Dream Recall/Affect and Cortisol: An Exploratory Study
Abstract
1. Introduction
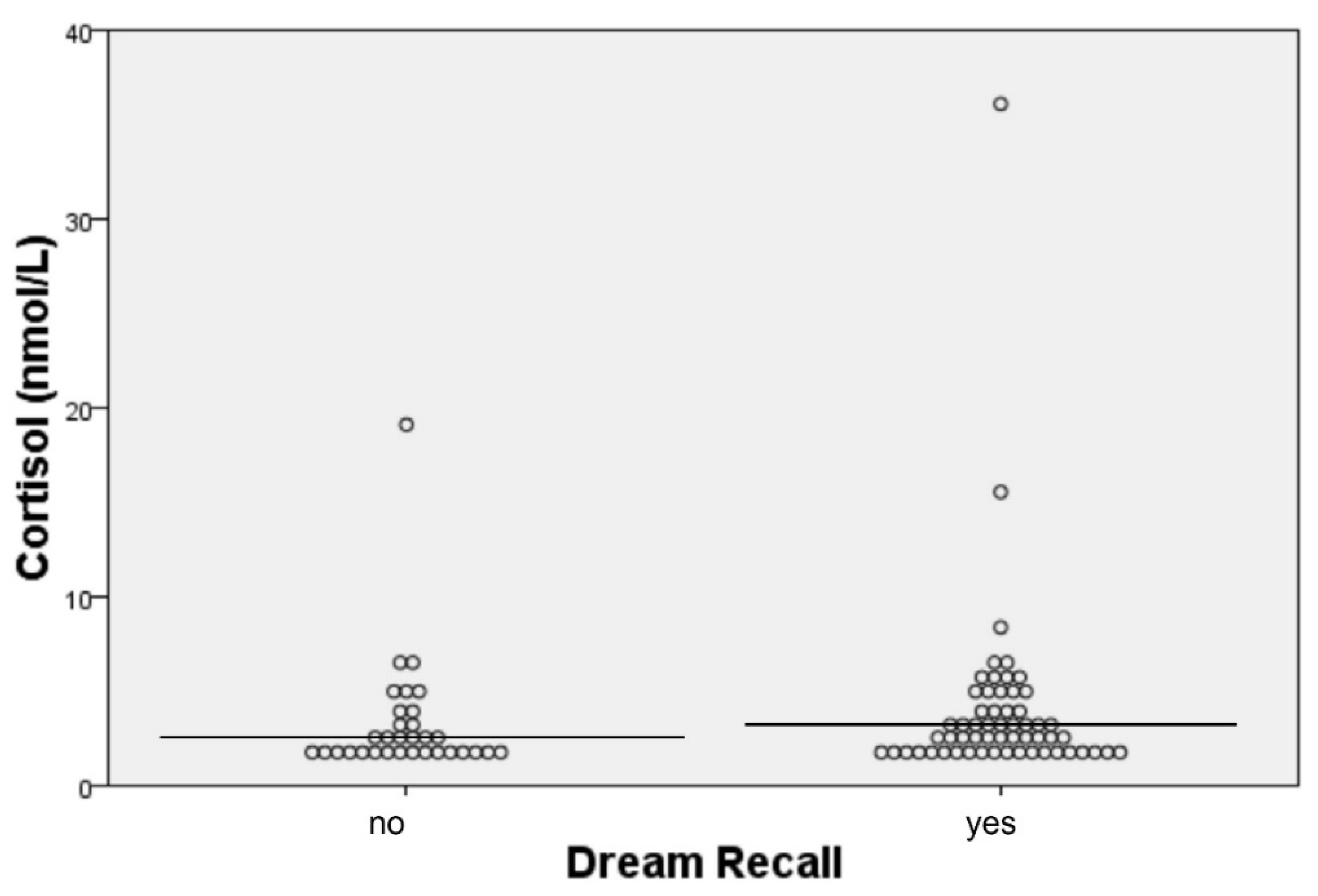
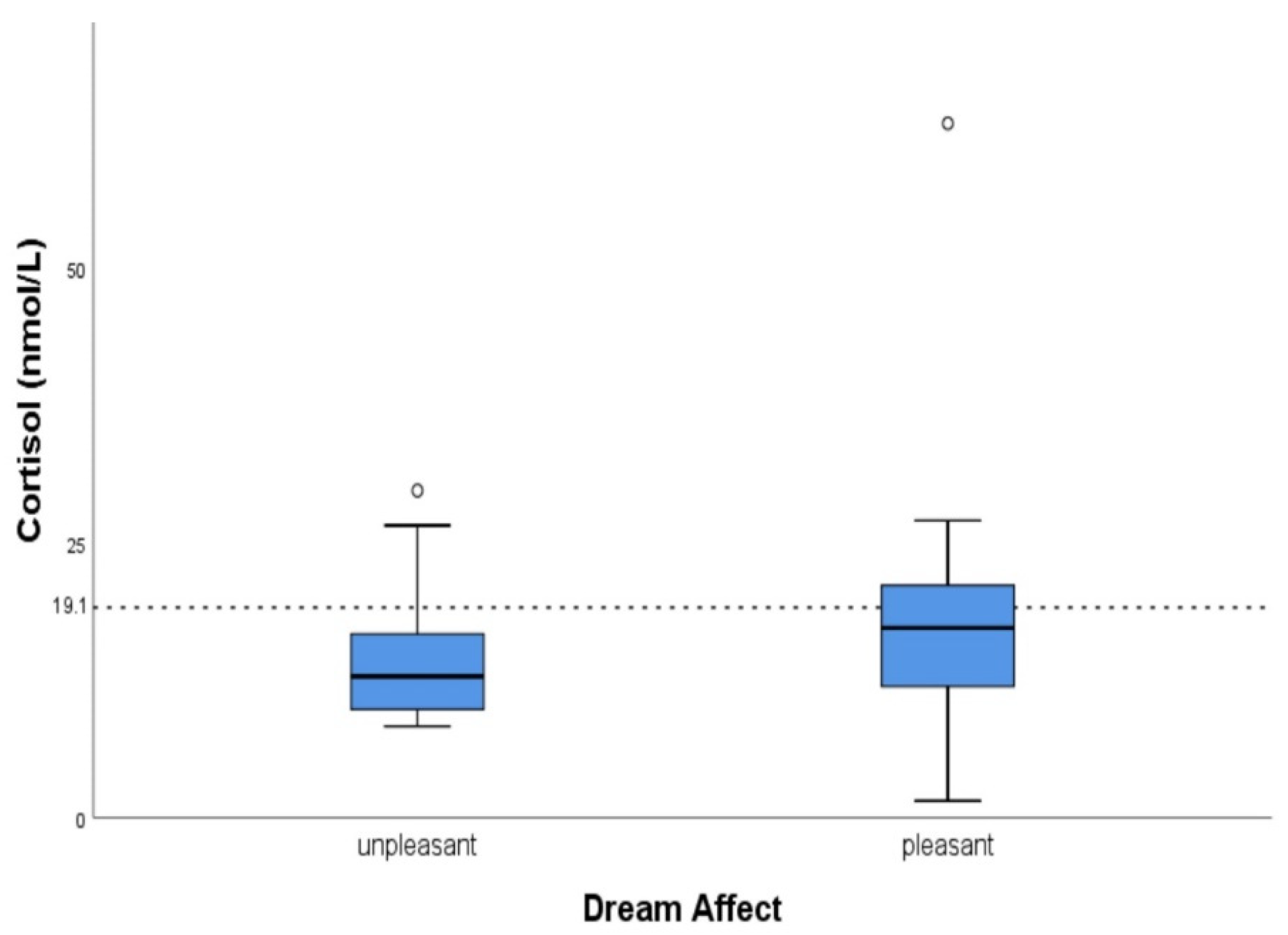
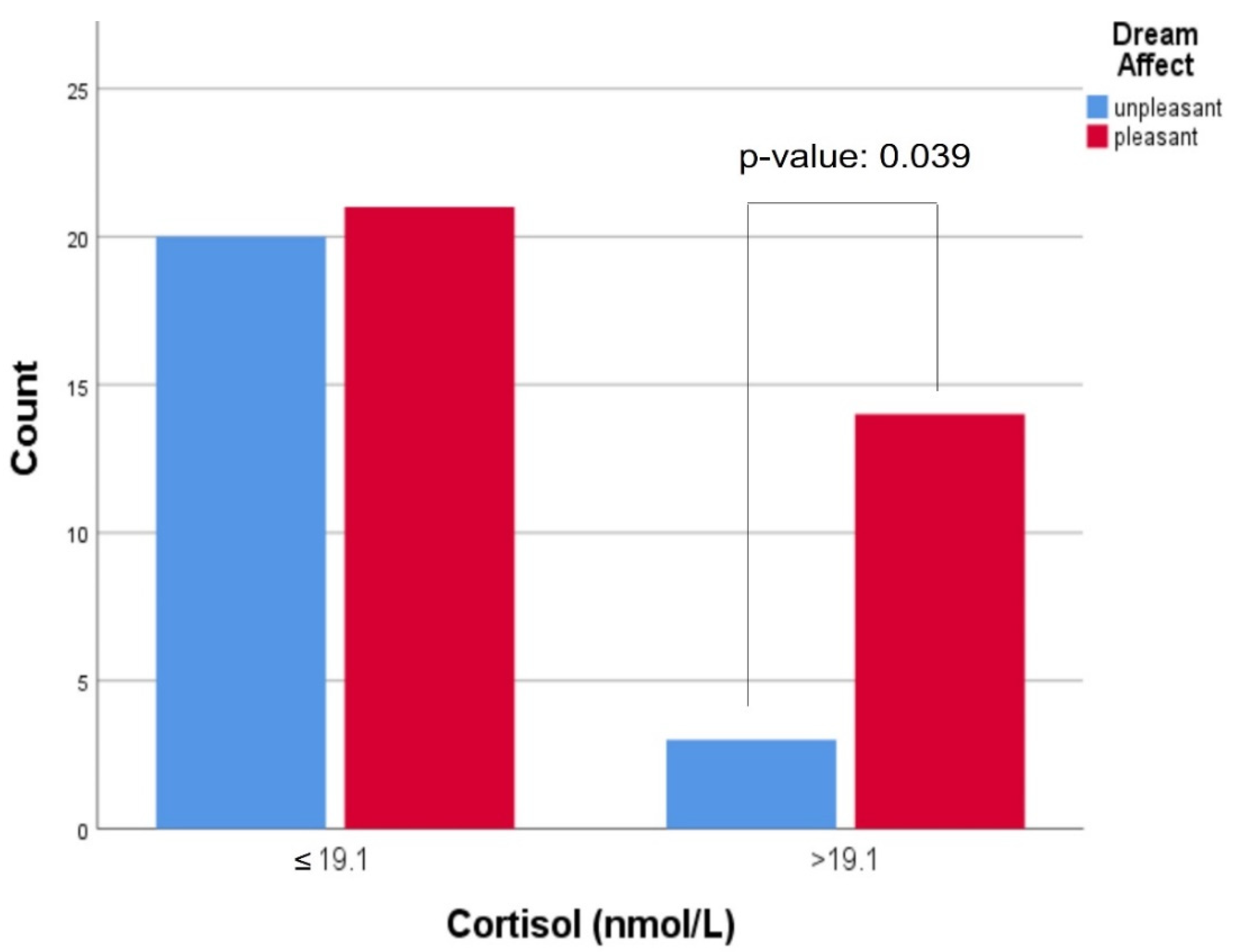
2. Results
3. Discussion
4. Materials and Methods
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eichenlaub, J.-B.; Nicolas, A.; Daltrozzo, J.; Redouté, J.; Costes, N.; Ruby, P. Resting Brain Activity Varies with Dream Recall Frequency Between Subjects. Neuropsychopharmacology 2014, 39, 1594–1602. [Google Scholar] [CrossRef] [PubMed]
- Ruby, P.M.; Blochet, C.; Eichenlaub, J.-B.; Bertrand, O.; Morlet, D.; Bidet-Caulet, A. Alpha reactivity to first names differs in subjects with high and low dream recall frequency. Front. Psychol. 2013, 4, 419. [Google Scholar] [CrossRef] [PubMed]
- Pagel, J.F. What physicians need to know about dreams and dreaming. Curr. Opin. Pulm. Med. 2012, 18, 574–579. [Google Scholar] [CrossRef] [PubMed]
- Ebben, M.; Lequerica, A.; Spielman, A. Effects of pyridoxine on dreaming: A preliminary study. Percept. Mot. Skills 2002, 94, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Pace-Schott, E.F.; Gersh, T.; Silvestri, R.; Stickgold, R.; Salzman, C.; Hobson, J.A. SSRI Treatment suppresses dream recall frequency but increases subjective dream intensity in normal subjects. J. Sleep Res. 2001, 10, 129–142. