Anticipation of Stress and Relaxation Dynamically Impacts Sleep
Abstract
1. Introduction
2. Results
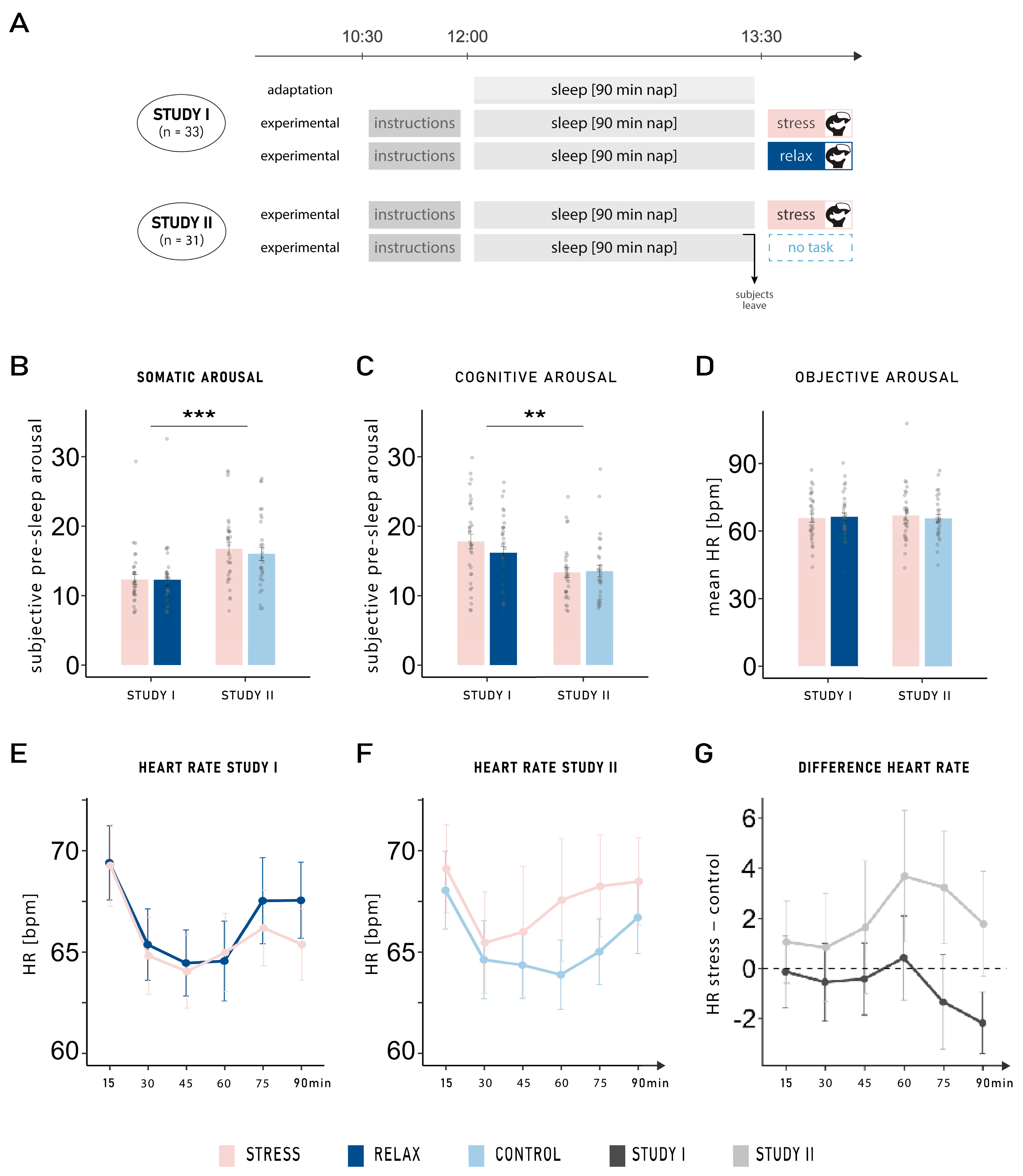
2.1. Subjective and Objective Pre-Sleep Arousal
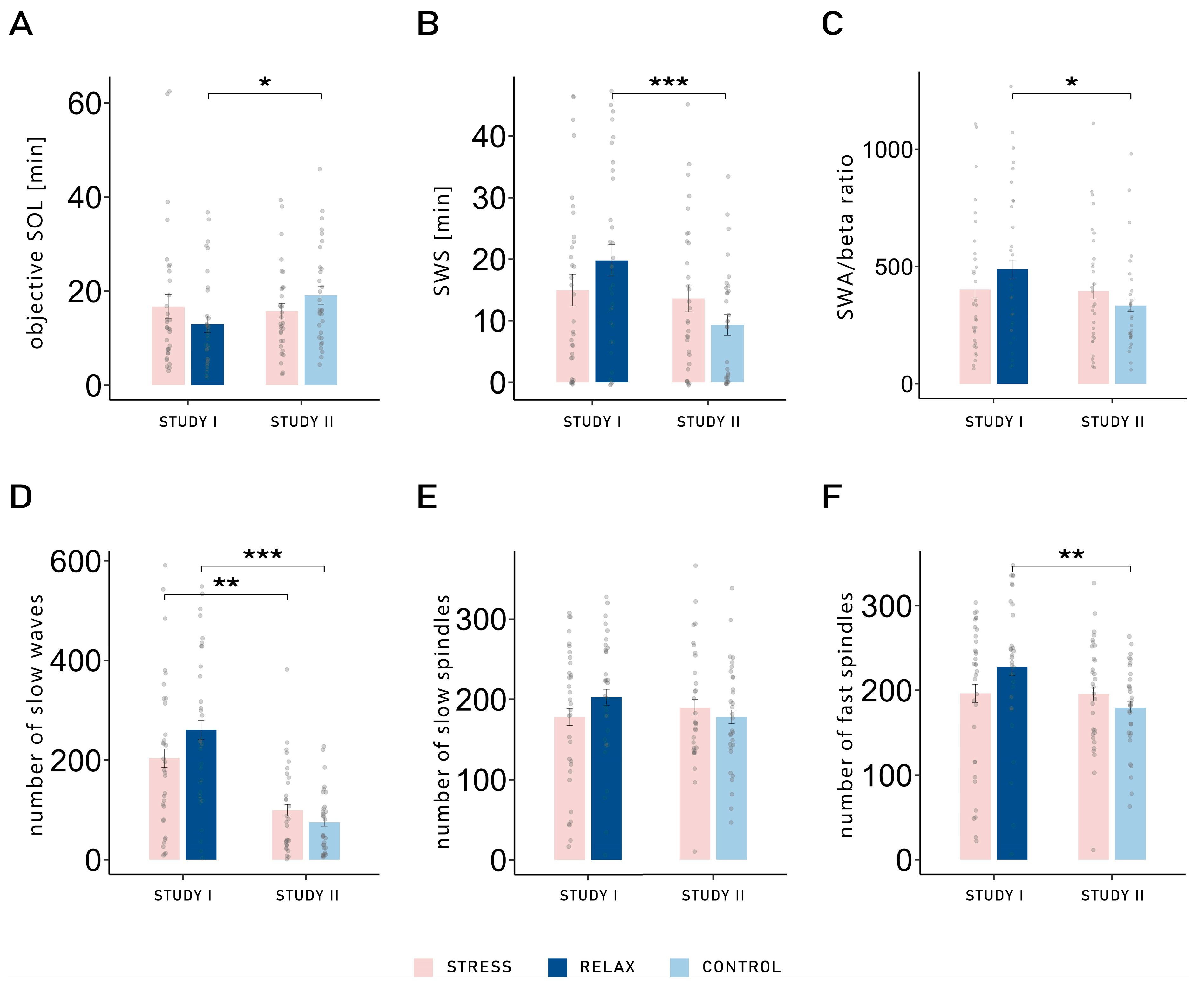
2.2. Sleep Architecture
2.3. Slow Waves and Sleep Spindles
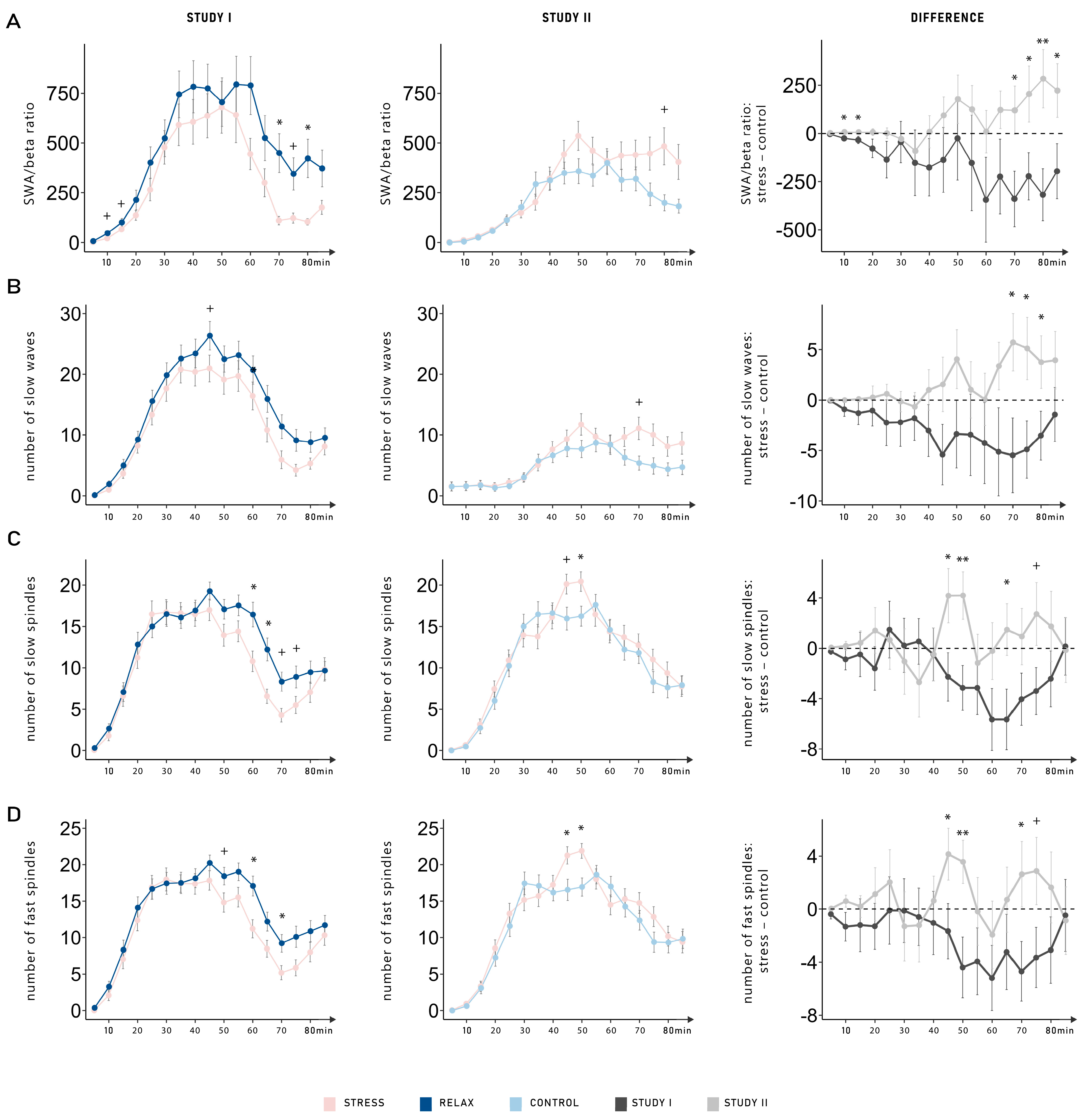
2.4. Dynamic Changes of SWA/Beta Power Ratio, Slow Waves, and Sleep Spindles
3. Discussion
4. Materials and Methods
4.1. Participants
4.2. Design and Procedure
4.3. Stressful Tasks in Virtual Reality
4.4. Questionnaires
4.5. EEG Recording
4.6. Preprocessing and Artifact Rejection
4.7. Power Analysis and Slow Wave and Spindle Detection
4.8. Electrocardiography
4.9. Statistical Analyses
4.10. Preregistration
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kogler, L.; Mueller, V.I.; Chang, A.; Eickhoff, S.B.; Fox, P.T.; Gur, R.C.; Derntl, B. Psychosocial versus physiological stress—Meta-analyses on deactivations and activations of the neural correlates of stress reactions. Neuroimage 2015, 119, 235–251. [Google Scholar] [CrossRef]
- Campbell, J.; Ehlert, U. Acute psychosocial stress: Does the emotional stress response correspond with physiological responses? Psychoneuroendocrinology 2012, 37, 1111–1134. [Google Scholar] [CrossRef]
- Tang, N.K.Y.; Harvey, A.G. Effects of Cognitive Arousal and Physiological Arousal on Sleep Perception. Sleep 2004, 27, 69–78. [Google Scholar] [CrossRef]
- Wuyts, J.; De Valck, E.; Vandekerckhove, M.; Pattyn, N.; Bulckaert, A.; Berckmans, D.; Haex, B.; Verbraecken, J.; Cluydts, R. The influence of pre-sleep cognitive arousal on sleep onset processes. Int. J. Psychophysiol. 2012, 83, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Âkerstedt, T. Psychosocial stress and impaired sleep. Scand. J. Work Environ. Health 2006, 32, 493–501. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, Z.; Thomas, K.G.F.; Lipinska, G. Bedtime Stress Increases Sleep Latency and Impairs Next-Day Prospective Memory Performance. Front. Neurosci. 2020, 14, 756. [Google Scholar] [CrossRef]
