Italian Cross-Cultural Adaptation of a Knowledge Assessment Tool (IBD-KID2) for Children with Inflammatory Bowel Disease
Abstract
1. Introduction
2. Results
2.1. Conceptual and Semantic Equivalence
2.2. Measurement Equivalence
2.2.1. Participants
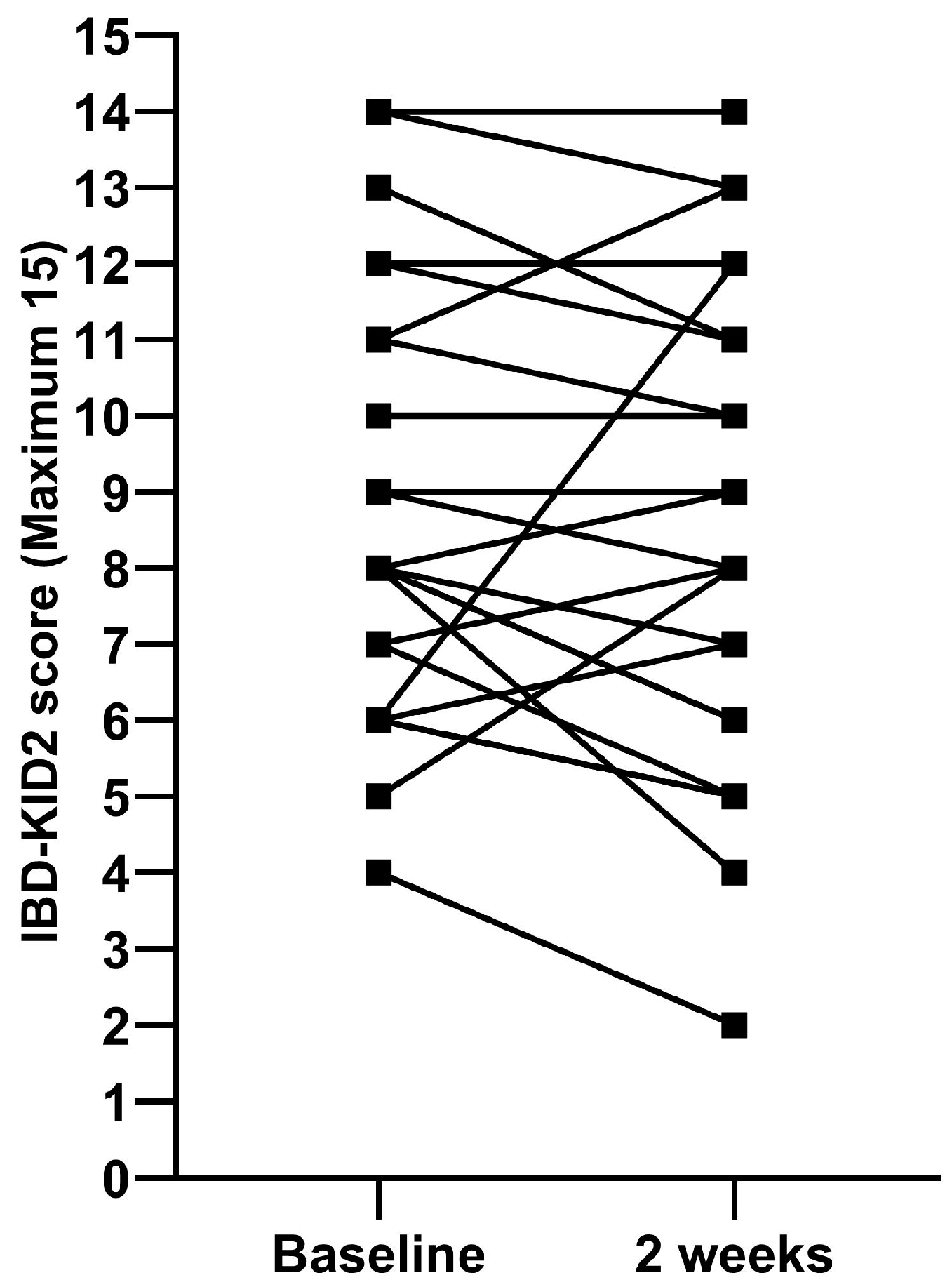
2.2.2. IBD-KID2 Scores
2.2.3. Reliability
2.2.4. Generalizability
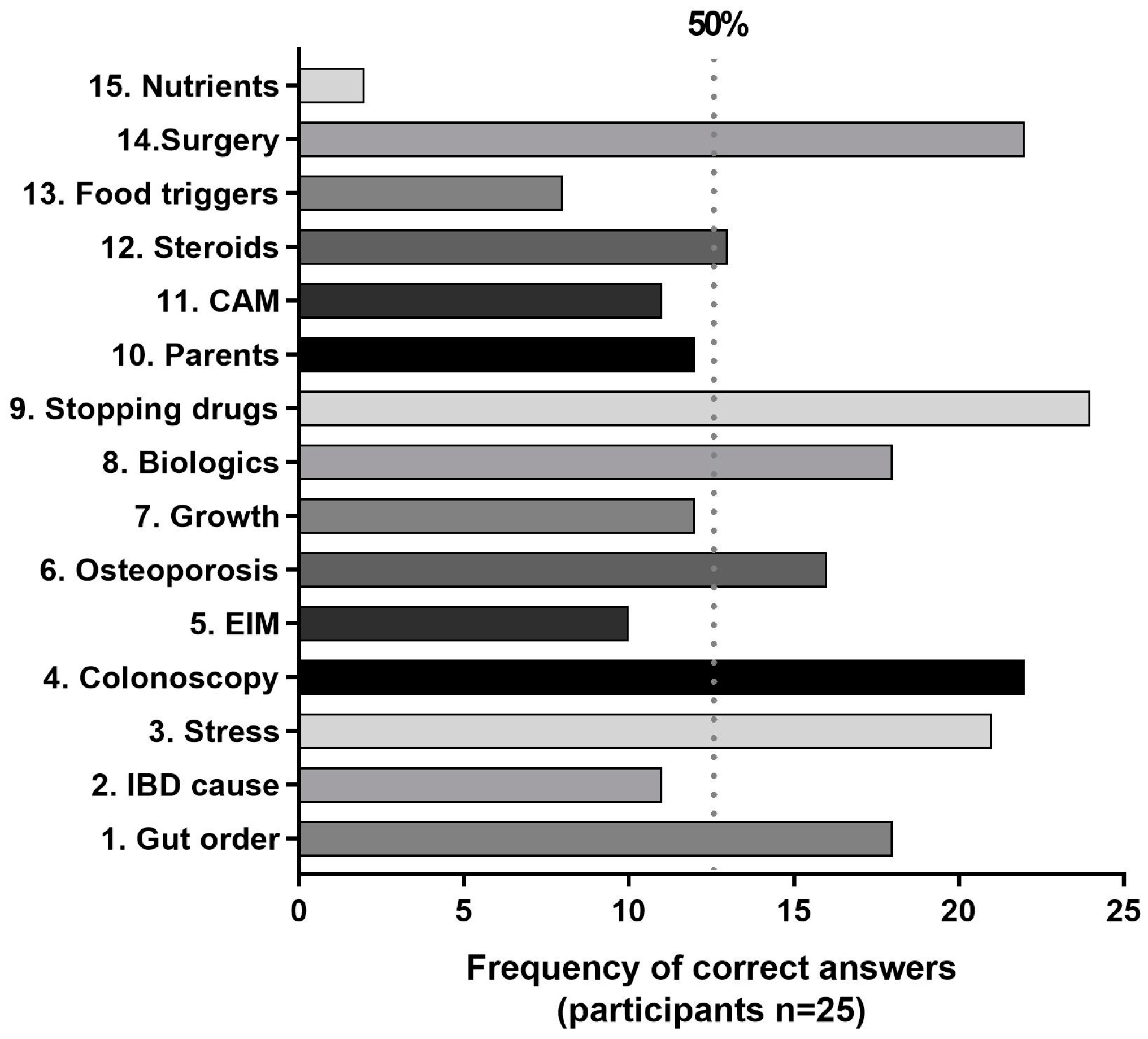
2.2.5. Areas of Knowledge
2.2.6. Internal Consistency
3. Discussion
