Associations between Sleep Hygiene and Mental Complaints in a French Healthcare Worker Population during the COVID-19 Crisis: A Cross-Sectional Analysis to Personalize Sleep Health Interventions
Abstract
1. Introduction
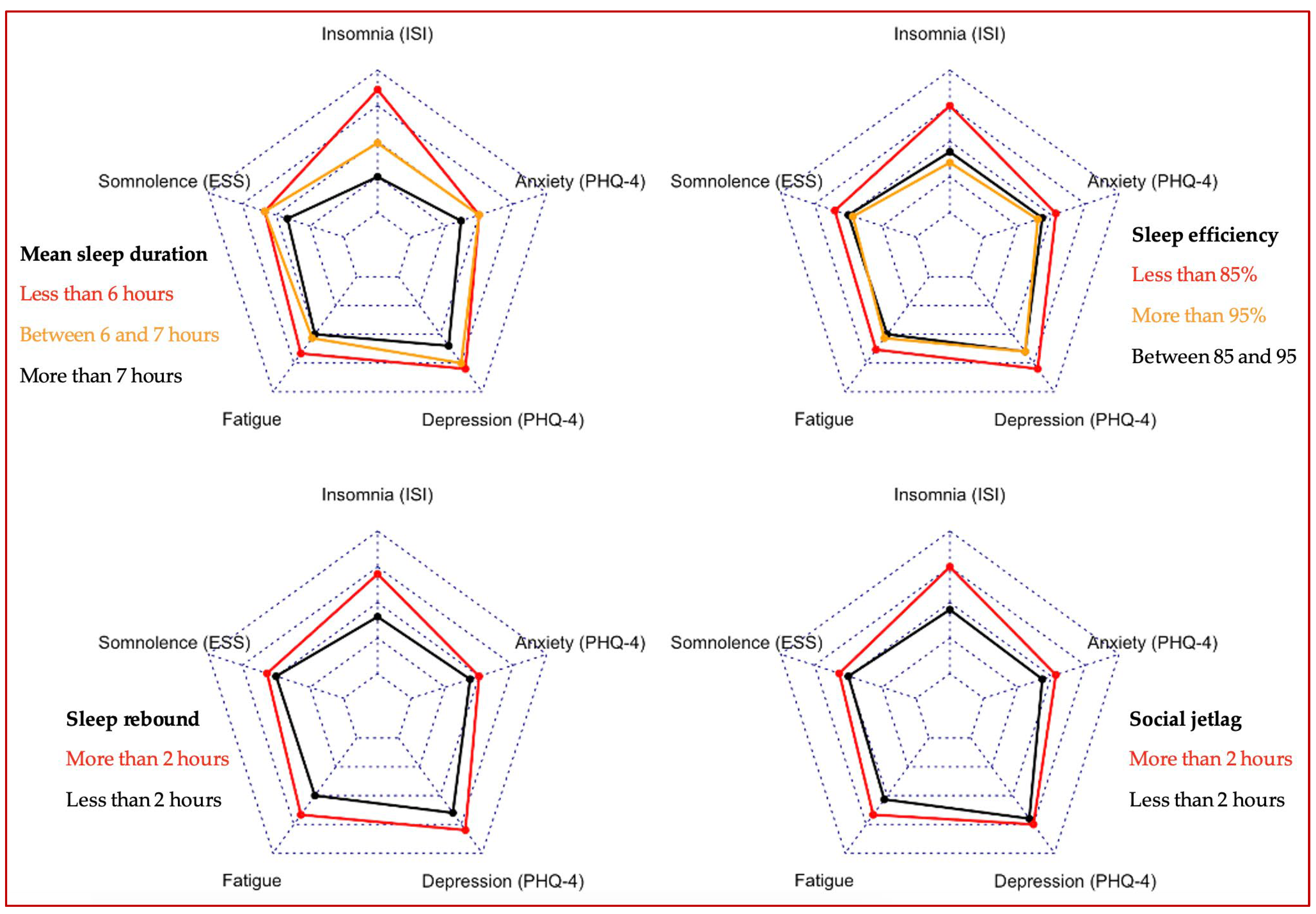
2. Results
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Garbarino, S.; Lanteri, P.; Durando, P.; Magnavita, N.; Sannita, W.G. Co-Morbidity, Mortality, Quality of Life and the Healthcare/Welfare/Social Costs of Disordered Sleep: A Rapid Review. Int. J. Environ. Res. Public Health 2016, 13, 831. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J. Sleep health: Can we define it? Does it matter? Sleep 2014, 37, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Beck, F.; Léon, C.; Pin-Le Corre, S.; Léger, D. Sleep disorders: Sociodemographics and psychiatric comorbidities in a sample of 14,734 adults in France (Baromètre santé INPES). Rev. Neurol. 2009, 165, 933–942. [Google Scholar] [CrossRef] [PubMed]
- Léger, D.; Guilleminault, C.; Bader, G.; Lévy, E.; Paillard, M. Medical and socio-professional impact of insomnia. Sleep 2002, 25, 621–625. [Google Scholar] [CrossRef]
- Wu, K.; Wei, X. Analysis of Psychological and Sleep Status and Exercise Rehabilitation of Front-Line Clinical Staff in the Fight Against COVID-19 in China. Med. Sci. Monit. Basic Res. 2020, 26, e924085. [Google Scholar] [CrossRef] [PubMed]
- Irish, L.A.; Kline, C.E.; Gunn, H.E.; Buysse, D.J.; Hall, M.H. The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Med. Rev. 2015, 22, 23–36. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Marvaldi, M.; Mallet, J.; Dubertret, C.; Moro, M.R.; Guessoum, S.B. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2021, 126, 252–264. [Google Scholar] [CrossRef] [PubMed]
- Vallée, M.; Kutchukian, S.; Pradere, B.; Verdier, E.; Durbant, È.; Ramlugun, D.; Weizman, I.; Kassir, R.; Cayeux, A.; Pécheux, O.; et al. Prospective and observational study of COVID-19’s impact on mental health and training of young surgeons in France. Br. J. Surg. 2020, 107, e486–e488. [Google Scholar] [CrossRef]