- Beck, J.; Loretz, E.; Rasch, B. Stress dynamically reduces sleep depth: Temporal proximity to the stressor is crucial. Cereb. Cortex 2023, 33, 96–113. [Google Scholar] [CrossRef]
- Beck, J.; Cordi, M.J.; Rasch, B. Hypnotic Suggestions Increase Slow-Wave Parameters but Decrease Slow-Wave Spindle Coupling. Nat. Sci. Sleep 2021, 13, 1383–1393. [Google Scholar] [CrossRef]
- Koroma, M.; Beck, J.; Schmidt, C.; Rasch, B.; Demertzi, A. Probing the embodiment of sleep functions: Insights from cardiac responses to word-induced relaxation during sleep. J. Sleep Res. 2024, 33, e14160. [Google Scholar] [CrossRef] [PubMed]
- Kirschbaum, C.; Pirke, K.M.; Hellhammer, D.H. The ’Trier Social Stress Test’—A tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology 1993, 28, 76–81. [Google Scholar] [CrossRef]
- Mölle, M.; Marshall, L.; Gais, S.; Born, J. Grouping of Spindle Activity during Slow Oscillations in Human Non-Rapid Eye Movement Sleep. J. Neurosci. 2002, 22, 10941–10947. [Google Scholar] [CrossRef]
- Casey, A.H. Contrast Effects. In Encyclopedia of Animal Cognition and Behavior; Springer: Cham, Switzerland, 2022; pp. 1673–1675. [Google Scholar] [CrossRef]
- Elder, G.J.; Barclay, N.L.; Wetherell, M.A.; Ellis, J.G. Anticipated next-day demand affects the magnitude of the cortisol awakening response, but not subjective or objective sleep. J. Sleep Res. 2018, 27, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Sprajcer, M.; Jay, S.M.; Vincent, G.E.; Vakulin, A.; Lack, L.; Ferguson, S.A. The effects of anticipating a high-stress task on sleep and performance during simulated on-call work. J. Sleep Res. 2018, 27, e12691. [Google Scholar] [CrossRef] [PubMed]