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tselebis, A.; Zoumakis, E.; Ilias, I. Dream Recall/Affect and the Hypothalamic–Pituitary–Adrenal Axis. Clocks Sleep 2021, 3, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Lightman, S.L.; Birnie, M.T.; Conway-Campbell, B.L. Dynamics of ACTH and Cortisol Secretion and Implications for Disease. Endocr. Rev. 2020, 41, bnaa002. [Google Scholar] [CrossRef]
- Payne, J.D.; Nadel, L. Sleep, dreams, and memory consolidation: The role of the stress hormone cortisol. Learn. Mem. 2004, 11, 671–678. [Google Scholar] [CrossRef]
- Payne, J.D. Memory consolidation, the diurnal rhythm of cortisol, and the nature of dreams: A new hypothesis. Int. Rev. Neurobiol. 2010, 92, 101–134. [Google Scholar]
- Hill, A.R.; Spencer-Segal, J.L. Glucocorticoids and the Brain after Critical Illness. Endocrinology 2021, 162, 242. [Google Scholar] [CrossRef]
- Spanò, G.; Pizzamiglio, G.; McCormick, C.; Clark, I.A.; De Felice, S.; Miller, T.D.; Edgin, J.O.; Rosenthal, C.R.; Maguire, E.A. Dreaming with hippocampal damage. eLife 2020, 9, 56211. [Google Scholar] [CrossRef] [PubMed]
- Feld, G.B.; Born, J. Neurochemical mechanisms for memory processing during sleep: Basic findings in humans and neuropsychiatric implications. Neuropsychopharmacology 2019, 45, 31–44. [Google Scholar] [CrossRef] [PubMed]
- Paul, F.; Alpers, G.W.; Reinhard, I.; Schredl, M. Nightmares do result in psychophysiological arousal: A multimeasure ambulatory assessment study. Psychophysiology 2019, 56, e13366. [Google Scholar] [CrossRef]
