Sleep Health Inequities: Sociodemographic, Psychosocial, and Structural Determinants of Short Sleep in U.S. Adults
Abstract
1. Introduction
2. Results
2.1. Sample Characteristics
2.2. Bivariate Distributions
2.3. Multivariable Associations
2.3.1. Sociodemographic and Psychosocial Predictors
2.3.2. Economic and Behavioral Predictors
3. Discussion
4. Materials and Methods
4.1. Data Source and Study Population
4.2. Measures
4.2.1. Sleep Duration
4.2.2. Sociodemographic Characteristics
4.2.3. Psychosocial Factors
4.2.4. Economic and Behavioral Factors
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| AASM | American Academy of Sleep Medicine |
| AI/AN | American Indian/Alaska Native |
| AOR | Adjusted Odds Ratio |
| BMJ | British Medical Journal |
| BRFSS | Behavioral Risk Factor Surveillance System |
| CDC | Centers for Disease Control and Prevention |
| CI | Confidence Interval |
| HPA | Hypothalamic–Pituitary–Adrenal (axis) |
| HRSN | Health-Related Social Needs |
| HS | High School |
| JAMA | Journal of the American Medical Association |
| LLCPWT | Landline/Cell Phone Weight (BRFSS survey weight) |
| NHIS | National Health Interview Survey |
| OR | Odds Ratio |
| PSU | Primary Sampling Unit |
| REM | Rapid Eye Movement (sleep) |
| SPSS | Statistical Package for the Social Sciences |
| STSTR | Stratum (BRFSS survey stratum) |
| U.S. | United States |
References
- DelRosso, L.M. Global Perspectives on Sleep Health: Definitions, Disparities, and Implications for Public Health. Brain Sci. 2025, 15, 304. [Google Scholar] [CrossRef]
- Ramar, K.; Malhotra, R.K.; Carden, K.A.; Martin, J.L.; Abbasi-Feinberg, F.; Aurora, R.N.; Kapur, V.K.; Olson, E.J.; Rosen, C.L.; Rowley, J.A.; et al. Sleep is essential to health: An American Academy of Sleep Medicine position statement. J. Clin. Sleep Med. 2021, 17, 2115–2119. [Google Scholar] [CrossRef] [PubMed]
- Gottlieb, D.J. The Sleep Heart Health Study: A progress report. Curr. Opin. Pulm. Med. 2008, 14, 537–542. [Google Scholar] [CrossRef]
- Kecklund, G.; Axelsson, J. Health consequences of shift work and insufficient sleep. BMJ 2016, 355, i5210. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.; Al-Jahdali, H. The consequences of sleep deprivation on cognitive performance. Neurosciences 2023, 28, 91–99. [Google Scholar] [CrossRef]
- Depner, C.M.; Stothard, E.R.; Wright, K.P., Jr. Metabolic consequences of sleep and circadian disorders. Curr. Diabetes Rep. 2014, 14, 507. [Google Scholar] [CrossRef]
- Curcio, G.; Ferrara, M.; De Gennaro, L. Sleep loss, learning capacity and academic performance. Sleep Med. Rev. 2006, 10, 323–337. [Google Scholar] [CrossRef]
- Hafner, M.; Stepanek, M.; Taylor, J.; Troxel, W.M.; van Stolk, C. Why Sleep Matters-The Economic Costs of Insufficient Sleep: A Cross-Country Comparative Analysis. RAND Health Q. 2017, 6, 11. [Google Scholar]