- Kalmbach, D.A.; Buysse, D.J.; Cheng, P.; Roth, T.; Yang, A.; Drake, C.L. Nocturnal cognitive arousal is associated with objective sleep disturbance and indicators of physiologic hyperarousal in good sleepers and individuals with insomnia disorder. Sleep Med. 2020, 71, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Van Dalfsen, J.H.; Markus, C.R. The influence of sleep on human hypothalamic–pituitary–adrenal (HPA) axis reactivity: A systematic review. Sleep Med. Rev. 2018, 39, 187–194. [Google Scholar] [CrossRef]
- Baker, F.C.; Lee, K.A. Menstrual Cycle Effects on Sleep. Sleep Med. Clin. 2022, 17, 283–294. [Google Scholar] [CrossRef]
- Driver, H.S.; Werth, E.; Dijk, D.-J.; Borbély, A.A. The Menstrual Cycle Effects on Sleep. Sleep Med. Clin. 2008, 3, 1–11. [Google Scholar] [CrossRef]
- Shechter, A.; Boivin, D.B. Sleep, Hormones, and Circadian Rhythms throughout the Menstrual Cycle in Healthy Women and Women with Premenstrual Dysphoric Disorder. Int. J. Endocrinol. 2010, 2010, 259345. [Google Scholar] [CrossRef]
- Blanaru, M.; Bloch, B.; Vadas, L.; Arnon, Z.; Ziv, N.; Kremer, I.; Haimov, I. The effects of music relaxation and muscle relaxation techniques on sleep quality and emotional measures among individuals with posttraumatic stress disorder. Ment. Illn. 2012, 4, 59–65. [Google Scholar] [CrossRef]
- De Niet, G.; Tiemens, B.; Lendemeijer, B.; Hutschemaekers, G. Music-assisted relaxation to improve sleep quality: Meta-analysis. J. Adv. Nurs. 2009, 65, 1356–1364. [Google Scholar] [CrossRef]
- Liu, K.; Chen, Y.; Wu, D.; Lin, R.; Wang, Z.; Pan, L. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement. Ther. Clin. Pract. 2020, 39, 101132. [Google Scholar] [CrossRef]
