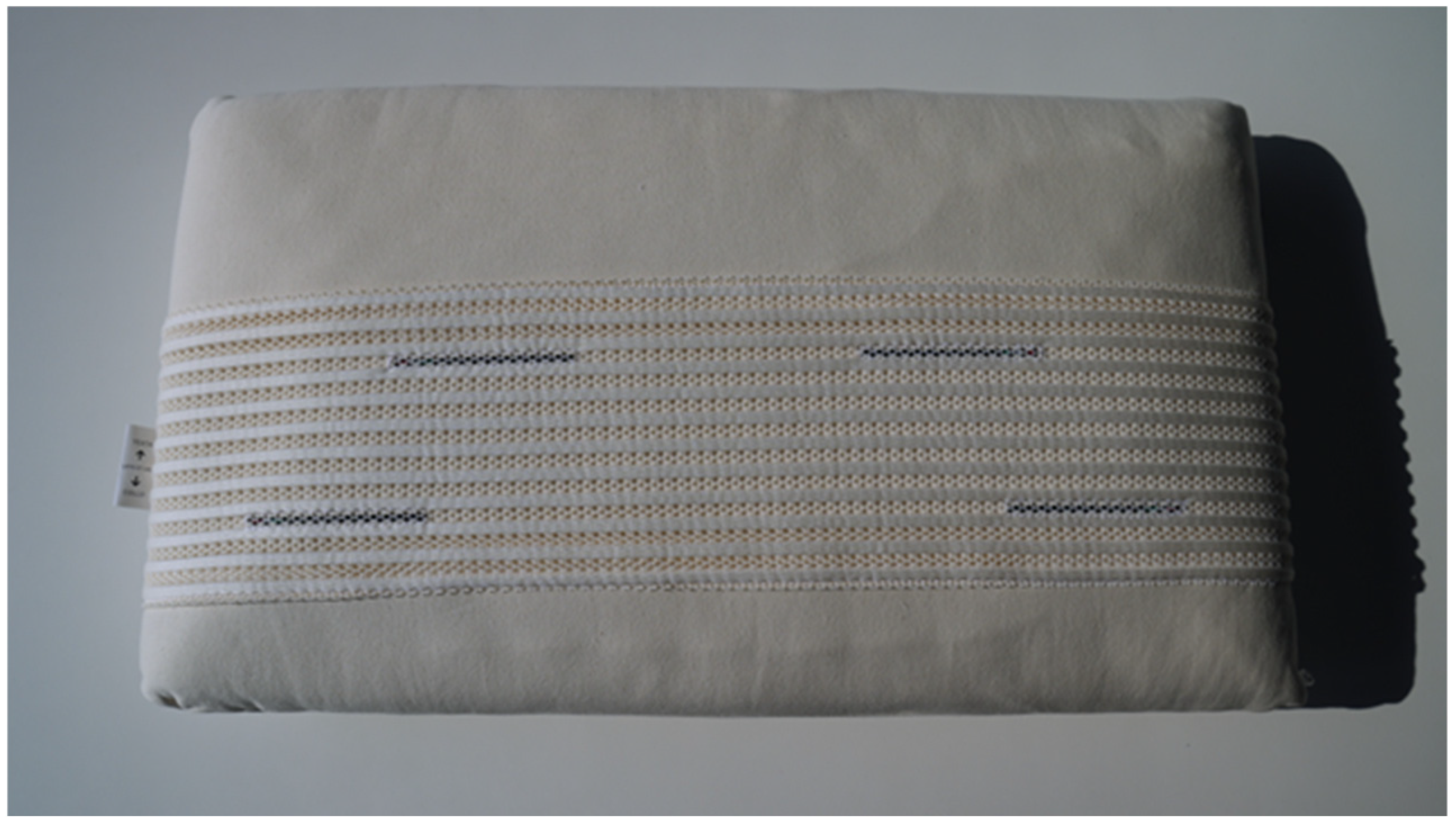
Enhancing Sleep Quality: The Impact of the “Repose Tao” Pillow with Taopatch® Nanotechnology—A Pilot Study
Abstract
1. Introduction
2. Results
3. Discussion
Limitations and Future Research
4. Materials and Methods
4.1. Participants
4.2. Procedures
Intervention
4.3. Measurements
Sleep Quality Assessment
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Helvig, A.; Wade, S.; Hunter-Eades, L. Rest and the associated benefits in restorative sleep: A concept analysis. J. Adv. Nurs. 2016, 72, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Koketsu, J.S. Sleep and rest. In Pedretti’s Occupational Therapy-E-Book; Elsevier: Amsterdam, The Netherlands, 2024; p. 320. [Google Scholar]
- Taillard, J.; Gronfier, C.; Bioulac, S.; Philip, P.; Sagaspe, P. Sleep in normal aging, homeostatic and circadian regulation and vulnerability to sleep deprivation. Brain Sci. 2021, 11, 1003. [Google Scholar] [CrossRef] [PubMed]
- Khoury, J.; Doghramji, K. Primary sleep disorders. Psychiatr. Clin. 2015, 38, 683–704. [Google Scholar] [CrossRef] [PubMed]
- Ting, L.; Malhotra, A. Disorders of sleep: An overview. Prim. Care 2005, 32, 305–319. [Google Scholar] [CrossRef]
- Ohayon, M.M. Epidemiological overview of sleep disorders in the general population. Sleep Med. Res. 2011, 2, 1–9. [Google Scholar] [CrossRef]
- Almeneessier, A.S.; Gupta, R.; Pandi-Perumal, S.R.; BaHammam, A.S. Overview of sleep disorders. In The Behavioral, Molecular, Pharmacological, and Clinical Basis of the Sleep-Wake Cycle; Academic Press: New York, NY, USA, 2019; pp. 103–122. [Google Scholar]
- Lanzafame, R.J. Editorial: Good vibrations: More evidence of reciprocity? Photomed. Laser Surg. 2007, 25, 465–466. [Google Scholar] [CrossRef]
- Kuehn, B.M. Resetting the circadian clock might boost metabolic health. JAMA 2017, 317, 1303–1305. [Google Scholar] [CrossRef]
- Kramer, A.; Merrow, M. Circadian Clocks; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Foster, R.G.; Kreitzman, L. The rhythms of life: What your body clock means to you! Exp. Physiol. 2014, 99, 599–606. [Google Scholar] [CrossRef]
- Valverde, A.; Hamilton, C.; Moro, C.; Billeres, M.; Magistretti, P.; Mitrofanis, J. Lights at night: Does photobiomodulation improve sleep? Neural Regen. Res. 2023, 18, 474–477. [Google Scholar]
- Santana-Blank, L.; Rodríguez-Santana, E. Photobiomodulation in Light of Our Biological Clock’s Inner Workings. Photomed. Laser Surg. 2018, 36, 119–121. [Google Scholar] [CrossRef]
- Jung, J.; Kim, T. Photobiomodulation and Its Therapeutic Potential in Sleep Disturbances. Sleep Med. Res. 2024, 15, 218–227. [Google Scholar] [CrossRef]
- Bagnato, V.S.; Rodrigues, T.Z.; Garcia, V.; Vidotti, H.G.M.; Aquino Junior, A.E.D. Systemic effects of photobiomodulation and ultrasound as a potentiating tool in the treatment of sleep disorders: Pilot study. J. Nov. Physiother. 2024, 14, 1000703-1. [Google Scholar]
