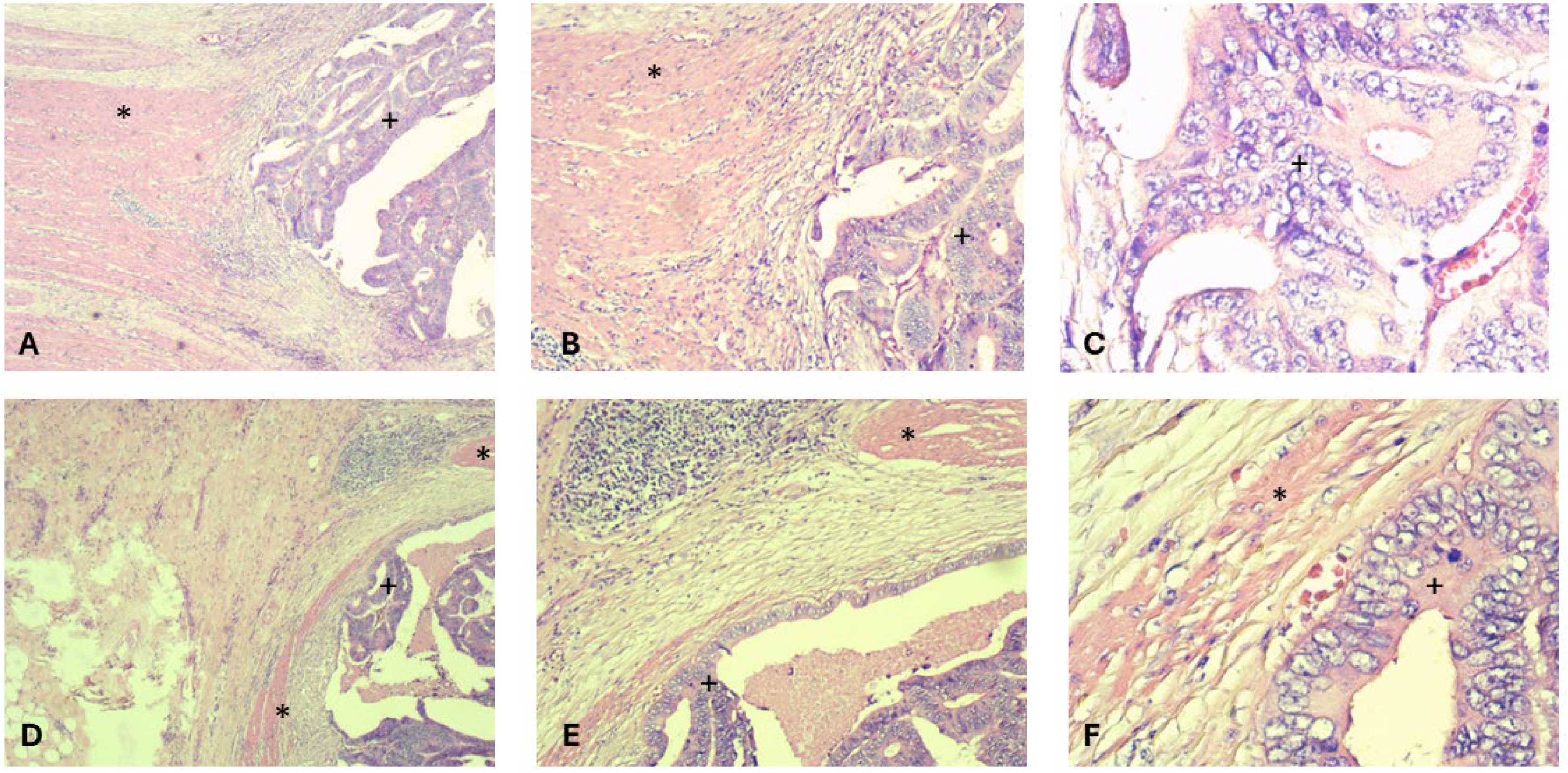
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Flor, N.; Zanchetta, E.; Di Leo, G.; Mezzanzanica, M.; Greco, M.; Carrafiello, G.; Sardanelli, F. Synchronous colorectal cancer using CT colonography vs. other means: A systematic review and meta-analysis. Abdom. Radiol. 2018, 43, 3241–3249. [Google Scholar] [CrossRef] [PubMed]
- Welch, J.P. Multiple colorectal tumors: An appraisal of natural history and therapeutic options. Am. J. Surg. 1981, 142, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Latournerie, M.; Jooste, V.; Cottet, V.; Lepage, C.; Faivre, J.; Bouvier, A. Epidemiology and prognosis of synchronous colorectal cancers. J. Br. Surg. 2008, 95, 1528–1533. [Google Scholar] [CrossRef] [PubMed]
- Yeh, C.-C.; Hsi, S.-C.; Chuu, C.-P.; Kao, Y.-H. Synchronous triple carcinoma of the colon and rectum. World J. Surg. Oncol. 2013, 11, 66. [Google Scholar] [CrossRef] [PubMed]
- Lam, A.K.-Y.; Chan, S.S.-Y.; Leung, M. Synchronous colorectal cancer: Clinical, pathological and molecular implications. World J. Gastroenterol. 2014, 20, 6815. [Google Scholar] [CrossRef] [PubMed]
- Box, J.C.; Rodriguez-Bigas, M.A.; Weber, T.K.; Petrelli, N.J. Clinical implications of multiple colorectal carcinomas in hereditary nonpolyposis colorectal carcinoma. Dis. Colon Rectum 1999, 42, 717–721. [Google Scholar] [CrossRef] [PubMed]
- Fante, R.; Roncucci, L.; Gregorio, C.D.; Tamassia, M.G.; Losi, L.; Benatti, P.; Pedroni, M.; Percesepe, A.; Pietri, S.D.; de Leon, M.P. Frequency and clinical features of multiple tumors of the large bowel in the general population and in patients with hereditary colorectal carcinoma. Cancer Interdiscip. Int. J. Am. Cancer Soc. 1996, 77, 2013–2021. [Google Scholar] [CrossRef]
- Bergeron, E.; Maniere, T.; Do, X.V.; Bensoussan, M.; De Broux, E. Three colonic cancers, two sites of complete occlusion, one patient: A case report. World J. Gastrointest. Surg. 2021, 13, 1095. [Google Scholar] [CrossRef] [PubMed]
- Kato, T.; Alonso, S.; Muto, Y.; Noda, H.; Miyakura, Y.; Suzuki, K.; Tsujinaka, S.; Saito, M.; Perucho, M.; Rikiyama, T. Clinical characteristics of synchronous colorectal cancers in Japan. World J. Surg. Oncol. 2016, 14, 272. [Google Scholar] [CrossRef] [PubMed]