- Baselgia, S.; Combertaldi, S.L.; Fahr, A.; Wirz, D.S.; Ort, A.; Rasch, B. Pre-sleep arousal induced by suspenseful series and cliffhangers have only minor effects on sleep: A sleep laboratory study. Sleep Med. 2023, 102, 186–198. [Google Scholar] [CrossRef]
- Cordi, M.J.; Rossier, L.; Rasch, B. Hypnotic Suggestions Given Before Nighttime Sleep Extend Slow-Wave Sleep as Compared to a Control Text in Highly Hypnotizable Subjects. Int. J. Clin. Exp. Hypn. 2020, 68, 105–129. [Google Scholar] [CrossRef]
- Brodt, S.; Inostroza, M.; Niethard, N.; Born, J. Sleep—A brain-state serving systems memory consolidation. Neuron 2023, 111, 1050–1075. [Google Scholar] [CrossRef]
- Rasch, B.; Born, J. About Sleep’s Role in Memory. Physiol. Rev. 2013, 93, 681–766. [Google Scholar] [CrossRef] [PubMed]
- Stewart-Williams, S.; Podd, J. The Placebo Effect: Dissolving the Expectancy Versus Conditioning Debate. Psychol. Bull. 2004, 130, 324–340. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Wei, H.; Zhang, H.; Li, X.; Bo, C.; Wan, L.; Lu, X.; Hu, L. The Influence of Expectancy Level and Personal Characteristics on Placebo Effects: Psychological Underpinnings. Front. Psychiatry 2019, 10, 20. [Google Scholar] [CrossRef]
- Allen, A.P.; Kennedy, P.J.; Dockray, S.; Cryan, J.F.; Dinan, T.G.; Clarke, G. The Trier Social Stress Test: Principles and practice. Neurobiol. Stress 2017, 6, 113–126. [Google Scholar] [CrossRef]
- Liszio, S.; Graf, L.; Masuch, M. The Relaxing Effect of Virtual Nature: Immersive Technology Provides Relief in Acute Stress Situations. Annu. Rev. Cyberther. Telemed. 2018, 16, 87–93. [Google Scholar]
