Measuring Sleep Health Disparities with Polysomnography: A Systematic Review of Preliminary Findings
Abstract
1. Introduction
2. Results
2.1. Characteristics of Studies
2.2. Polysomnography, Socioeconomic Indicators and Sleep Health
2.3. Interactions and Moderators of Polysomnography Recording
3. Discussion
3.1. Summary of Findings
3.2. Relation with Current Knowledge
3.3. Improvements for Clinical Practice
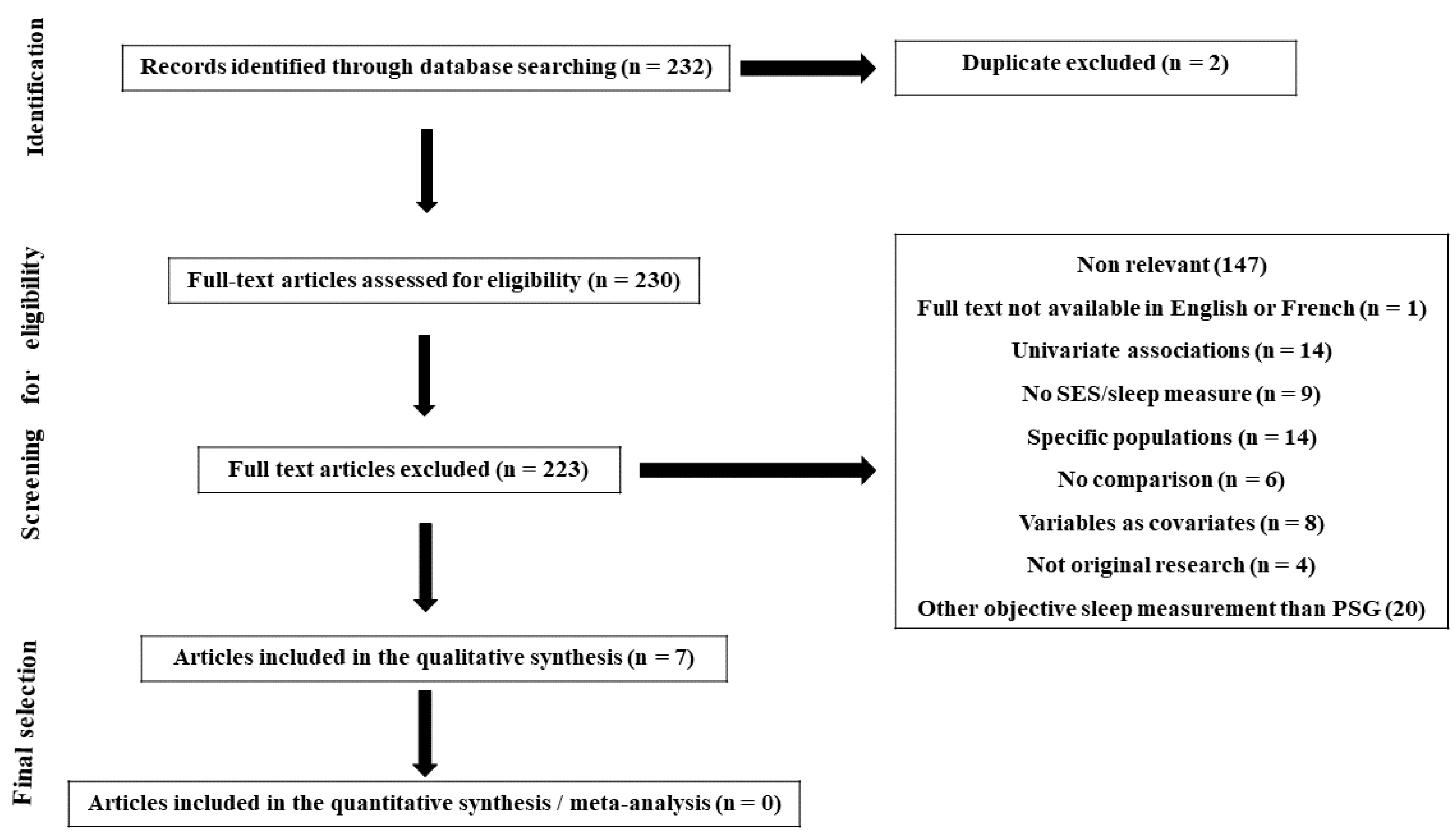
4. Materials and Methods
4.1. Literature Search
4.2. Inclusion and Exclusion Criteria
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Everly, G.S.; Lating, J.M. Sleep and Stress. In A Clinical Guide to the Treatment of the Human Stress Response; Springer: New York, NY, USA, 2019; pp. 497–522. [Google Scholar] [CrossRef]
- Achermann, P.; Borbély, A.A. Chapter 36—Sleep Homeostasis and Models of Sleep Regulation. In Principles and Practice of Sleep Medicine, 6th ed.; Kryger, M., Roth, T., Dement, W.C., Eds.; Elsevier: Amsterdam, The Netherlands, 2017; pp. 377–387.e6. [Google Scholar] [CrossRef]
- Anders, M.P.; Breckenkamp, J.; Blettner, M.; Schlehofer, B.; Berg-Beckhoff, G. Association between socioeconomic factors and sleep quality in an urban population-based sample in Germany. Eur. J. Public Health 2014, 24, 968–973. [Google Scholar] [CrossRef] [PubMed]
- Fang, S.C.; Subramanian, S.V.; Piccolo, R.; Yang, M.; Yaggi, H.K.; Bliwise, D.L.; Araujo, A.B. Geographic variations in sleep duration: A multilevel analysis from the Boston Area Community Health (BACH) Survey. J. Epidemiol. Community Health 2015, 69, 63–69. [Google Scholar] [CrossRef]
- Gosling, J.A.; Batterham, P.J.; Glozier, N.; Christensen, H. The influence of job stress, social support and health status on intermittent and chronic sleep disturbance: An 8-year longitudinal analysis. Sleep Med. 2014, 15, 979–985. [Google Scholar] [CrossRef] [PubMed]
- Haba-Rubio, J.; Marti-Soler, H.; Tobback, N.; Andries, D.; Marques-Vidal, P.; Waeber, G.; Vollenweider, P.; von Gunten, A.; Preisig, M.; Castelao, E.; et al. Sleep characteristics and cognitive impairment in the general population: The HypnoLaus study. Neurology 2017, 88, 463–469. [Google Scholar] [CrossRef]
- Etindele Sosso, F.A.; Holmes, S.D.; Weinstein, A.A. Influence of socioeconomic status on objective sleep measurement: A systematic review and meta-analysis of actigraphy studies. Sleep Health 2021, 7, 417–428. [Google Scholar] [CrossRef]
- Stringhini, S.; Haba-Rubio, J.; Marques-Vidal, P.; Waeber, G.; Preisig, M.; Guessous, I.; Bovet, P.; Vollenweider, P.; Tafti, M.; Heinzer, R. Association of socioeconomic status with sleep disturbances in the Swiss population-based CoLaus study. Sleep Med. 2015, 16, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Hirshkowitz, M. Polysomnography Challenges. Sleep Med. Clin. 2016, 11, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Lauderdale, D.S.; Knutson, K.L.; Yan, L.L.; Rathouz, P.J.; Hulley, S.B.; Sidney, S.; Liu, K. Objectively measured sleep characteristics among early-middle-aged adults: The CARDIA study. Am. J. Epidemiol. 2006, 164, 5–16. [Google Scholar] [CrossRef]
- Mezick, E.J.; Matthews, K.A.; Hall, M.; Strollo, P.J., Jr.; Buysse, D.J.; Kamarck, T.W.; Owens, J.F.; Reis, S.E. Influence of race and socioeconomic status on sleep: Pittsburgh SleepSCORE project. Psychosom. Med. 2008, 70, 410–416. [Google Scholar] [CrossRef]