- Revell, V.L.; Skene, D.J. Light-induced melatonin suppression in humans with polychromatic and monochromatic light. Chronobiol. Int. 2007, 24, 1125–1137. [Google Scholar] [CrossRef]
- Zaidi, F.H.; Hull, J.T.; Peirson, S.N.; Wulff, K.; Aeschbach, D.; Gooley, J.J.; Brainard, G.C.; Gregory-Evans, K.; Rizzo, J.F.; Czeisler, C.A.; et al. Short-wavelength light sensitivity of circadian, pupillary, and visual awareness in humans lacking an outer retina. Curr. Biol. 2007, 17, 2122–2128. [Google Scholar] [CrossRef]
- Khalsa, S.B.S.; Jewett, M.E.; Cajochen, C.; Czeisler, C.A. A phase response curve to single bright light pulses in human subjects. J. Physiol. 2003, 549, 945–952. [Google Scholar] [CrossRef]
- Zeitzer, J.M.; Khalsa, S.B.; Boivin, D.B.; Duffy, J.F.; Shanahan, T.L.; Kronauer, R.E.; Czeisler, C.A. Temporal dynamics of late-night photic stimulation of the human circadian timing system. Am. J. Physiol. 2005, 289, R839–R844. [Google Scholar] [CrossRef]
- Rani, S.; Singh, S.; Kumar, V. Light sensitivity of the biological clock. In Biological Rhythms; Springer: Berlin/Heidelberg, Germany, 2002; pp. 232–243. [Google Scholar]
- Glass, G.E. Photobiomodulation: The clinical applications of low-level light therapy. Aesthet. Surg. J. 2021, 41, 723–738. [Google Scholar] [CrossRef]
- Giménez, M.C.; Luxwolda, M.; Van Stipriaan, E.G.; Bollen, P.P.; Hoekman, R.L.; Koopmans, M.A.; Gordijn, M.C. Effects of near-infrared light on well-being and health in human subjects with mild sleep-related complaints: A double-blind, randomized, placebo-controlled study. Biology 2022, 12, 60. [Google Scholar] [CrossRef]
- Baig, N.; Kammakakam, I.; Falath, W. Nanomaterials: A review of synthesis methods, properties, recent progress, and challenges. Mater. Adv. 2021, 2, 1821–1871. [Google Scholar] [CrossRef]
- Moro, C.; Valverde, A.; Dole, M.; Hoh Kam, J.; Hamilton, C.; Liebert, A.; Mitrofanis, J. The effect of photobiomodulation on the brain during wakefulness and sleep. Front. Neurosci. 2022, 16, 1–15. [Google Scholar] [CrossRef]
- Elder, G.J.; Flo-Groeneboom, E. How can light be used to optimize sleep and health in older adults? Prog. Brain Res. 2022, 273, 331–355. [Google Scholar] [PubMed]
- Campoli, F.; Iovane, A.; Fabris, A.; Francavilla, V.; Proia, P.; Caprioli, L.; Bonaiuto, V.; Annino, G.; Padua, E.; Messina, G. Acute Effects of Nanotechnological Devices for the Muscle and Joint Pain Treatment. In International Workshop on Engineering Methodologies for Medicine and Sport; Springer: Cham, Switzerland, 2024; pp. 86–96. [Google Scholar]
- Ottaviani, M.M.; Macefield, V.G. Structure and functions of the vagus nerve in mammals. Compr. Physiol. 2022, 12, 3989–4037. [Google Scholar] [CrossRef] [PubMed]