- Zimmer, P.; Buttlar, B.; Halbeisen, G.; Walther, E.; Domes, G. Virtually stressed? A refined virtual reality adaptation of the Trier Social Stress Test (TSST) induces robust endocrine responses. Psychoneuroendocrinology 2019, 101, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Nicassio, P.M.; Mendlowitz, D.R.; Fussell, J.J.; Petras, L. The phenomenology of the pre-sleep state: The development of the pre-sleep arousal scale. Behav. Res. Ther. 1985, 23, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Görtelmeyer, R. SF-A/R und SF-B/R—Schlaffragebogen A und B; Hogrefe: Göttingen, Germany, 2011. [Google Scholar]
- Iber, C.; Ancoli-Israel, S.; Chesson, A.L.; Quan, S.F. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications; American Academy of Sleep Medicine: Westchester, IL, USA, 2007; Volume 1. [Google Scholar]
- Perslev, M.; Darkner, S.; Kempfner, L.; Nikolic, M.; Jennum, P.J.; Igel, C. U-Sleep: Resilient high-frequency sleep staging. npj Digit. Med. 2021, 4, 72. [Google Scholar] [CrossRef] [PubMed]
- Oostenveld, R.; Fries, P.; Maris, E.; Schoffelen, J.-M. FieldTrip: Open Source Software for Advanced Analysis of MEG, EEG, and Invasive Electrophysiological Data. Comput. Intell. Neurosci. 2011, 2011, 156869. [Google Scholar] [CrossRef]
- Maes, J.; Verbraecken, J.; Willemen, M.; De Volder, I.; van Gastel, A.; Michiels, N.; Verbeek, I.; Vandekerckhove, M.; Wuyts, J.; Exadaktylos, V.; et al. Sleep misperception, EEG characteristics and Autonomic Nervous System activity in primary insomnia: A retrospective study on polysomnographic data. Int. J. Psychophysiol. Off. J. Int. Organ. Psychophysiol. 2014, 91, 163–171. [Google Scholar] [CrossRef]
- Tarvainen, M.P.; Niskanen, J.-P.; Lipponen, J.A.; Ranta-aho, P.O.; Karjalainen, P.A. Kubios HRV—Heart rate variability analysis software. Comput. Methods Programs Biomed. 2014, 113, 210–220. [Google Scholar] [CrossRef] [PubMed]
| Study I Anticipated Stress vs. Relaxation | Study II Anticipated Stress vs. Neutral Control | Main Effect of Study | Main Effect of Condition | Interaction Effect | ||||||
