Abstract
In all reported cases of foreign body migration or impaction in the biliary tree, there is no mention of the presence of hypereosinophilia among the laboratory findings. This could possibly be attributed to the local tissue reaction caused by the impacted foreign body. Here, we present our experience with the removal of a screw from a surgical retractor that became lodged in the common bile duct (CBD) and migrated in a patient who had previously undergone a left lateral hepatectomy for hepatic hydatidosis. The imaging was not sufficient to make a diagnosis, and the interpretation of hypereosinophilia in such a case could pose a challenge.
1. Introduction
In all documented cases of foreign body migration or impaction in the biliary tree, including the most recent ones, hypereosinophilia was not reported. In this report, we share our experience of successfully removing a screw from a surgical retractor that had migrated into the common bile duct (CBD) in a patient who had previously undergone left lateral hepatectomy for hepatic hydatidosis. The patient’s clinical presentation included an elevated eosinophil count, which subsequently normalized after the extraction procedure.
Foreign bodies within the biliary tree are a rare occurrence, and their impact on the body’s immune response is not well-documented in existing medical literature. Our case, however, presented a unique scenario where the presence of the foreign object coincided with an increase in eosinophils, indicating a potential link between the foreign body and the immune system’s response. While eosinophilia is commonly associated with allergies and parasitic infections, its appearance in this context underscores the adaptability of the immune response.
2. Case
A 47-year-old patient was admitted to the Surgery Unit, with a one-week history of persistent epigastric upper abdominal pain jaundice and no fever, despite medication. The patient had a past medical history of left lateral hepatectomy performed two years ago due to hepatic hydatidosis. Physical examination revealed abdominal tenderness, distension, and icteric skin and sclerae. Laboratory examination showed elevated levels of total bilirubin (9 mg/dL normal range: 0.3 to 1 mg/dL); direct bilirubin (7 mg/dL normal range: 0.0 to 0.4 mg/dL); aspartate aminotransferase concentration (90 U/L normal range: up to 38 U/L); alanine aminotransferase concentration (86 U/L normal values up to 40 U/L); alkaline phosphatase concentration (321 U/L normal values up to 115 U/L); gamma glutamyl transpeptidase concentration (118 U/L normal values up to 39 U/L); and white blood cell counts (22,000/mm3 normal range: 4500 to 11,000 mm3), as well as increased percentage of neutrophils (82% normal range 45 to 70%), alongside elevated eosinophils eosinophils (11% normal range: 2 to 4%).
The abdominal ultrasound (US) revealed dilation of the extra-hepatic tree. The initial clinical suspicion was recurrence of hepatic hydatidosis, with a possible biliary fistula and subsequent cholangitis. Contrast-enhanced magnetic resonance cholangiopancreatography (MRCP) showed potential recurrence of hepatic hydatidosis without communication with the biliary system. The biliary tree appeared dilated, and a low signal filling defect was observed in the distal CBD (Figure 1).

Figure 1.
Contrast-enhanced magnetic resonance cholangiopancreatography (MRCP) revealed a possible recurrence of hepatic hydatidosis, but no communication was observed with the biliary tree. However, the biliary tree exhibited dilation and a distal common bile duct filling defect with a low signal (arrow).
These findings led to the hypothesis of cholelithiasis as a possible cause for the patient’s symptoms.
An Endoscopic Retrograde Cholangiopancreatography (ERCP) was performed, revealing a foreign body impacted inside the CBD, identified as a screw from the previous surgical retractor. After sphincterotomy, the size and shape of the screw allowed for its removal using a Fogarty balloon catheter (Figure 2). The patient recovered without complications and was discharged in good condition. In the post-operative period, there was a gradual reduction in eosinophils, reaching a normal range within 7 days (white blood cell counts 8500 mm3, eosinophils 3.8%).
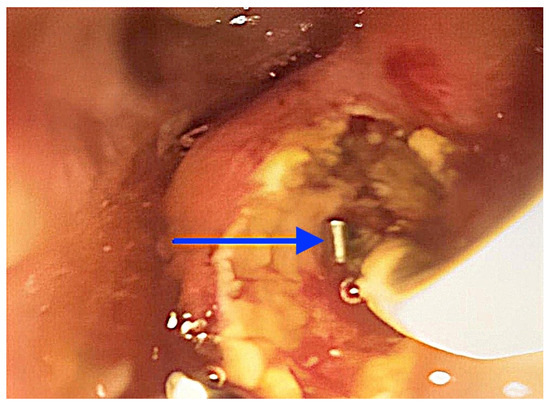
Figure 2.