- Hall, M.H.; Matthews, K.A.; Kravitz, H.M.; Gold, E.B.; Buysse, D.J.; Bromberger, J.T.; Owens, J.F.; Sowers, M. Race and financial strain are independent correlates of sleep in midlife women: The SWAN sleep study. Sleep 2009, 32, 73–82. [Google Scholar]
- Reddy, E.V.; Kadhiravan, T.; Mishra, H.K.; Sreenivas, V.; Handa, K.K.; Sinha, S.; Sharma, S.K. Prevalence and risk factors of obstructive sleep apnea among middle-aged urban Indians: A community-based study. Sleep Med. 2009, 10, 913–918. [Google Scholar] [CrossRef]
- Tomfohr, L.M.; Ancoli-Israel, S.; Dimsdale, J.E. Childhood socioeconomic status and race are associated with adult sleep. Behav. Sleep Med. 2010, 8, 219–230. [Google Scholar] [CrossRef][Green Version]
- Tufik, S.; Santos-Silva, R.; Taddei, J.A.; Bittencourt, L.R. Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med. 2010, 11, 441–446. [Google Scholar] [CrossRef]
- Petrovic, D.; Haba-Rubio, J.; Carmeli, C.; Vollenweider, P.; Heinzer, R.; Stringhini, S. Social inequalities in sleep-disordered breathing: Evidence from the CoLaus|HypnoLaus study. J. Sleep Res. 2019, 28, e12799. [Google Scholar] [CrossRef] [PubMed]
- Etindele-Sosso, F.A. Insomnia, excessive daytime sleepiness, anxiety, depression and socioeconomic status among customer service employees in Canada. Sleep Sci. 2020, 13, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Etindele Sosso, F.A.; Matos, E. Socioeconomic disparities in obstructive sleep apnea: A systematic review of empirical research. Sleep Breath. 2021, 25, 1729–1739. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, D.; Sosso, F.A.E.; Khoury, T.; Surani, S.R. Sleep Disturbances Are Mediators Between Socioeconomic Status and Health: A Scoping Review. Int. J. Ment. Health Addict. 2020, 20, 480–504. [Google Scholar] [CrossRef]
- Silva-Perez, L.J.; Gonzalez-Cardenas, N.; Surani, S.; Etindele Sosso, F.A.; Surani, S.R. Socioeconomic Status in Pregnant Women and Sleep Quality During Pregnancy. Cureus 2019, 11, e6183. [Google Scholar] [CrossRef]
- Doane, L.D.; Breitenstein, R.S.; Beekman, C.; Clifford, S.; Smith, T.J.; Lemery-Chalfant, K. Early Life Socioeconomic Disparities in Children’s Sleep: The Mediating Role of the Current Home Environment. J. Youth Adolesc. 2019, 48, 56–70. [Google Scholar] [CrossRef]
- Hawkins, S.S.; Takeuchi, D.T. Social determinants of inadequate sleep in US children and adolescents. Public Health 2016, 138, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Jarrin, D.C.; McGrath, J.J.; Silverstein, J.E.; Drake, C. Objective and subjective socioeconomic gradients exist for sleep quality, sleep latency, sleep duration, weekend oversleep, and daytime sleepiness in adults. Behav. Sleep Med. 2013, 11, 144–158. [Google Scholar] [CrossRef] [PubMed]
- Seo, W.H.; Kwon, J.H.; Eun, S.H.; Kim, G.; Han, K.; Choi, B.M. Effect of socio-economic status on sleep. J. Paediatr. Child Health 2017, 53, 592–597. [Google Scholar] [CrossRef] [PubMed]
- Speirs, K.E.; Liechty, J.M.; Wu, C.F. Sleep, but not other daily routines, mediates the association between maternal employment and BMI for preschool children. Sleep Med. 2014, 15, 1590–1593. [Google Scholar] [CrossRef]