- Nagy, T.; Salavecz, G.; Simor, P.; Purebl, G.; Bódizs, R.; Dockray, S.; Steptoe, A. Frequent nightmares are associated with blunted cortisol awakening response in women. Physiol. Behav. 2015, 147, 233–237. [Google Scholar] [CrossRef]
- Hess, G.; Schredlb, M.; Gierens, A.; Domes, G. Effects of nightmares on the cortisol awakening response: An ambulatory assessment pilot study. Psychoneuroendocrinology 2020, 122, 104900. [Google Scholar] [CrossRef] [PubMed]
- Starkman, M.N.; Schteingart, D.E. Neuropsychiatric manifestations of patients with Cushing’s syndrome. Relationship to cortisol and adrenocorticotropic hormone levels. Arch. Intern. Med. 1981, 141, 215–219. [Google Scholar] [CrossRef]
- Asarnow, L.D. Depression and sleep: What has the treatment research revealed and could the HPA axis be a potential mechanism? Curr. Opin. Psychol. 2020, 34, 112–116. [Google Scholar] [CrossRef]
- Edge, L.C. The role of emotional brain processing during sleep in depression. J. Psychiatr. Ment. Health Nurs. 2010, 17, 857–861. [Google Scholar] [CrossRef]
- Ilias, I.; Economou, N.-T.; Lekkou, A.; Romigi, A.; Koukkou, E. Dream Recall and Content versus the Menstrual Cycle: A Cross-Sectional Study in Healthy Women. Med. Sci. 2019, 7, 81. [Google Scholar] [CrossRef]