| Stress | Control | Stress | Control | p | η2 | p | η2 | p | η2 | |
| Subjective Sleep Parameters | ||||||||||
| Cognitive PSA | 17.82 ± 1.03 | 16.18 ± 0.91 | 13.32 ± 0.72 | 13.52 ± 0.83 | 0.002 | 0.12 | 0.214 | <0.01 | 0.117 | <0.01 |
| Somatic PSA | 12.33 ± 0.70 | 12.27 ± 0.80 | 16.74 ± 0.90 | 16.03 ± 0.94 | <0.001 | 0.16 | 0.450 | <0.01 | 0.524 | <0.01 |
| Sleep Quality | 3.56 ± 0.14 | 3.57 ± 0.13 | 3.71 ± 0.12 | 3.65 ± 0.11 | 0.416 | <0.01 | 0.785 | <0.01 | 0.729 | <0.01 |
| SOL | 23.18 ± 1.93 | 20.45 ± 1.97 | 25.16 ± 1.97 | 22.58 ± 1.70 | 0.352 | <0.01 | 0.096 | 0.02 | 0.963 | <0.01 |
| Objective Sleep Parameters | ||||||||||
| SOL [min] | 16.76 ± 2.57 | 12.94 ± 1.74 | 15.76 ± 1.67 | 19.15 ± 1.88 | 0.308 | 0.01 | 0.869 | <0.01 | 0.007 | 0.03 |
| WASO [%] | 9.93 ± 2.63 | 5.74 ± 1.93 | 8.10 ± 1.54 | 6.79 ± 1.86 | 0.857 | <0.01 | 0.163 | 0.01 | 0.463 | <0.01 |
| N1 [%] | 20.05 ± 2.75 | 17.07 ± 2.22 | 9.63 ± 1.13 | 11.30 ± 1.49 | 0.003 | 0.11 | 0.595 | <0.01 | 0.064 a | 0.01 |
| N2 [%] | 37.82 ± 2.61 | 39.70 ± 2.57 | 44.92 ± 3.24 | 50.96 ± 3.55 | 0.015 | 0.07 | 0.064 a | 0.01 | 0.324 | <0.01 |
| SWS [%] | 20.55 ± 3.14 | 26.23 ± 3.20 | 18.40 ± 3.37 | 12.21 ± 2.28 | 0.024 | 0.05 | 0.918 | <0.01 | 0.020 | 0.03 |
| REM [%] | 11.64 ± 1.71 | 11.27 ± 1.77 | 12.55 ± 2.17 | 12.37 ± 2.54 | 0.656 | <0.01 | 0.882 | <0.01 | 0.959 | <0.01 |
| TST [min] | 63.67 ± 3.48 | 68.30 ± 3.16 | 64.81 ± 3.00 | 61.68 ± 2.96 | 0.472 | <0.01 | 0.754 | <0.01 | 0.110 | 0.01 |
| WASO [min] | 7.18 ± 1.89 | 3.36 ± 0.85 | 5.84 ± 1.05 | 4.69 ± 1.20 | 0.996 | <0.01 | 0.055 a | 0.03 | 0.297 | <0.01 |
| N1 [min] | 13.14 ± 1.64 | 11.26 ± 1.35 | 7.35 ± 0.80 | 7.55 ± 0.82 | 0.003 | 0.11 | 0.335 | <0.01 | 0.236 | <0.01 |