- Brug, J.; van Stralen, M.M.; Te Velde, S.J.; Chinapaw, M.J.; De Bourdeaudhuij, I.; Lien, N.; Bere, E.; Maskini, V.; Singh, A.S.; Maes, L.; et al. Differences in weight status and energy-balance related behaviors among schoolchildren across Europe: The ENERGY-project. PLoS ONE 2012, 7, e34742. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, L.J.; Johnson, C.; Crosette, J.; Ramos, M.; Mindell, J.A. Prevalence of diagnosed sleep disorders in pediatric primary care practices. Pediatrics 2010, 125, e1410–e1418. [Google Scholar] [CrossRef]
- Roberts, R.E.; Lee, E.S.; Hemandez, M.; Solari, A.C. Symptoms of insomnia among adolescents in the lower Rio Grande Valley of Texas. Sleep 2004, 27, 751–760. [Google Scholar] [CrossRef]
- Manyanga, T.; Barnes, J.D.; Tremblay, M.S.; Katzmarzyk, P.T.; Broyles, S.T.; Barreira, T.V.; Fogelholm, M.; Hu, G.; Maher, C.; Maia, J.; et al. No evidence for an epidemiological transition in sleep patterns among children: A 12-country study. Sleep Health 2018, 4, 87–95. [Google Scholar] [CrossRef]
- Bagley, E.J.; Kelly, R.J.; Buckhalt, J.A.; El-Sheikh, M. What keeps low-SES children from sleeping well: The role of presleep worries and sleep environment. Sleep Med. 2015, 16, 496–502. [Google Scholar] [CrossRef]
- Marco, C.A.; Wolfson, A.R.; Sparling, M.; Azuaje, A. Family socioeconomic status and sleep patterns of young adolescents. Behav. Sleep Med. 2011, 10, 70–80. [Google Scholar] [CrossRef]
- Acebo, C.; Sadeh, A.; Seifer, R.; Tzischinsky, O.; Hafer, A.; Carskadon, M.A. Sleep/wake patterns derived from activity monitoring and maternal report for healthy 1- to 5-year-old children. Sleep 2005, 28, 1568–1577. [Google Scholar] [CrossRef]
- Harper, S.; Lynch, J. Health Inequalities: Measurement and Decomposition: Oakes JM, Kaufman JS., Methods in Social Epidemiology, 2nd ed.; Jossey-Bass & Pfeiffer Imprint, Wiley: San Francisco, CA, USA, 2017. [Google Scholar]
- Glymour, M.M.; Avendano, M.; Kawachi, I. Socioeconomic status and health. Soc. Epidemiol. 2014, 2, 17–63. [Google Scholar]
| Study | Study Design | Population | Age (Mean ± SD or Range) | Sample Size | Socioeconomic Indicators | Sleep Health Measurement | Interactions and Moderators | Conclusions |
|---|---|---|---|---|---|---|---|---|
| [11] | Cross-sectional | Adult members of a larger cohort in Pittsburgh metropolitan area | 45–75 | 187 | Composite SES score (education and annual income) | Two-night home PSG (sleep duration, sleep latency, sleep efficiency, WASO, sleep architecture, apnea–hypopnea index (AHI)) | Environmental factors (outside noise, room temperature and health worries) and negative effects were statistical mediators of the relationship between SES and PSQI scores | Lower SES was associated with longer sleep latency and more WASO |
| [12] | Cross-sectional | Midlife women from the general population of 4 US cities | 50.72 ± 2.02 | 368 | Educational attainment (college or advanced degree vs without). Financial strain (somewhat to very difficult paying for basics vs not difficult at all) | Three-night home PSG assessing sleep duration, sleep continuity, sleep latency, WASO, sleep efficiency, sleep architecture and power spectral analysis of NREM EEG | N/A | Financial strain was a significant correlate of poorer subjective sleep quality and PSG-assessed sleep continuity |
| [13] | Cross-sectional | Adults from the general population in South Delhi, India | 30–65 | 360 | Kuppuswami socioeconomic status score | OSA (AHI ≥ 5 in PSG) | N/A | Prevalence of OSA was not significantly different across the socio-economic strata |