- Taylor, P.N.; Muller, I.; Nana, M.; Velasco, I.; Lazarus, J.H. Indications for treatment of subclinical hypothyroidism and isolated hypothyroxinaemia in pregnancy. Best Pr. Res. Clin. Endocrinol. Metab. 2020, 34, 101436. [Google Scholar] [CrossRef]
- Nielsen, T.; Levin, R. Nightmares: A new neurocognitive model. Sleep Med. Rev. 2007, 11, 295–310. [Google Scholar] [CrossRef] [PubMed]
- Schultz, K.J.; Koulack, D. Dream Affect and the Menstrual Cycle. J. Nerv. Ment. Dis. 1980, 168, 436–438. [Google Scholar] [CrossRef] [PubMed]
- Sheldrake, P.; Cormack, M. Dream recall and the menstrual cycle. J. Psychosom. Res. 1974, 18, 347–350. [Google Scholar] [CrossRef]
- Mangiaruga, A.; Scarpelli, S.; Bartolacci, C.; De Gennaro, L. Spotlight on dream recall: The ages of dreams. Nat. Sci. Sleep 2018, 10, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Scarpelli, S.; Bartolacci, C.; D’Atri, A.; Gorgoni, M.; De Gennaro, L. The Functional Role of Dreaming in Emotional Processes. Front. Psychol. 2019, 10, 459. [Google Scholar] [CrossRef] [PubMed]
- Roehrs, T.; Papineau, K.; Rosenthal, L.; Roth, T. Ethanol as a Hypnotic in Insomniacs Self Administration and Effects on Sleep and Mood. Neuropsychopharmacology 1999, 20, 279–286. [Google Scholar] [CrossRef]
| Sampling Time | Men | Women (Follicular Phase) | Women (Luteal Phase) | |||
|---|---|---|---|---|---|---|
| Cortisol *: Median (Q1–Q3) | Dream Recall (Positive Affect **) | Cortisol *: Median (Q1–Q3) | Dream Recall (Positive Affect **) | Cortisol *: Median (Q1–Q3) | Dream Recall (Positive Affect **) | |