- Qiu, D.; Yu, Y.; Li, R.Q.; Li, Y.L.; Xiao, S.Y. Prevalence of sleep disturbances in Chinese healthcare professionals: A systematic review and meta-analysis. Sleep Med. 2020, 67, 258–266. [Google Scholar] [CrossRef]
- Richter, E.; Blasco, V.; Antonini, F.; Rey, M.; Reydellet, L.; Harti, K.; Nafati, C.; Albanèse, J.; Leone, M.; AzuRea Network. Sleep disorders among French anaesthesiologists and intensivists working in public hospitals: A self-reported electronic survey. Eur. J. Anaesthesiol. 2015, 32, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Bezner, T.L.; Sivaraman, M. COVID-19 Pandemic and Its Impact on Sleep Health: A Rapid Review. Mo Med 2022, 119, 385–389. [Google Scholar] [PubMed]
- Roenneberg, T.; Wirz-Justice, A.; Merrow, M. Life between clocks: Daily temporal patterns of human chronotypes. J. Biol. Rhythms. 2003, 18, 80–90. [Google Scholar] [CrossRef] [PubMed]
- Roenneberg, T.; Pilz, L.K.; Zerbini, G.; Winnebeck, E.C. Chronotype and social jetlag: A (self-) critical review. Biology 2019, 8, E54. [Google Scholar] [CrossRef]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Adams Hillard, P.J.; Katz, E.S.; et al. National Sleep Foundation’s updated sleep duration recommendations: Final report. Sleep Health 2015, 1, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Beauvalet, J.C.; Quiles, C.L.; de Oliveira, M.A.B.; Ilgenfritz, C.A.V.; Hidalgo, M.P.L.; Tonon, A.C. Social jetlag in health and behavioral research: A systematic review. ChronoPhysiology Ther. 2017, 7, 19–31. [Google Scholar] [CrossRef]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Cerri, L.Q.; Justo, M.C.; Clemente, V.; Gomes, A.A.; Pereira, A.S.; Marques, D.R. Insomnia Severity Index: A reliability generalisation meta-analysis. J. Sleep Res. 2023, 32, e13835. [Google Scholar] [CrossRef]
- Kaminska, M.; Jobin, V.; Mayer, P.; Amyot, R.; Perraton-Brillon, M.; Bellemare, F. The Epworth Sleepiness Scale: Self-administration versus administration by the physician, and validation of a French version. Can. Respir. J. 2010, 17, e27–e34. [Google Scholar] [CrossRef]