A screw from a surgical retractor (arrow), which was residual from the previous hepatic surgery, was successfully extracted from the common bile duct (CBD) during Endoscopic Retrograde Cholangiopancreatography (ERCP) using a balloon catheter.
3. Discussion
Our case report presents a rare and intriguing occurrence of a post-surgical impacted foreign body in the biliary tree, effectively managed with ERCP. What sets this case apart is the unexpected diagnosis that emerged, diverging from the initial suspicion of biliary hydatidosis or cholelithiasis based on the patient’s clinical history and imaging findings.
Our case serves as a compelling example of the expanding role of endoscopy in replacing traditional redo-surgical approaches for gastro-intestinal post-surgical complications [1,2,3,4]. While cholangioscopy is a valuable additional treatment option for indeterminate biliary stenosis and biliary stone removal [5,6,7,8,9,10,11,12,13,14,15], its unavailability at our Endoscopy Unit during the procedure necessitated the use of the traditional technique.
Impaction of foreign bodies in the biliary tree presents a complex and challenging differential diagnosis. This underscores the significance of integrating diverse diagnostic modalities and techniques when evaluating complex hepatobiliary conditions. While imaging modalities such as contrast-enhanced MRI provide critical insights into anatomical abnormalities and aid in forming initial hypotheses, they may not always provide a comprehensive understanding of the underlying pathology.
This highlights the complementary role of endoscopy, as it enables direct visualization, precise interventions, and confirmatory diagnoses. It is essential for clinicians to be aware of the limitations of imaging techniques, such as MRI, which can yield false positives or negatives, encounter challenges in differentiating certain pathologies, and lack real-time visualization of dynamic processes. Thus, considering alternative diagnostic modalities becomes crucial in such scenarios.
In our case, the presence of hypereosinophilia initially raised suspicion of the spreading of a small component of a recurrent hydatid cyst in the biliary tree. However, the rapid normalization of the eosinophil count following the removal of the metallic foreign body confirmed that hyperesinophilia could serve as a marker for the local tissue reaction to the impacted foreign body.
Experiences involving the migration of foreign bodies within the biliary tree have been documented in the medical literature, often in the form of case reports.
In the case described by Wen et al., a 58-year-old patient presented with right upper quadrant abdominal pain and fever, approximately one month after undergoing laparotomic cholecystectomy and choledochojejunostomy. A CT scan revealed an abscess in the liver lobe and a linear curve of high-density material within a mass. During a subsequent ERCP procedure, a curved, linear, rusty metallic surgical suture needle measuring 1.7 cm was removed from the patient’s hepatic duct [16].
The case reported by Corral et al. presents an even more remarkable scenario of foreign body migration within the biliary tree. An 82-year-old patient, previously subjected to embolization of the cystic and hepatic arteries for pseudoaneurysm, developed cholangitis six months later. Cultures were positive for Escherichia Coli. While CT imaging showed dilation of the intrahepatic ducts, the subsequent cholangiography revealed the migration of embolization coils into the CBD. Coils were successfully removed in two ERCP sessions, using an 8.5 mm balloon sweeping technique and a biopsy forceps [17]. Recent reports have also highlighted cases of endovascular coil migration into the cystic duct, gallbladder, and jejunum, typically occurring 3 months to 3 years after placement [18,19,20,21].
In a recent video article, Zhang et al. reported the case of a 77-year-old woman, with a history of previous laparoscopic T-tube drainage and laparoscopic cholecystectomy (more than 10 years prior), who was admitted for routine biliary stones management. The patient had undergone ERCP with biliary stenting for choledocholithiasis six months before her current visit. While laboratory tests indicated normal results, an abdominal CT scan showed bile duct dilatation with large bile duct stones and the presence of a high-density image of the stent that had migrated into the CBD. During the ERCP, the operators successfully removed the stent using a specialized mesh basket (Microtech, Nanjing, China) [22].
In the paper by Di Mitri et al., two cases involving patients aged 71 and 70 with foreign body impactions in the CBD were reported. The foreign bodies in the CBD included a fractured distal end of a Dormia basket, previously used for mechanical lithotripsy of a large stone, and an impacted biliary plastic stent placed for a CBD stricture, respectively. During the ERCP procedures, after all attempts to remove the foreign bodies proved ineffective, the operators employed the SpyGlass System in both cases. In the patient with the impacted Dormia basket, after fragmenting the large stone using laser lithotripsy (Storz 25750220, 365 mm diameter fiber, 15 Hz/20 W), the basket was extracted with the assistance of a SpyBite forceps (Boston Scientific, Massachusetts, USA). Subsequently, a successful balloon sweep of the CBD was performed using the Fogarty balloon catheter. In the second patient, the operators removed the plastic stent by grasping its wall with the SpyBite forceps [23].