| Day 1 Evening | 3.1 (1.5–5.46) | 9/15 (8/9) | 2.5 (1.9–3.25) | 12/15 (8/12) | 2.64 (1.5–4.68) | 9/15 (3/9) |
| Day 2 Morning | 14.88 (11.6–20.45) | 13.68 (11.32–23.15) | 12.19 (8.46–17.42) | |||
| Day 2 Evening | 3.03 (1.64–6.06) | 7/15 (3/7) | 2.89 (1.5–3.71) | 11/15 (6/11) | 1.98 (1.5–2.89) | 10/15 (7/10) |
| Day 3 Morning | 15.18 (11.11–19.98) | 18.55 (12.82–21.76) | 12.63 (9.45–18.5) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Triantafyllou, A.S.; Ilias, I.; Economou, N.-T.; Pappa, A.; Koukkou, E.; Steiropoulos, P. Dream Recall/Affect and Cortisol: An Exploratory Study. Clocks & Sleep 2022, 4, 9-15. https://doi.org/10.3390/clockssleep4010003
Triantafyllou AS, Ilias I, Economou N-T, Pappa A, Koukkou E, Steiropoulos P. Dream Recall/Affect and Cortisol: An Exploratory Study. Clocks & Sleep. 2022; 4(1):9-15. https://doi.org/10.3390/clockssleep4010003
Chicago/Turabian StyleTriantafyllou, Alexandros S., Ioannis Ilias, Nicholas-Tiberio Economou, Athina Pappa, Eftychia Koukkou, and Paschalis Steiropoulos. 2022. "Dream Recall/Affect and Cortisol: An Exploratory Study" Clocks & Sleep 4, no. 1: 9-15. https://doi.org/10.3390/clockssleep4010003
APA StyleTriantafyllou, A. S., Ilias, I., Economou, N.-T., Pappa, A., Koukkou, E., & Steiropoulos, P. (2022). Dream Recall/Affect and Cortisol: An Exploratory Study. Clocks & Sleep, 4(1), 9-15. https://doi.org/10.3390/clockssleep4010003