- Gonçalves, M.T.; Malafaia, S.; Moutinho Dos Santos, J.; Roth, T.; Marques, D.R. Epworth sleepiness scale: A meta-analytic study on the internal consistency. Sleep Med. 2023, 109, 261–269. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. Maslach Burnout Inventory Manual, 3rd ed.; Consulting Psychologists Press: Menlo Park, CA, USA, 1996. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W.; Löwe, B. An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics 2009, 50, 613–621. [Google Scholar] [PubMed]
| Variables | n (%) | Mean ± SD {Min–Max} |
Age
| 1562 (100%) 358 (22.9%) 681 (43.6%) 494 (31.6%) 29 (1.9%) | 40.0 ± 11.2 {18–75} |
Gender
| 1562 (100%) 1258 (80.5%) 304 (19.5%) | |
IMC
| 1562 (100%) 36 (2.3%) 968 (62.0%) 377 (24.1%) 159 (10.2%) 22 (1.4%) | 24.5 ± 6.0 {8–100} |
Literacy
| 1562 (100%) 138 (8.8%) 1096 (70.2%) 328 (21.0%) | |
Living environment
| 1562 (100%) 425 (27.2%) 1137 (72.8%) | |
Work schedules
| 1562 (100%) 840 (53.8%) 514 (32.9%) 208 (13.3%) | |
Work in COVID-19 unit
| 1562 (100%) 265 (17.0%) 1297 (83.0%) | |
Mean sleep duration (hours)
| 1562 (100%) 405 (25.9%) 484 (31.0%) 673 (43.1%) | 6 h45 ± 54′ {5 h–9 h30} |
Time-in-bed (hours)
| 1562 (100%) 93 (6.0%) 280 (17.9%) 1189 (76.1%) | 7 h37 ± 54′ {5 h–14 h} |
Sleep efficiency (%)
| 1562 (100%) 379 (24.3%) 756 (48.4%) 427 (27.3%) | 89% ± 10% {48%–100%} |
Time-awake-in-bed
| 1562 (100%) 487 (33.9%) 460 (32.0%) 491 (34.1%) | 52′ ± 46′ {0–8 h} |
Sleep rebound
| 1562 (100%) 427 (27.3%) 1135 (72.7%) | 1 h36 ± 1 h26 {−6 h30–10 h} |
Social jetlag
| 1562 (100%) 179 (11.5%) 1383 (88.5%) | 23′ ± 2 h38 {−11 h30–5 h30} |
Insomnia (ISI)
| 1562 (100%) 530 (33.9%) 1032 (66.1%) | 11.9 ± 5.6 {0–28} |
Excessive daytime sleepiness (ESS)
| 1562 (100%) 704 (45.1%) 858 (54.9%) | 10.1 ± 4.7 {0–24} |
Sleep apnea (NOSAS)
| 1562 (100%) 142 (9.1%) 1420 (90.9%) | |
Fatigue
| 1562 (100%) 205 (13.1%) 1357 (86.9%) | |
Burnout
| 1562 (100%) 217 (13.9%) 1345 (86.1%) | |
Anxiety (PHQ-4)
| 1562 (100%) 557 (35.7%) 1005 (64.3%) | 2.4 ± 1.8 {0–6} |
Depression (PHQ-4)
| 1562 (100%) 257 (16.5%) 1305 (83.6%) | 1.4 ± 1.4 {0–6} |
| Variable | Insomnia p OR [CI] | EDS p OR [CI] | Fatigue p OR [CI] | Depression p OR [CI] | Anxiety p OR [CI] |
Mean sleep duration (hours)