| [14] | Cross-sectional | Adults recruited through advertisements in San Diego, California | 18–52 | 128 | Childhood SES: highest level of education attained by each parent (low if neither parent achieved education beyond high school, and high if either parent achieved some education beyond high school) | PSG (sleep duration, latency, efficiency, architecture, WASO) | Women from low childhood SES backgrounds had longer sleep latency than women from the high childhood SES background group | Individuals with lower childhood SES spent more time in Stage 2 sleep and less time in SWS than participants from higher childhood SES backgrounds independently of current SES |
| [15] | Cross-sectional | Adults from the general population in Sao Paulo, Brazil | 20–80 | 1042 | Annual household income (high, middle or low) according to the Brazilian Economic Classification Criteria Employment Status (working vs not working) | OSA ICSD-2 criteria (AHI from PSG) | Income affects OSA risk differentially for males and females | Global SES was not associated with OSA |
| [8] | Cross-sectional | Adults from the general population in Lausanne, Switzerland | 40–81 | 3391 | Educational level (high, middle, low). Occupational position (high, middle, low) | Total sleep time, sleep latency, slow wave sleep, sleep efficiency, stage shifts (in-home 1-night PSG) | N/A | Men with a low educational level or occupational position were more likely to suffer from poor sleep quality, short sleep duration and insomnia. Men with a low occupational position were also more likely to have long sleep latency. Women with a low educational level were more likely to have long sleep latency and short sleep duration. Women with a low occupational position were more likely to have long sleep latency, excessive daytime sleepiness and short sleep duration. Participants with low SES had lower sleep efficiency and higher stage shifts in PSG. |
| [16] | Cross-sectional | Adults of a general population cohort in Lausanne, Switzerland | 40–81 | 2162 | Occupation (managers, lower-level executives, low qualified non-manuals and manuals). Education (university, higher secondary, lower secondary or lower) | Home PSG (apnea–hypopnea index (AHI) and ≥ 3% oxygen desaturation index (ODI)) | These associations were mediated by BMI | Lower occupational position was associated with an increased risk of AHI ≥ 30 and ODI ≥ 30. Lower education was associated with an increased risk of ODI ≥15. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Etindele Sosso, F.A. Measuring Sleep Health Disparities with Polysomnography: A Systematic Review of Preliminary Findings. Clocks & Sleep 2022, 4, 80-87. https://doi.org/10.3390/clockssleep4010009
Etindele Sosso FA. Measuring Sleep Health Disparities with Polysomnography: A Systematic Review of Preliminary Findings. Clocks & Sleep. 2022; 4(1):80-87. https://doi.org/10.3390/clockssleep4010009
Chicago/Turabian StyleEtindele Sosso, Faustin Armel. 2022. "Measuring Sleep Health Disparities with Polysomnography: A Systematic Review of Preliminary Findings" Clocks & Sleep 4, no. 1: 80-87. https://doi.org/10.3390/clockssleep4010009
APA StyleEtindele Sosso, F. A. (2022). Measuring Sleep Health Disparities with Polysomnography: A Systematic Review of Preliminary Findings. Clocks & Sleep, 4(1), 80-87. https://doi.org/10.3390/clockssleep4010009