- Chattu, V.K.; Chattu, S.K.; Spence, D.W.; Manzar, M.D.; Burman, D.; Pandi-Perumal, S.R. Do Disparities in Sleep Duration Among Racial and Ethnic Minorities Contribute to Differences in Disease Prevalence? J. Racial Ethn. Health Disparities 2019, 6, 1053–1061. [Google Scholar] [CrossRef] [PubMed]
- Jackson, C.L.; Redline, S.; Emmons, K.M. Sleep as a potential fundamental contributor to disparities in cardiovascular health. Annu. Rev. Public Health 2015, 36, 417–440. [Google Scholar] [CrossRef]
- Billings, M.E.; Hale, L.; Johnson, D.A. Physical and Social Environment Relationship with Sleep Health and Disorders. Chest 2020, 157, 1304–1312. [Google Scholar] [CrossRef]
- Hansen, M.; Simon, K.R.; Strack, J.; He, X.; Noble, K.G.; Merz, E.C. Socioeconomic disparities in sleep duration are associated with cortical thickness in children. Brain Behav. 2023, 13, e2859. [Google Scholar] [CrossRef]
- Seo, S.; Mattos, M.K. The relationship between social support and sleep quality in older adults: A review of the evidence. Arch. Gerontol. Geriatr. 2024, 117, 105179. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Wang, R.X.; Bian, C.; Liu, F.Y.; Tang, M.W.; Zhang, Y.H. Sleep quality, psychological resilience, family resilience, social support, and mental disability in patients with chronic schizophrenia: A cross-sectional study. Schizophr. Res. 2024, 274, 199–205. [Google Scholar] [CrossRef]
- Gyasi, R.M.; Osei-Amankwah, L.; Nyamadi, V.M.; Kenney, C.K.; Frempong, F.; Peprah, P.; Amoako, G.K.; Adam, A.M.; Hajek, A. Financial inclusion and sleep problems in later stages of life: Estimating mediation by emotional pain and food insecurity. Aging Ment. Health 2025, 1–11. [Google Scholar] [CrossRef]
- Remington, P.L. The Behavioral Risk Factor Public Health Surveillance System. Am. J. Prev. Med. 2020, 59, 776–778. [Google Scholar] [CrossRef]
- Pankowska, M.M.; Lu, H.; Wheaton, A.G.; Liu, Y.; Lee, B.; Greenlund, K.J.; Carlson, S.A. Prevalence and Geographic Patterns of Self-Reported Short Sleep Duration Among US Adults, 2020. Prev. Chronic Dis. 2023, 20, E53. [Google Scholar] [CrossRef]
- Caraballo, C.; Mahajan, S.; Valero-Elizondo, J.; Massey, D.; Lu, Y.; Roy, B.; Riley, C.; Annapureddy, A.R.; Murugiah, K.; Elumn, J.; et al. Evaluation of Temporal Trends in Racial and Ethnic Disparities in Sleep Duration Among US Adults, 2004–2018. JAMA Netw. Open 2022, 5, e226385. [Google Scholar] [PubMed]
- Groeger, J.A.; Hepsomali, P. Social Deprivation and Ethnicity Are Associated with More Problematic Sleep in Middle-Aged and Older Adults. Clocks Sleep 2023, 5, 399–413. [Google Scholar] [CrossRef]
- Pabayo, R.; Patel, P.; Liu, S.Y.; Molnar, B.E. Sleepless in inequality: Findings from the 2018 behavioral risk factor surveillance system, a cross-sectional study. BMC Public Health 2022, 22, 1973. [Google Scholar] [CrossRef]
- Nyarko, S.H.; Xiao, Q. Neighborhood Light at Night and Noise Levels, and Long-Term Sleep Trajectories in the Southern Community Cohort Study. Clocks Sleep 2024, 6, 234–245. [Google Scholar] [CrossRef] [PubMed]