- Terman, M.; Terman, J.S. Light therapy. Princ. Pract. Sleep Med. 2005, 4, 1424–1442. [Google Scholar]
- Golden, R.N.; Gaynes, B.N.; Ekstrom, R.D.; Hamer, R.M.; Jacobsen, F.M.; Suppes, T.; Nemeroff, C.B. The efficacy of light therapy in the treatment of mood disorders: A review and meta-analysis of the evidence. Am. J. Psychiatry 2005, 162, 656–662. [Google Scholar] [CrossRef]
- Gupta, R.; Behera, C.; Paudwal, G.; Rawat, N.; Baldi, A.; Gupta, P.N. Recent advances in formulation strategies for efficient delivery of vitamin D. AAPS Pharmscitech 2019, 20, 11. [Google Scholar] [CrossRef]
- Gudin, J.A.; Dietze, D.T.; Hurwitz, P.L. Using Nanotechnology to Improve Pain and Function with a Novel, Drug-Free, Topical Pain-Relief Patch: An Interim Analysis. Anesth Pain Res. 2020, 4, 1–10. [Google Scholar] [CrossRef]
- Karadjova, M.; Dimitrova, T.; Dobreva, D.; Petrova, J.; Messina, G. Improvement of gait, balance and coordination after application of Taopatch® device. Eur. J. Transl. Myol. 2023, 33, 75–87. [Google Scholar]
- Corna, S.; Aspesi, V.; Clerici, D.; Parisio, C.; Seitanidis, J.; Cau, N.; Capodaglio, P. Effects of nanotechnology-based devices on postural control in healthy subjects. J. Sports Med. Phys. Fit. 2017, 58, 1418–1422. [Google Scholar]
- Messina, G.; Amato, A.; Alioto, A.; Stallone, R.; Rizzo, F.; Ragonese, P.; Proia, P. A new road to improve vitamin D and balance through Taopatch® and proprioceptive protocol in Multiple Sclerosis patients. Eur. J. Transl. Myol. 2022, 32, 10774. [Google Scholar] [CrossRef]
- Krsek, A.; Baticic, L. Nanotechnology-driven therapeutic innovations in neurodegenerative disorders: A focus on Alzheimer’s and Parkinson’s disease. Future Pharmacol. 2024, 4, 352–379. [Google Scholar] [CrossRef]
- Lok, R.; Qian, J.; Chellappa, S.L. Sex differences in sleep, circadian rhythms, and metabolism: Implications for precision medicine. Sleep Med. Rev. 2024, 75, 101926–101939. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Wing, Y.K. Sex differences in insomnia: A meta-analysis. Sleep 2006, 29, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Baker, F.C.; Yűksel, D.; de Zambotti, M. Sex Differences in Sleep. In Sleep Disorders in Women: A Guide to Practical Management; Attarian, H., Viola-Saltzman, M., Eds.; Humana: Cham, Switzerland, 2020. [Google Scholar]
- Fatima, Y.; Doi, S.A.; Najman, J.M.; Al Mamun, A. Exploring gender difference in sleep quality of young adults: Findings from a large population study. Clin. Med. Res. 2016, 14, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Meers, J.; Stout-Aguilar, J.; Nowakowski, S. Chapter 3—Sex differences in sleep health. In Sleep and Health; Grandner, M.A., Ed.; Academic Press: New York, NY, USA, 2019; pp. 21–29. [Google Scholar]
- Baker, F.C.; Driver, H.S. Circadian rhythms, sleep, and the menstrual cycle. Sleep Med. 2007, 8, 613–622. [Google Scholar] [CrossRef]