- Michna, M.K.; Bichalska-Lach, M.; Rudzki, M.; Waniczek, D. A rare case of a trifocal synchronous colon cancer in a 65-year old patient. Pol. Ann. Med. 2023, 30, 140–143. [Google Scholar] [CrossRef]
- Van, T.N.; Van, N.P.; Van, D.M.; Van, H.N. Prone Position Laparoscopic Extra-Levator Abdomino-Perineal Excision (eLAPE) Improves Early Outcomes for Low Rectal Cancer. Surg. Gastroenterol. 2024, 29, 244–251. [Google Scholar] [CrossRef]
- Simu, P.; Jung, I.; Banias, L.; Kovacs, Z.; Fulop, Z.Z.; Bara, T.; Simu, I.; Gurzu, S. Synchronous Colorectal Cancer: Improving Accuracy of Detection and Analyzing Molecular Heterogeneity—The Main Keys for Optimal Approach. Diagnostics 2021, 11, 314. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
La, P.V.; Nguyen, D.N.; Tran, D.M.; Duong, T.T.; Tran, M.T.P.; La, P.V.; Le, M.N.T.; Dang, C.P.; Doan, V.A. Triple Synchronous Colorectal Cancer: An Extremely Rare Case Underscoring the Need for Careful Perioperative Evaluation. Gastrointest. Disord. 2025, 7, 36. https://doi.org/10.3390/gidisord7020036
La PV, Nguyen DN, Tran DM, Duong TT, Tran MTP, La PV, Le MNT, Dang CP, Doan VA. Triple Synchronous Colorectal Cancer: An Extremely Rare Case Underscoring the Need for Careful Perioperative Evaluation. Gastrointestinal Disorders. 2025; 7(2):36. https://doi.org/10.3390/gidisord7020036
Chicago/Turabian StyleLa, Phu Van, Diep Ngoc Nguyen, Dien Minh Tran, Tu Tuan Duong, Minh Thanh Phuoc Tran, Phuc Vinh La, Minh Nhat Thanh Le, Cong Phi Dang, and Vu Anh Doan. 2025. "Triple Synchronous Colorectal Cancer: An Extremely Rare Case Underscoring the Need for Careful Perioperative Evaluation" Gastrointestinal Disorders 7, no. 2: 36. https://doi.org/10.3390/gidisord7020036
APA StyleLa, P. V., Nguyen, D. N., Tran, D. M., Duong, T. T., Tran, M. T. P., La, P. V., Le, M. N. T., Dang, C. P., & Doan, V. A. (2025). Triple Synchronous Colorectal Cancer: An Extremely Rare Case Underscoring the Need for Careful Perioperative Evaluation. Gastrointestinal Disorders, 7(2), 36. https://doi.org/10.3390/gidisord7020036