3.1. Strengths
3.2. Limitations
4. Materials and Methods
4.1. IBD-KID2
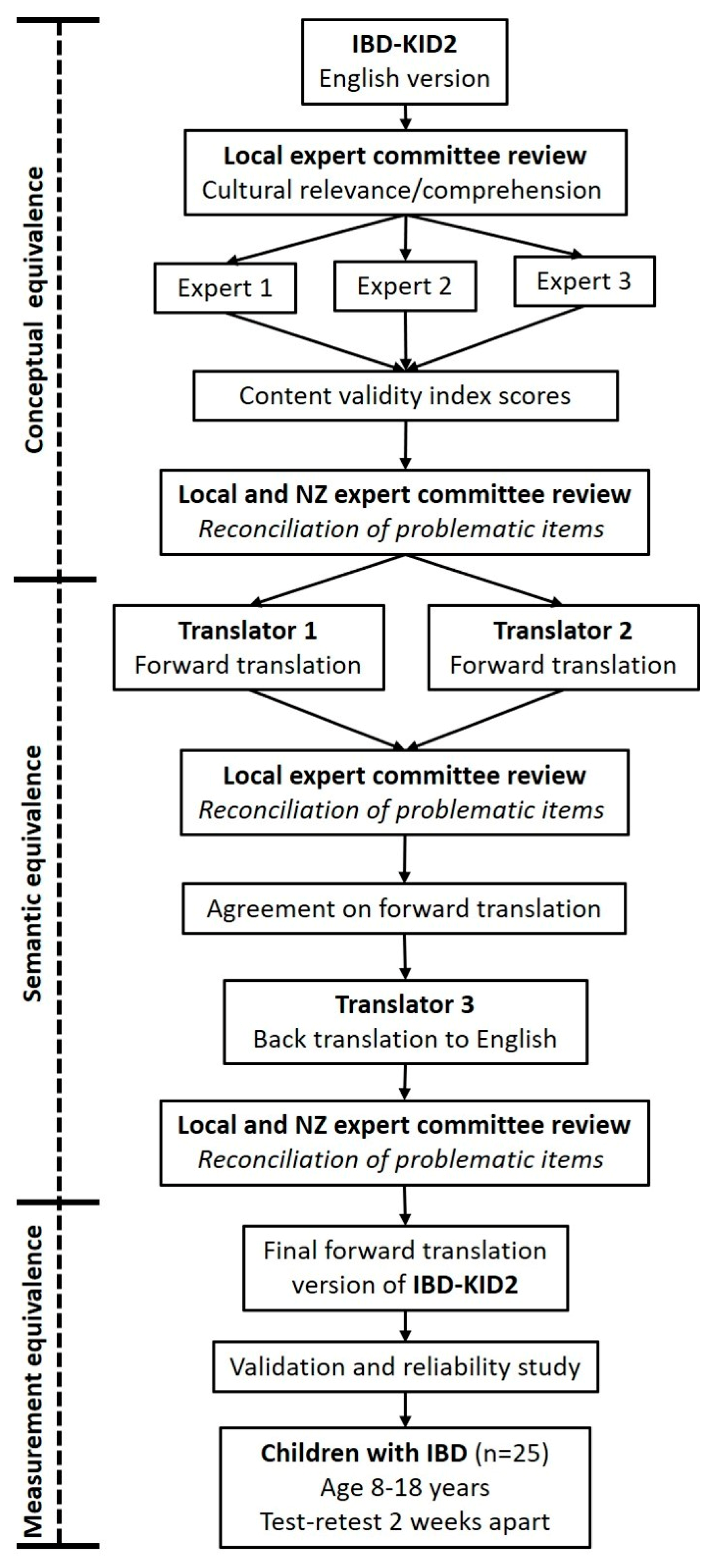
4.2. Translation Process
- Concept: the instrument is measuring the same theoretical construct in each culture.