The impact of a foreign body in the biliary tree is an event that demands immediate attention due to the potential development of cholangitis, a serious and potentially life-threatening condition. Cholangitis arises when there is inflammation and infection within the biliary tree, which can occur as a consequence of biliary obstruction, often caused by the presence of a foreign body. This condition can lead to severe complications if not promptly diagnosed and managed.
In such cases, ERCP is the preferred procedure for foreign body retrieval. In our case, the shape and position of the foreign body allowed for extraction using a simple balloon; in more complex cases, cholangioscopy becomes necessary in places where the foreign body is tightly impacted, as reported in the literature.
Remarkably, in all the cases we have described, there is a conspicuous absence of mention regarding eosinophilia as a diagnostic factor when evaluating the patients’ clinical conditions. Eosinophilia, characterized by an elevated number of eosinophils in the bloodstream, is typically associated with various factors, including parasitic infections and allergic reactions, especially within the gastrointestinal tract [24,25,26,27,28,29,30]. It is a valuable laboratory finding that can provide important diagnostic insights. However, our case report offers a unique perspective on eosinophilia in the context of a patient with a history of abdominal surgery.
In our case report, we emphasize the role of eosinophilia as a supplementary indicator, in conjunction with imaging findings, of a complication that can manifest even years after the initial surgical procedure. This unexpected elevation in eosinophil count initially raised questions, as it did not align with the typical etiologies of eosinophilia, such as parasitic infections or allergies. However, it became a pivotal component of the diagnostic puzzle, ultimately leading to the discovery of a migrated foreign body within the biliary tree. This case serves as a compelling example of how laboratory findings, such as eosinophilia, can play a useful role in guiding clinicians toward accurate diagnoses, particularly in atypical clinical scenarios.
The field of endoscopy, encompassing procedures such as ERCP, has witnessed significant advancements in recent years. It has established itself as an increasingly valuable tool in the diagnosis and management of hepatobiliary diseases. In our reported case, the successful removal of the foreign body through ERCP not only alleviated the patient’s distressing symptoms but also underscored the potential of endoscopic interventions to deliver effective therapeutic outcomes. ERCP allows for precise and minimally invasive interventions within the biliary tree, reducing the need for traditional, more invasive surgical approaches.
While imaging techniques, such as Magnetic Resonance Imaging (MRI), play a pivotal role in providing valuable insights into anatomical abnormalities and forming initial diagnostic hypotheses, they may fall short in providing a comprehensive understanding of the underlying pathology in certain cases. This limitation becomes particularly pronounced when dealing with dynamic processes and subtle pathophysiological changes that can occur within the biliary tree. Therefore, it is imperative for healthcare providers to explore alternative diagnostic modalities, such as endoscopy. Endoscopy not only facilitates direct visualization of the affected area but also enables precise interventions and confirmatory diagnoses in real-time. It has become an indispensable tool for clinicians when dealing with complex hepatobiliary conditions.
In summary, our clinical case highlights the critical importance of considering eosinophilia as a potential diagnostic factor, even in patients with a history of abdominal surgery. It serves as a reminder that unexpected laboratory findings can lead to the detection of uncommon but clinically significant conditions. Additionally, the case underscores the growing significance of endoscopy, particularly ERCP, in the field of hepatobiliary medicine, offering effective and minimally invasive solutions to complex clinical challenges. This holistic approach to diagnosis and treatment has the potential to improve patient outcomes and the overall quality of care in the management of biliary tree-related complications.
Author Contributions
Conceptualization, E.S. and F.V.M.; methodology, F.R., R.A., S.T., M.M., (Marta Marasà) S.C., M.M. (Marcello Maida), D.B., G.C. and E.F.; data curation, M.M. and D.B.; writing—original draft preparation, E.S. and F.V.M., editing, F.V.M.; supervision, D.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study, due to the fact that this was only a retrospective case report, as internal policy.
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
Not applicable.