- Owen, J.A. Physiology of the menstrual cycle. Am. J. Clin. Nutr. 1975, 28, 333–338. [Google Scholar] [CrossRef]
- Boukari, R.; Laouafa, S.; Ribon-Demars, A.; Bairam, A.; Joseph, V. Ovarian steroids act as respiratory stimulant and antioxidant against the causes and consequences of sleep-apnoea in women. Respir. Physiol. Neurobiol. 2017, 239, 46–54. [Google Scholar] [CrossRef]
- Caufriez, A.; Leproult, R.; L’Hermite-Baleriaux, M.; Kerkhofs, M.; Copinschi, G. Progesterone prevents sleep disturbances and modulates GH, TSH, and melatonin secretion in postmenopausal women. J. Clin. Endocrinol. Metab. 2011, 96, E614–E623. [Google Scholar] [CrossRef]
- Gomez-Santos, C.; Saura, C.B.; Lucas, J.A.; Castell, P.; Madrid, J.A.; Garaulet, M. Menopause status is associated with circadian- and sleep-related alterations. Menopause 2016, 23, 682–690. [Google Scholar] [CrossRef]
- Cole, J.C.; Dubois, D.; Kosinski, M. Use of patient-reported sleep measures in clinical trials of pain treatment: A literature review and synthesis of current sleep measures and a conceptual model of sleep disturbance in pain. Clin. Therap. 2007, 29, 2580–2588. [Google Scholar] [CrossRef]
- Katz, J.N.; Chang, L.C.; Sangha, O.; Fossel, A.H.; Bates, D.W. The association of self-reported back pain with sleep disturbance and fatigue: A cross-sectional study of primary care patients. Arch. Intern. Med. 2011, 156, 545–549. [Google Scholar]
- Liebert, A.; Capon, W.; Pang, V.; Vila, D.; Bicknell, B.; McLachlan, C.; Kiat, H. Photophysical mechanisms of photobiomodulation therapy as precision medicine. Biomedicines 2023, 11, 237. [Google Scholar] [CrossRef]
- Wang, X.; Liu, Y.; Zhang, H.; Zhou, Y. Advances in nanotechnology-based sleep aids: Current evidence and future perspectives. J. Sleep Res. 2022, 31, e13562. [Google Scholar] [CrossRef] [PubMed]
- Cole, J.C.; Motivala, S.J.; Buysse, D.J.; Oxman, M.N.; Levin, M.J.; Irwin, M.R. Validation of a 3-factor scoring model for the Pittsburgh Sleep Quality Index in older adults. Sleep 2006, 29, 112–116. [Google Scholar] [CrossRef] [PubMed]
- Cole, C.; Richards, K.C.; Zaslavsky, O. Sleep hygiene and sleep quality in older adults. J. Gerontol. Nurs. 2006, 32, 12–20. [Google Scholar]
- Duffy, J.F.; Wright, K.P. Entrainment of the human circadian system by light. J. Biol. Rhythm. 2005, 20, 326–338. [Google Scholar] [CrossRef]
- Lechat, B.; Scott, H.; Naik, G.; Hansen, K.; Nguyen, D.P.; Vakulin, A.; Eckert, D.J. New and emerging approaches to better define sleep disruption and its consequences. Front. Neurol. 2021, 15, 751730. [Google Scholar] [CrossRef]
- Parrino, L.; Halasz, P.; Szucs, A.; Thomas, R.J.; Azzi, N.; Rausa, F.; Mutti, C. Sleep medicine: Practice, challenges and new frontiers. Front. Neurol. 2022, 13, 966659. [Google Scholar] [CrossRef]