| p < 0.001 Ref 1.7 [1.3–2.2] 3.8 [2.8–5.0] | p = 0.031 Ref 1.1 [0.9–1.5] 1.4 [1.1–1.8] | p = 0.646 Ref 1.2 [0.8–1.7] 1.1 [0.8–1.7] | p < 0.001 Ref 1.9 [1.3–2.6] 1.7 [1.1–2.4] | p < 0.001 Ref 2.0 [1.5–2.5] 2.0 [1.5–2.6] |
Sleep efficiency (%)
| p < 0.001 Ref 1.9 [1.5–2.5] 0.8 [0.6–1.1] | p = 0.026 Ref 1.4 [1.1–1.8] 1.0 [0.8–1.3] | p = 0.003 Ref 1.9 [1.3–2.7] 1.4 [0.9–2.0] | p = 0.022 Ref 1.5 [1.1–2.1] 0.9 [0.6–1.3] | p = 0.004 Ref 1.5 [1.2–2.0] 1.0 [0.8–1.3] |
Sleep rebound
| p = 0.001 Ref 1.5 [1.2–2.0] | p = 0.907 Ref 1.0 [0.8–1.3] | p = 0.026 Ref 1.5 [1.1–2.1] | p = 0.557 Ref 1.1 [0.8–1.5] | p = 0.074 Ref 1.3 [1.0–1.6] |
Social jetlag
| p < 0.001 Ref 1.9 [1.3–2.7] | p = 0.254 Ref 0.8 [0.6–1.2] | p = 0.249 Ref 1.4 [0.8–2.2] | p = 0.726 Ref 0.9 [0.6–1.5] | p = 0.079 Ref 1.4 [1.0–2.0] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coelho, J.; Micoulaud-Franchi, J.-A.; Philip, P. Associations between Sleep Hygiene and Mental Complaints in a French Healthcare Worker Population during the COVID-19 Crisis: A Cross-Sectional Analysis to Personalize Sleep Health Interventions. Clocks & Sleep 2024, 6, 246-254. https://doi.org/10.3390/clockssleep6020017
Coelho J, Micoulaud-Franchi J-A, Philip P. Associations between Sleep Hygiene and Mental Complaints in a French Healthcare Worker Population during the COVID-19 Crisis: A Cross-Sectional Analysis to Personalize Sleep Health Interventions. Clocks & Sleep. 2024; 6(2):246-254. https://doi.org/10.3390/clockssleep6020017
Chicago/Turabian StyleCoelho, Julien, Jean-Arthur Micoulaud-Franchi, and Pierre Philip. 2024. "Associations between Sleep Hygiene and Mental Complaints in a French Healthcare Worker Population during the COVID-19 Crisis: A Cross-Sectional Analysis to Personalize Sleep Health Interventions" Clocks & Sleep 6, no. 2: 246-254. https://doi.org/10.3390/clockssleep6020017
APA StyleCoelho, J., Micoulaud-Franchi, J.-A., & Philip, P. (2024). Associations between Sleep Hygiene and Mental Complaints in a French Healthcare Worker Population during the COVID-19 Crisis: A Cross-Sectional Analysis to Personalize Sleep Health Interventions. Clocks & Sleep, 6(2), 246-254. https://doi.org/10.3390/clockssleep6020017