| N2 [min] | 26.50 ± 2.21 | 28.50 ± 2.07 | 33.95 ± 2.37 | 35.21 ± 1.52 | 0.004 | 0.09 | 0.351 | <0.01 | 0.831 | <0.01 |
| SWS [min] | 14.97 ± 2.52 | 19.80 ± 2.56 | 13.79 ± 2.23 | 9.40 ± 1.71 | 0.036 | 0.05 | 0.903 | <0.01 | 0.014 | 0.03 |
| REM [min] | 9.06 ± 1.38 | 8.74 ± 1.42 | 9.71 ± 1.70 | 9.45 ± 1.92 | 0.699 | <0.01 | 0.844 | <0.01 | 0.984 | <0.01 |
| Study I Anticipated Stress vs. Relaxation | Study II Anticipated Stress vs. Neutral Control | Main Effect of Study | Main Effect of Condition | Interaction Effect | In 5-Min Segments: Interaction Effect | |||||||
| Stress | Control | Stress | Control | p | η2 | p | η2 | p | η2 | p | η2 | |
| SWA/beta ratio in frontal area | ||||||||||||
| 402.36 ± 35.64 | 487.45 ± 40.61 | 395.81 ± 33.63 | 334.60 ± 27.12 | 0.187 | 0.02 | 0.743 | <0.01 | 0.048 | 0.02 | 0.018 | 0.01 | |
| Slow waves in frontal area | ||||||||||||
| Count | 203.94 ± 18.90 | 260.82 ± 19.00 | 99.31 ± 11.25 | 75.42 ± 8.09 | <0.001 | 0.26 | 0.255 | <0.01 | 0.007 | 0.03 | 0.005 | <0.01 |
| Amplitude | 138.27 ± 4.30 | 144.79 ± 4.31 | 83.75 ± 2.19 | 83.14 ± 2.02 | <0.001 | 0.54 | 0.237 | <0.01 | 0.154 | <0.01 | 0.005 | <0.01 |
| Density | 2.29 ± 0.14 | 2.63 ± 0.14 | 1.02 ± 0.10 | 0.83 ± 0.07 | <0.001 | 0.42 | 0.538 | <0.01 | 0.023 | 0.02 | 0.005 | <0.01 |
| Duration | 1.25 ± 0.01 | 1.25 ± 0.01 | 1.70 ± 0.01 | 1.73 ± 0.01 | <0.001 | 0.94 | 0.050 | 0.01 | 0.033 | 0.01 | 0.011 | <0.01 |
| Up-slope | 381.44 ± 14.44 | 386.66 ± 14.67 | 109.94 ± 2.98 | 109.31 ± 2.83 | <0.001 | 0.73 | 0.771 | <0.01 | 0.711 | <0.01 | 0.027 | <0.01 |
| Down-slope | −365.17 ± 11.88 | −388.86 ± 13.86 | −102.99 ± 2.97 | −102.55 ± 2.76 | <0.001 | 0.77 | 0.065 a | <0.01 | 0.056 a | <0.01 | 0.011 | <0.01 |
| Slow spindles in frontal area | ||||||||||||
| Count | 178.36 ± 10.70 | 202.70 ± 9.68 | 190.00 ± 9.48 | 178.21 ± 8.55 | 0.703 | <0.01 | 0.523 | <0.01 | 0.069 a | 0.01 | 0.034 | <0.01 |