- El-Sheikh, M.; Keiley, M.; Bagley, E.J.; Chen, E. Socioeconomic Adversity and Women’s Sleep: Stress and Chaos as Mediators. Behav. Sleep Med. 2015, 13, 506–523. [Google Scholar]
- Virtanen, M.; Myllyntausta, S.; Karkkola, P.; Pentti, J.; Ropponen, A.; Vahtera, J.; Stenholm, S. Components of Stress and Their Associations with Sleep Problems: A Cohort Study of Older Employees. J. Occup. Environ. Med. 2022, 64, 390–396. [Google Scholar] [CrossRef]
- Azizi-Zeinalhajlou, A.; Mirghafourvand, M.; Nadrian, H.; Samei Sis, S.; Matlabi, H. The contribution of social isolation and loneliness to sleep disturbances among older adults: A systematic review. Sleep Biol. Rhythms 2022, 20, 153–163. [Google Scholar]
- Etindele Sosso, F.A. Measuring Sleep Health Disparities with Polysomnography: A Systematic Review of Preliminary Findings. Clocks Sleep 2022, 4, 80–87. [Google Scholar] [CrossRef]
- Dregan, A.; Armstrong, D. Cross-country variation in sleep disturbance among working and older age groups: An analysis based on the European Social Survey. Int. Psychogeriatr. 2011, 23, 1413–1420. [Google Scholar] [PubMed]
- Chen, Y.; Kartsonaki, C.; Clarke, R.; Guo, Y.; Yu, C.; Bian, Z.; Jiang, Q.; Li, S.; Chen, J.; Li, L.; et al. Characteristics and correlates of sleep duration, daytime napping, snoring and insomnia symptoms among 0.5 million Chinese men and women. Sleep Med. 2018, 44, 67–75. [Google Scholar] [CrossRef]
- McLay, L.; Jamieson, H.A.; France, K.G.; Schluter, P.J. Loneliness and social isolation is associated with sleep problems among older community dwelling women and men with complex needs. Sci. Rep. 2021, 11, 4877. [Google Scholar] [CrossRef]
- Santos-Silva, R.; Bittencourt, L.R.; Pires, M.L.; de Mello, M.T.; Taddei, J.A.; Benedito-Silva, A.A.; Pompeia, C.; Tufik, S. Increasing trends of sleep complaints in the city of Sao Paulo, Brazil. Sleep Med. 2010, 11, 520–524. [Google Scholar] [CrossRef]
- Hirotsu, C.; Tufik, S.; Andersen, M.L. Interactions between sleep, stress, and metabolism: From physiological to pathological conditions. Sleep Sci. 2015, 8, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Rocha, S.; Almeida, D.M.; Chiang, J.J.; Cole, S.W.; Irwin, M.R.; Seeman, T.; Fuligni, A.J. The Relationship Between Family Socioeconomic Status and Adolescent Sleep and Diurnal Cortisol. Psychosom. Med. 2022, 84, 848–855. [Google Scholar] [CrossRef]
- Tran, P.; Shelton, B.; Tran, L. Estimates of short sleep duration among US rural and urban women with prediabetes. PLoS ONE 2023, 18, e0284304. [Google Scholar] [PubMed]
- Cohrs, S.; Rodenbeck, A.; Riemann, D.; Szagun, B.; Jaehne, A.; Brinkmeyer, J.; Gründer, G.; Wienker, T.; Diaz-Lacava, A.; Mobascher, A.; et al. Impaired sleep quality and sleep duration in smokers-results from the German Multicenter Study on Nicotine Dependence. Addict. Biol. 2014, 19, 486–496. [Google Scholar] [PubMed]