- Content: the content of each item is relevant to the phenomenon of each culture studied
- Semantic: the meaning of items is the same in each culture after translation
- Technical: the method of assessment is comparable with respect to the data it yields.
- Criterion: the interpretation of results is the same in both cultures
4.2.1. Conceptual Equivalence
4.2.2. Semantic Equivalence
4.2.3. Measurement Equivalence
- Participants and site
- Methodology
- Ethics and consent
4.3. Statistics
4.3.1. Conceptual Equivalence
4.3.2. Measurement Equivalence
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Farrell, D.; McCarthy, G.; Savage, E. Self-reported Symptom Burden in Individuals with Inflammatory Bowel Disease. J. Crohns Colitis 2016, 10, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Sykora, J.; Pomahacova, R.; Kreslova, M.; Cvalinova, D.; Stych, P.; Schwarz, J. Current global trends in the incidence of pediatric-onset inflammatory bowel disease. World J. Gastroenterol. 2018, 24, 2741–2763. [Google Scholar] [CrossRef]
- Roberts, S.E.; Thorne, K.; Thapar, N.; Broekaert, I.; Benninga, M.A.; Dolinsek, J.; Mas, E.; Miele, E.; Orel, R.; Pienar, C.; et al. A Systematic Review and Meta-analysis of Paediatric Inflammatory Bowel Disease Incidence and Prevalence Across Europe. J. Crohns Colitis 2020, 14, 1119–1148. [Google Scholar] [CrossRef]
- Kuenzig, M.E.; Fung, S.G.; Marderfeld, L.; Mak, J.W.Y.; Kaplan, G.G.; Ng, S.C.; Wilson, D.C.; Cameron, F.; Henderson, P.; Kotze, P.G.; et al. Twenty-first Century Trends in the Global Epidemiology of Pediatric-Onset Inflammatory Bowel Disease: Systematic Review. Gastroenterology 2022, 162, 1147–1159.e1144. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.K.; Lee, Y.J.; Park, J.H. Medication-Related Knowledge and Medication Adherence in Pediatric and Adolescent Patients with Inflammatory Bowel Disease. J. Korean Med. Sci. 2020, 35, e92. [Google Scholar] [CrossRef] [PubMed]
- Hommel, K.A.; Greenley, R.N.; Maddux, M.H.; Gray, W.N.; Mackner, L.M. Self-management in pediatric inflammatory bowel disease: A clinical report of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Fishman, L.N.; Barendse, R.M.; Hait, E.; Burdick, C.; Arnold, J. Self-management of older adolescents with inflammatory bowel disease: A pilot study of behavior and knowledge as prelude to transition. Clin. Pediatr. 2010, 49, 1129–1133. [Google Scholar] [CrossRef] [PubMed]
- van Gaalen, M.A.C.; van Pieterson, M.; van den Brink, G.; de Ridder, L.; Rizopoulos, D.; van der Woude, C.J.; Escher, J.C. Rotterdam Transition Test: A Valid Tool for Monitoring Disease Knowledge in Adolescents with Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2022, 74, 60–67. [Google Scholar] [CrossRef]
- Gumidyala, P.A.; Plevinsky, M.J.; Poulopoulos, A.N.; Kahn, N.S.; Walkiewicz, N.D.; Greenley, N.R. What Teens Do Not Know Can Hurt Them: An Assessment of Disease Knowledge in Adolescents and Young Adults with IBD. Inflamm. Bowel Dis. 2017, 23, 89–96. [Google Scholar] [CrossRef]