- Malik, S.; Muhammad, K.; Waheed, Y. Emerging Applications of Nanotechnology in Healthcare and Medicine. Molecules 2023, 28, 6624. [Google Scholar] [CrossRef]
- Egwu, C.O.; Aloke, C.; Onwe, K.T.; Umoke, C.I.; Nwafor, J.; Eyo, R.A.; Chukwu, J.A.; Ufebe, G.O.; Ladokun, J.; Audu, D.T. Nanomaterials in Drug Delivery: Strengths and Opportunities in Medicine. Molecules 2024, 29, 2584. [Google Scholar] [CrossRef]
- Buysee, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. Pittsburgh Sleep Quality Index (PSQI); APA PsycTests: Washington, DC, USA, 1989. [Google Scholar]
- Olejnik, S.; Algina, J. Generalized Eta and Omega Squared Statistics: Measures of Effect Size for Some Common Research Designs. Psychol. Methods 2003, 8, 434–447. [Google Scholar] [CrossRef]

| Age (Years) | Height (m) | Weight (kg) | |
|---|---|---|---|
| EG | 44.3 ± 3.1 | 1.70 ± 4.85 | 77.7 ± 7.19 |
| CG | 43.4 ± 3.2 | 1.69 ± 4.36 | 69.4 ± 6.77 |
| Sleep Dimensions | T0 | T1 | T2 | F | η2 | |
|---|---|---|---|---|---|---|
| Subjective Sleep Quality | EG | 1.2 ± 0.7 | 0.8 ± 0.6 | 0.4 ± 0.6 ** | 21.35 | 0.20 |
| CG | 1.4 ± 0.8 | 0.8 ± 1.1 | 0.8 ± 1.1 * | |||
| Sleep Latency | EG | 1.1 ± 0.9 | 0.7 ± 0.8 | 0.5 ± 0.5 * | 39.06 | 0.32 |
| CG | 1.6 ± 0.5 | 0.7 ± 0.8 | 0.1 ± 0.3 ** | |||
| Sleep Duration | EG | 1.3 ± 1.1 | 0.9 ± 0.7 | 0.9 ± 0.6 * | 15.31 | 0.15 |
| CG | 2 ± 0.8 | 1.5 ± 1.1 | 1.2 ± 0.9 | |||
| Sleep Disturbance | EG | 1.4 ± 0.5 | 1 ± 0.3 | 0.7 ± 0.5 * | 11.14 | 0.12 |
| CG | 1.4 ± 0.7 | 1 ± 0.8 | 1.2 ± 0.6 | |||
| Daytime Disfunction | EG | 0.7 ± 0.5 | 0.4 ± 0.5 | 0.4 ± 0.6 * | 19.11 | 0.17 |
| CG | 1.4 ± 0.7 | 1 ± 0.5 | 2 ± 0 * | |||
| TOT | EG | 6.5 ± 3.9 | 5.8 ± 2.2 | 3.2 ± 1.9 ** | 42.35 | 0.39 |
| CG | 8.7 ± 2.7 | 6.2 ± 3 | 6 ± 1.7 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campoli, F.; Orofino, F.; Messina, G.; Corrado, D.D.; Francavilla, V.C. Enhancing Sleep Quality: The Impact of the “Repose Tao” Pillow with Taopatch® Nanotechnology—A Pilot Study. Clocks & Sleep 2025, 7, 32. https://doi.org/10.3390/clockssleep7030032
Campoli F, Orofino F, Messina G, Corrado DD, Francavilla VC. Enhancing Sleep Quality: The Impact of the “Repose Tao” Pillow with Taopatch® Nanotechnology—A Pilot Study. Clocks & Sleep. 2025; 7(3):32. https://doi.org/10.3390/clockssleep7030032
Chicago/Turabian StyleCampoli, Francesca, Francesca Orofino, Giuseppe Messina, Donatella Di Corrado, and Vincenzo Cristian Francavilla. 2025. "Enhancing Sleep Quality: The Impact of the “Repose Tao” Pillow with Taopatch® Nanotechnology—A Pilot Study" Clocks & Sleep 7, no. 3: 32. https://doi.org/10.3390/clockssleep7030032
APA StyleCampoli, F., Orofino, F., Messina, G., Corrado, D. D., & Francavilla, V. C. (2025). Enhancing Sleep Quality: The Impact of the “Repose Tao” Pillow with Taopatch® Nanotechnology—A Pilot Study. Clocks & Sleep, 7(3), 32. https://doi.org/10.3390/clockssleep7030032