Acknowledgments
All the authors thank the staff of Hospital G. Giglio for their support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Mandarino, F.V.; Barchi, A.; D’Amico, F.; Fanti, L.; Azzolini, F.; Viale, E.; Esposito, D.; Rosati, R.; Fiorino, G.; Bemelman, W.A.; et al. Endoscopic Vacuum Therapy (EVT) versus Self-Expandable Metal Stent (SEMS) for Anastomotic Leaks after Upper Gastrointestinal Surgery: Systematic Review and Meta-Analysis. Life 2023, 13, 287. [Google Scholar] [CrossRef]
- Mandarino, F.V.; Testoni, S.G.G.; Barchi, A.; Pepe, G.; Esposito, D.; Fanti, L.; Viale, E.; Biamonte, P.; Azzolini, F.; Danese, S. Gastric emptying study before gastric peroral endoscopic myotomy (G-POEM): Can intragastric meal distribution be a predictor of success? Gut 2023, 72, 1019–1020. [Google Scholar] [CrossRef]
- Mandarino, F.V.; Barchi, A.; Fanti, L.; D’Amico, F.; Azzolini, F.; Esposito, D.; Biamonte, P.; Lauri, G.; Danese, S. Endoscopic vacuum therapy for post-esophagectomy anastomotic dehiscence as rescue treatment: A single center case series. Esophagus 2022, 19, 417–425. [Google Scholar] [CrossRef]
- Mandarino, F.V.; Esposito, D.; Spelta, G.N.E.; Cavestro, G.M.; Rosati, R.; Parise, P.; Gemma, M.F.; Fanti, L. Double layer stent for the treatment of leaks and fistula after upper gastrointestinal oncologic surgery: A retrospective study. Updates Surg. 2022, 74, 1055–1062. [Google Scholar] [CrossRef]
- Nabi, Z.; Reddy, D.N. Multidisciplinary Approach to Indeterminate Biliary Strictures. Gastrointest. Endosc. Clin. N. Am. 2022, 32, 411–425. [Google Scholar] [CrossRef]
- Pallio, S.; Sinagra, E.; Santagati, A.; D’Amore, F.; Pompei, G.; Conoscenti, G.; Romeo, F.; Borina, E.; Melita, G.; Rossi, F.; et al. Use of catheter-based cholangioscopy in the diagnosis of indeterminate stenosis: A multi-centre experience. Minerva Gastroenterol. 2022. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Ramchandani, M.; Reddy, D.N.; Gupta, R.; Lakhtakia, S.; Tandan, M.; Darisetty, S.; Sekaran, A.; Rao, G.V. Role of single-operator peroral cholangioscopy in the diagnosis of indeterminate biliary lesions: A single-center, prospective study. Gastrointest. Endosc. 2011, 74, 511–519. [Google Scholar] [CrossRef]
- Kalaitzakis, E.; Webster, G.J.; Oppong, K.W.; Kallis, Y.; Vlavianos, P.; Huggett, M.; Dawwas, M.F.; Lekharaju, V.; Hatfield, A.; Westaby, D.; et al. Diagnostic and therapeutic utility of single-operator peroral cholangioscopy for indeterminate biliary lesions and bile duct stones. Eur. J. Gastroenterol. Hepatol. 2012, 24, 656–664. [Google Scholar] [CrossRef]
- Chaves, J.; Fernandez, Y.; Viesca, M.; Arvanitakis, M. Using Endoscopy in the Diagnosis of Pancreato-Biliary Cancers. Cancers 2023, 15, 3385. [Google Scholar] [CrossRef]
- Becq, A.; Soualy, A.; Camus, M. Cholangioscopy for biliary diseases. Curr. Opin. Gastroenterol. 2023, 39, 67–74. [Google Scholar] [CrossRef]
- Shin, J.; Oh, C.H.; Dong, S.H. Single-operator Cholangioscopy Guided Lithotripsy. Korean J. Gastroenterol. 2022, 80, 163–168. [Google Scholar] [CrossRef]
- Sato, T.; Nakai, Y.; Fujishiro, M. Current endoscopic approaches to biliary strictures. Curr. Opin. Gastroenterol. 2022, 38, 450–460. [Google Scholar] [CrossRef]
- Oleas, R.; Alcívar-Vasquez, J.; Robles-Medranda, C. New technologies for indeterminate biliary strictures. Transl. Gastroenterol. Hepatol. 2022, 7, 22. [Google Scholar] [CrossRef]
- Podboy, A.; Gaddam, S.; Park, K.; Gupta, K.; Liu, Q.; Lo, S.K. Management of Difficult Choledocholithiasis. Dig. Dis. Sci. 2022, 67, 1613–1623. [Google Scholar] [CrossRef]
- Lee, T.; Teng, T.Z.J.; Shelat, V.G. Choledochoscopy: An update. World J. Gastrointest. Endosc. 2021, 13, 571–592. [Google Scholar] [CrossRef]