- Krauthammer, A.; Harel, T.; Zevit, N.; Shouval, D.S.; Shamir, R.; Weiss, B. Knowledge of disease and self-management of adolescents with inflammatory bowel diseases. Acta Paediatr. 2020, 109, 2119–2124. [Google Scholar] [CrossRef]
- Vernon-Roberts, A.; Lopez, R.; Lewindon, P.; Lemberg, D.; Bowcock, N.; Alex, G.; Otley, A.; Jacobsen, K.; Evans, H.; Roberts, A.; et al. Assessment of disease-related knowledge among children with inflammatory bowel disease and their family. J. Pediatr. Gastroenterol. Nutr. Rep. 2021, 2, e093. [Google Scholar] [CrossRef]
- Vaz, K.K.H.; Carmody, J.K.; Zhang, Y.; Denson, L.A.; Hommel, K.A. Evaluation of a Novel Educational Tool in Adolescents with Inflammatory Bowel Disease: The NEAT Study. J. Pediatr. Gastroenterol. Nutr. 2019, 69, 564–569. [Google Scholar] [CrossRef]
- Vernon-Roberts, A.; Otley, A.; Frampton, C.; Gearry, R.B.; Day, A.S. Validation of a Revised Knowledge Assessment Tool for Children with Inflammatory Bowel Disease (IBD-KID2). Inflamm. Intest. Dis. 2020, 5, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Haaland, D.; Day, A.S.; Otley, A. Development and validation of a pediatric IBD knowledge inventory device: The IBD-KID. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 313–319. [Google Scholar] [CrossRef]
- Cousin, C.; Bevilacqua, C.; Roman, C.; Roquelaure, B.; Loundou, A.; Baumstarck, K.; Fabre, A. MICI-MINOTS: Linguistic and metric validation of a pediatric questionnaire on knowledge about inflammatory bowel disease. Arch. Pediatr. 2020, 27, 110–116. [Google Scholar] [CrossRef]
- Kowalska-Duplaga, K.; Gawlik-Scislo, A.; Krzesiek, E.; Jarocka-Cyrta, E.; Łazowska-Przeorek, I.; Duplaga, M.; Banaszkiewicz, A. Determinants of disease-specific knowledge among children with inflammatory bowel disease and their parents: A multicentre study. World J. Gastroenterol. WJG 2021, 27, 4468–4480. [Google Scholar] [CrossRef] [PubMed]
- Vernon-Roberts, A.; Otley, A.; Frampton, C.; Gearry, R.B.; Day, A.S. Response pattern analysis of IBD-KID: A knowledge assessment tool for children with inflammatory bowel disease. J. Paediatr. Child Health 2019, 55, 155–162. [Google Scholar] [CrossRef]
- Gill, P.S.; Jones, D. Cross-cultural adaptation of outcome measures. Eur. J. Gen. Pract. 2000, 6, 120–121. [Google Scholar] [CrossRef]
- Gjersing, L.; Caplehorn, J.R.M.; Clausen, T. Cross-cultural adaptation of research instruments: Language, setting, time and statistical considerations. BMC Med. Res. Methodol. 2010, 10, 13. [Google Scholar] [CrossRef] [PubMed]
- Povoroznyuk, R.; Dzerovych, N.; Povoroznyuk, V. A new voice: Translating medical questionnaires. J. World Lang 2016, 3, 139–159. [Google Scholar] [CrossRef]
- Epstein, J.; Santo, R.M.; Guillemin, F. A review of guidelines for cross-cultural adaptation of questionnaires could not bring out a consensus. J. Clin. Epidemiol. 2015, 68, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Dias, R. Cross-Cultural Adaptation. In Encyclopedia of Quality of Life and Well-Being Research; Michalos, A.C., Ed.; Springer: Dordrecht, The Netherlands, 2014; pp. 1363–1367. [Google Scholar] [CrossRef]