| Amplitude | 30.56 ± 0.73 | 30.77 ± 0.86 | 28.44 ± 0.87 | 29.93 ± 0.99 | 0.349 | 0.01 | 0.210 | <0.01 | 0.343 | <0.01 | 0.078 a | <0.01 |
| Density | 2.25 ± 0.06 | 2.19 ± 0.05 | 2.17 ± 0.08 | 2.16 ± 0.06 | 0.647 | <0.01 | 0.518 | <0.01 | 0.600 | <0.01 | 0.023 | <0.01 |
| Duration | 0.87 ± 0.01 | 0.86 ± 0.01 | 0.84 ± 0.01 | 0.85 ± 0.01 | 0.284 | 0.02 | 0.845 | <0.01 | 0.295 | <0.01 | 0.048 | <0.01 |
| Fast spindles in parietal area | ||||||||||||
| Count | 196.27 ± 10.69 | 227.27 ± 10.09 | 195.32 ± 8.32 | 179.84 ± 6.65 | 0.125 | 0.03 | 0.426 | <0.01 | 0.019 | 0.03 | 0.022 | <0.01 |
| Amplitude | 25.83 ± 0.73 | 25.81 ± 0.86 | 18.69 ± 0.74 | 19.20 ± 0.60 | <0.001 | 0.27 | 0.547 | <0.01 | 0.522 | <0.01 | 0.023 | <0.01 |
| Density | 2.50 ± 0.04 | 2.47 ± 0.04 | 2.22 ± 0.05 | 2.25 ± 0.06 | 0.004 | 0.11 | 0.882 | <0.01 | 0.438 | <0.01 | 0.016 | <0.01 |
| Duration | 0.90 ± 0.01 | 0.90 ± 0.01 | 0.86 ± 0.01 | 0.87 ± 0.01 | 0.075 a | 0.04 | 0.853 | <0.01 | 0.242 | <0.01 | 0.056 a | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baselgia, S.; Beck, J.; Rasch, B. Anticipation of Stress and Relaxation Dynamically Impacts Sleep. Clocks & Sleep 2025, 7, 68. https://doi.org/10.3390/clockssleep7040068
Baselgia S, Beck J, Rasch B. Anticipation of Stress and Relaxation Dynamically Impacts Sleep. Clocks & Sleep. 2025; 7(4):68. https://doi.org/10.3390/clockssleep7040068
Chicago/Turabian StyleBaselgia, Sandrine, Jonas Beck, and Björn Rasch. 2025. "Anticipation of Stress and Relaxation Dynamically Impacts Sleep" Clocks & Sleep 7, no. 4: 68. https://doi.org/10.3390/clockssleep7040068
APA StyleBaselgia, S., Beck, J., & Rasch, B. (2025). Anticipation of Stress and Relaxation Dynamically Impacts Sleep. Clocks & Sleep, 7(4), 68. https://doi.org/10.3390/clockssleep7040068