- Wen, T.C.; Lin, K.H.; Chen, Y.Y. Migration of a Retained Surgical Suture Needle in the Common Bile Duct. Diagnostics 2022, 12, 2276. [Google Scholar] [CrossRef]
- Corral, J.E.; Woodward, T.A.; Lukens, F.J. All wired up: Migration of endovascular coils to the common bile duct. Clin. Gastroenterol. Hepatol. 2017, 16, A23–A24. [Google Scholar] [CrossRef]
- AlGhamdi, H.S.; Saeed, M.A.; Altamimi, A.R.; O’Hali, W.A.; Khankan, A.A.; Altraif, I.H. Endoscopic extraction of vascular embolization coils that have migrated into the biliary tract in a liver transplant recipient. Dig. Endosc. 2012, 24, 462–465. [Google Scholar] [CrossRef]
- Turaga, K.K.; Amirlak, B.; Davis, R.E.; Yousef, K.; Richards, A.; Fitzgibbons, R.J., Jr. Cholangitis after coil embolization of an iatrogenic hepatic artery pseudoaneurysm: An unusual case report. Surg. Laparosc. Endosc. Percutaneous Tech. 2006, 16, 36–38. [Google Scholar] [CrossRef]
- Van Steenbergen, W.; Lecluyse, K.; Maleux, G.; Pirenne, J. Successful percutaneous cholangioscopic extraction of vascular coils that had eroded into the bile duct after liver transplantation. Endoscopy 2007, 39 (Suppl. S1), E210–E211. [Google Scholar] [CrossRef][Green Version]
- Raashed, S.; Chandrasegaram, M.D.; Alsaleh, K.; Schlaphoff, G.; Merrett, N.D. Vascular coil erosion into hepaticojejunostomy following hepatic arterial embolisation. BMC Surg. 2015, 15, 51. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Feng, Y. Radiation-free digital cholangioscopy-guided removal of bile duct foreign body and holmium laser lithotripsy for large common bile duct stones. Endoscopy 2023, 55, E420–E421. [Google Scholar] [CrossRef] [PubMed]
- Di Mitri, R.; Mocciaro, F.; Bonaccorso, A.; Conte, E. SpyGlass rescue treatment of common bile duct impacted foreign bodies. Dig. Liver Dis. 2018, 51, 453. [Google Scholar] [CrossRef]
- van Balkum, M.; Kluin-Nelemans, H.; van Hellemond, J.J.; van Genderen, P.J.J.; Wismans, P.J. Hypereosinophilia: A diagnostic challenge. Neth. J. Med. 2018, 76, 431–436. [Google Scholar]
- Roufosse, F.; Weller, P.F. Practical approach to the patient with hypereosinophilia. J. Allergy Clin. Immunol. 2010, 126, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Moller, D.; Tan, J.; Gauiran, D.T.V.; Medvedev, N.; Hudoba, M.; Carruthers, M.N.; Dehghan, N.; van den Berghe, J.; Bruyère, H.; Chen, L.Y.C. Causes of hypereosinophilia in 100 consecutive patients. Eur. J. Haematol. 2020, 105, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.Y.; Khoury, P.; Ware, J.M.; Holland-Thomas, N.C.; Stoddard, J.L.; Gurprasad, S.; Waldner, A.J.; Klion, A.D. Marked and persistent eosinophilia in the absence of clinical manifestations. J. Allergy Clin. Immunol. 2014, 133, 1195–1202. [Google Scholar] [CrossRef]
- Mandarino, F.V.; Sinagra, E.; Barchi, A.; Verga, M.C.; Brinch, D.; Raimondo, D.; Danese, S. Gastroparesis: The Complex Interplay with Microbiota and the Role of Exogenous Infections in the Pathogenesis of the Disease. Microorganisms 2023, 11, 1122. [Google Scholar] [CrossRef]
- Salmeri, N.; Sinagra, E.; Dolci, C.; Buzzaccarini, G.; Sozzi, G.; Sutera, M.; Candiani, M.; Ungaro, F.; Massimino, L.; Danese, S.; et al. Microbiota in Irritable Bowel Syndrome and Endometriosis: Birds of a Feather Flock Together-A Review. Microorganisms 2023, 11, 2089. [Google Scholar] [CrossRef]
- Massimino, L.; Barchi, A.; Mandarino, F.V.; Spanò, S.; Lamparelli, L.A.; Vespa, E.; Passaretti, S.; Peyrin-Biroulet, L.; Savarino, E.V.; Jairath, V.; et al. A multi-omic analysis reveals the esophageal dysbiosis as the predominant trait of eosinophilic esophagitis. J. Transl. Med. 2023, 21, 46. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).