- Castro, M.; Papadatou, B.; Baldassare, M.; Balli, F.; Barabino, A.; Barbera, C.; Barca, S.; Barera, G.; Bascietto, F.; Berni Canani, R.; et al. Inflammatory bowel disease in children and adolescents in Italy: Data from the pediatric national IBD register (1996–2003). Inflamm. Bowel Dis. 2008, 14, 1246–1252. [Google Scholar] [CrossRef]
- Di Domenicantonio, R.; Cappai, G.; Arcà, M.; Agabiti, N.; Kohn, A.; Vernia, P.; Biancone, L.; Armuzzi, A.; Papi, C.; Davoli, M. Occurrence of inflammatory bowel disease in central Italy: A study based on health information systems. Dig. Liver Dis. 2014, 46, 777–782. [Google Scholar] [CrossRef] [PubMed]
- Buerkle, K.; Vernon-Roberts, A.; Ho, C.; Schultz, M.; Day, A. A Short Knowledge Assessment Tool Is Valid and Acceptable for Adults with Inflammatory Bowel Disease. Dig. Dis. Sci. 2022, 67, 2049–2058. [Google Scholar] [CrossRef]
- Sassatelli, R. Introduction: Food, Foodways and Italianicity. In Italians and Food; Sassatelli, R., Ed.; Springer International Publishing: Cham, Switzerland, 2019; pp. 1–15. [Google Scholar] [CrossRef]
- Diederen, K.; Krom, H.; Koole, J.C.D.; Benninga, M.A.; Kindermann, A. Diet and Anthropometrics of Children With Inflammatory Bowel Disease: A Comparison With the General Population. Inflamm. Bowel Dis. 2018, 24, 1632–1640. [Google Scholar] [CrossRef]
- Bramuzzo, M.; Grazian, F.; Grigoletto, V.; Daidone, A.; Martelossi, S.; Mario, F.; Maurel, E.; Lega, S.; Giudici, F.; Di Leo, G.; et al. Dietary beliefs in children and adolescents with inflammatory bowel disease and their parents. J. Pediatr. Gastroenterol. Nutr. 2022, 75, e43–e48. [Google Scholar] [CrossRef] [PubMed]
- Diederen, K.; Hoekman, D.R.; Hummel, T.Z.; Meij, T.G.; Koot, B.G.P.; Tabbers, M.M.; Vlieger, A.M.; Kindermann, A.; Benninga, M.A. The prevalence of irritable bowel syndrome-type symptoms in paediatric inflammatory bowel disease, and the relationship with biochemical markers of disease activity. Aliment. Pharm. Ther. 2016, 44, 181–188. [Google Scholar] [CrossRef]
- Hughes, L.D.; King, L.; Morgan, M.; Ayis, S.; Direkze, N.; Lomer, M.C.; Lindsay, J.O.; Whelan, K. Food-related Quality of Life in Inflammatory Bowel Disease: Development and Validation of a Questionnaire. J. Crohns Colitis 2016, 10, 194–201. [Google Scholar] [CrossRef]
- Brown, S.C.; Whelan, K.; Frampton, C.; Wall, C.L.; Gearry, R.B.; Day, A.S. Food-Related Quality of Life in Children and Adolescents With Crohn’s Disease. Inflamm. Bowel Dis. 2022, 28, 1838–1843. [Google Scholar] [CrossRef]
- Vernon-Roberts, A.; Gearry, R.; Day, A. Assessment of knowledge levels following an education program for parents of children with inflammatory bowel disease. Front. Pediatr. 2020, 8, 475. [Google Scholar] [CrossRef]
- Kilby, K.; Mathias, H.; Boisvenue, L.; Heisler, C.; Jones, J.L. Micronutrient absorption and related outcomes in people with inflammatory bowel disease: A review. Nutrients 2019, 11, 1388. [Google Scholar] [CrossRef] [PubMed]
- Day, A.S.; Lemberg, D.A.; Nichol, A.; Clarkson, C.; Otley, A.R. Generalisability of the inflammatory bowel disease knowledge inventory device to assess disease-related knowledge in Australian children. J. Paediatr. Child Health 2014, 50, 591–595. [Google Scholar] [CrossRef]