- Dokkedal-Silva, V.; Fernandes, G.L.; Tufik, S.; Andersen, M.L. The links between commuting time and sleep quality: A trend in modern urban centers. J. Clin. Sleep Med. 2022, 18, 2875–2876. [Google Scholar] [CrossRef] [PubMed]
- Nosek, B.A.; Errington, T.M. What is replication? PLoS Biol. 2020, 18, e3000691. [Google Scholar] [CrossRef]
- Diaba-Nuhoho, P.; Amponsah-Offeh, M. Reproducibility and research integrity: The role of scientists and institutions. BMC Res. Notes 2021, 14, 451. [Google Scholar] [CrossRef]
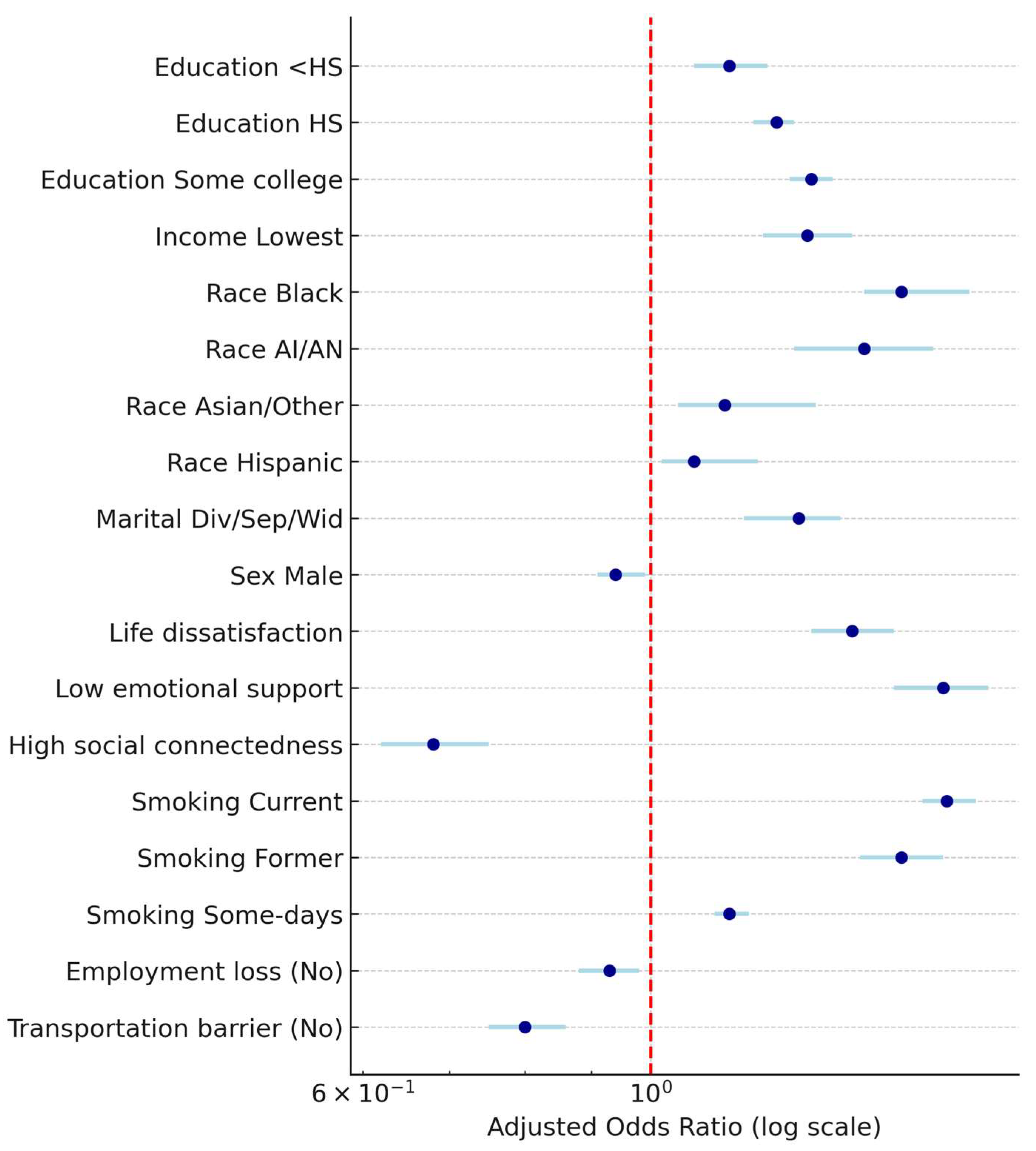
| Predictor | AOR | 95% CI | p-Value |
|---|---|---|---|
| Education (<HS vs. College) | 1.15 | 1.08–1.23 | <0.001 |
| Education (HS vs. College) | 1.25 | 1.20–1.29 | <0.001 |
| Education (Some College vs. College) | 1.33 | 1.28–1.38 | <0.001 |
| Income (Lowest vs. Highest) | 1.32 | 1.22–1.43 | <0.001 |
| Race/Ethnicity (Black vs. White) | 1.56–1.76 | 1.46–1.85 | <0.001 |
| Race/Ethnicity (AI/AN vs. White) | 1.46–1.58 | 1.29–1.65 | <0.001 |
| Race/Ethnicity (Asian/Other vs. White) | 1.14–1.25 | 1.05–1.34 | <0.01 |
| Race/Ethnicity (Hispanic vs. White) | 1.08–1.16 | 1.02–1.21 | 0.005 |
| Marital (Divorced/Separated vs. Married) | 1.21–1.39 | 1.18–1.40 | <0.001 |
| Sex (Male vs. Female) | 0.94–0.99 | 0.91–1.01 | 0.28–<0.001 |
| Life satisfaction (Dissatisfied vs. Satisfied) | 1.43 | 1.33–1.54 | <0.001 |
| Emotional support (Rarely vs. Always) | 1.68 | 1.54–1.82 | <0.001 |
| Social connectedness (High vs. Isolated) | 0.68 | 0.62–0.75 | <0.001 |
| Predictor | AOR | 95% CI | p-Value |
|---|---|---|---|
| Smoking (Current vs. Never) | 1.69 | 1.62–1.78 | <0.001 |
| Smoking (Former vs. Never) | 1.56 | 1.45–1.68 | <0.001 |
| Smoking (Some days vs. Never) | 1.15 | 1.12–1.19 | <0.001 |
| Binge drinking (Yes vs. No) | 0.97 | 0.93–1.00 | 0.068 |
| Employment loss (No vs. Yes) | 0.93 | 0.88–0.98 | 0.010 |
| Transportation barrier (No vs. Yes) | 0.80 | 0.75–0.86 | <0.001 |
| Urban vs. Rural | 0.98 | 0.94–1.03 | 0.48 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
DelRosso, L.M.; Vodapally, M. Sleep Health Inequities: Sociodemographic, Psychosocial, and Structural Determinants of Short Sleep in U.S. Adults. Clocks & Sleep 2025, 7, 59. https://doi.org/10.3390/clockssleep7040059
DelRosso LM, Vodapally M. Sleep Health Inequities: Sociodemographic, Psychosocial, and Structural Determinants of Short Sleep in U.S. Adults. Clocks & Sleep. 2025; 7(4):59. https://doi.org/10.3390/clockssleep7040059
Chicago/Turabian StyleDelRosso, Lourdes M., and Mamatha Vodapally. 2025. "Sleep Health Inequities: Sociodemographic, Psychosocial, and Structural Determinants of Short Sleep in U.S. Adults" Clocks & Sleep 7, no. 4: 59. https://doi.org/10.3390/clockssleep7040059
APA StyleDelRosso, L. M., & Vodapally, M. (2025). Sleep Health Inequities: Sociodemographic, Psychosocial, and Structural Determinants of Short Sleep in U.S. Adults. Clocks & Sleep, 7(4), 59. https://doi.org/10.3390/clockssleep7040059