- Day, A.S.; Mylvaganam, G.; Shalloo, N.; Clarkson, C.; Leach, S.T.; Lemberg, D.A. Assessment of disease-specific knowledge in Australian children with inflammatory bowel disease and their parents. J. Paediatr. Child Health 2017, 53, 778. [Google Scholar] [CrossRef]
- Beck, C.T.; Bernal, H.; Froman, R.D. Methods to document semantic equivalence of a translated scale. Res. Nurs. Health 2003, 26, 64–73. [Google Scholar] [CrossRef] [PubMed]
- Flaherty, A.J.; Gaviria, M.F.; Pathak, A.D.; Mitchell, A.T.; Wintrob, A.R.; Richman, A.J.; Birz, A.S. Developing Instruments for Cross-Cultural Psychiatric Research. J. Nerv. Ment. Dis. 1988, 176, 260–263. [Google Scholar] [CrossRef]
- Kassam-Adams, N.; Marsac, M.L.; Kohser, K.L.; Kenardy, J.A.; March, S.; Winston, F.K. A new method for assessing content validity in model-based creation and iteration of eHealth interventions. J. Med. Internet Res. 2015, 17, e95. [Google Scholar] [CrossRef]
- Polit, D.; Beck, C. The content validity index: Are you sure you know what’s being reported? critique and recommendations. Res. Nurs. Health 2006, 29, 489–497. [Google Scholar] [CrossRef] [PubMed]
- IBM SPSS Statistics for Windows; Version 27.0; IBM Corp.: Armonk, NY, USA, 2020.
| Item # | Relevance | Comprehension |
|---|---|---|
| 1 | 0.73 | 0.93 |
| 2 | 0.63 | 0.57 |
| 3 | 0.83 | 0.93 |
| 4 | 0.90 | 0.73 |
| 5 | 0.90 | 0.83 |
| 6 | 0.73 | 0.80 |
| 7 | 0.93 | 0.93 |
| 8 | 0.93 | 0.93 |
| 9 | 0.97 | 0.97 |
| 10 | 0.93 | 0.97 |
| 11 | 0.70 | 0.77 |
| 12 | 0.97 | 0.97 |
| 13 | 0.80 | 0.77 |
| 14 | 0.97 | 0.97 |
| 15 | 0.70 | 0.67 |
| Overall score | 0.84 | 0.85 |
| Linear Variable | R | p Value |
|---|---|---|
| Age | 0.267 | 0.198 |
| Time since diagnosis | 0.108 | 0.607 |
| Age at diagnosis | 0.075 | 0.723 |
| Categorical variable | Mean difference | p value |
| Age group (all) | - | 0.255 |
| Age group (<16 y vs. ≥16 y) | −0.46 | 0.691 |
| Gender | 1.4 | 0.222 |
| IBD sub-type | −1.51 | 0.177 |
| Family history of IBD | 2.04 | 0.235 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vernon-Roberts, A.; Musto, F.; Aloi, M.; Day, A.S. Italian Cross-Cultural Adaptation of a Knowledge Assessment Tool (IBD-KID2) for Children with Inflammatory Bowel Disease. Gastrointest. Disord. 2023, 5, 187-197. https://doi.org/10.3390/gidisord5020016
Vernon-Roberts A, Musto F, Aloi M, Day AS. Italian Cross-Cultural Adaptation of a Knowledge Assessment Tool (IBD-KID2) for Children with Inflammatory Bowel Disease. Gastrointestinal Disorders. 2023; 5(2):187-197. https://doi.org/10.3390/gidisord5020016
Chicago/Turabian StyleVernon-Roberts, Angharad, Francesca Musto, Marina Aloi, and Andrew S. Day. 2023. "Italian Cross-Cultural Adaptation of a Knowledge Assessment Tool (IBD-KID2) for Children with Inflammatory Bowel Disease" Gastrointestinal Disorders 5, no. 2: 187-197. https://doi.org/10.3390/gidisord5020016
APA StyleVernon-Roberts, A., Musto, F., Aloi, M., & Day, A. S. (2023). Italian Cross-Cultural Adaptation of a Knowledge Assessment Tool (IBD-KID2) for Children with Inflammatory Bowel Disease. Gastrointestinal Disorders, 5(2), 187-197. https://doi.org/10.3390/gidisord5020016



.png)




