No Effect of Chronotype on Sleepiness, Alertness, and Sustained Attention during a Single Night Shift
Abstract
:1. Introduction
2. Results
2.1. Chronotype and Habitual Sleep Markers
2.2. Subjective Sleepiness
2.3. Subjective Alertness
2.4. PVT Reciprocal Response Time
2.5. PVT Lapses
2.6. Decile-Based Chronotypes
3. Discussion
4. Materials and Methods
4.1. Participants
4.2. Procedure
4.3. Measures
4.3.1. Dim Light Melatonin Onset (DLMO)
4.3.2. Sleep Markers
4.3.3. Subjective Sleepiness and Alertness
4.3.4. Sustained Attention
4.4. Statistical Analyses
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alterman, T.; Luckhaupt, S.E.; Dahlhamer, J.M.; Ward, B.W.; Calvert, G.M. Prevalence rates of work organization characteristics among workers in the U.S.: Data from the 2010 National Health Interview Survey. Am. J. Ind. Med. 2013, 56, 647–659. [Google Scholar] [CrossRef] [Green Version]
- Eurofound. Fifth European Working Conditions Survey; Publications Office of the European Union: Luxembourg, 2012. [Google Scholar]
- Åkerstedt, T. Is there an optimal sleep-wake pattern in shift work? Scand. J. Work. Environ. Health 1998, 24, 18–27. [Google Scholar]
- Juda, M.; Vetter, C.; Roenneberg, T. Chronotype modulates sleep duration, sleep quality, and social jet lag in shift-workers. J. Biol. Rhythm. 2013, 28, 141–151. [Google Scholar] [CrossRef] [Green Version]
- Dijk, D.J.; Duffy, J.F.; Czeisler, C.A. Circadian and sleep/wake dependent aspects of subjective alertness and cognitive performance. J. Sleep Res. 1992, 1, 112–117. [Google Scholar] [CrossRef]
- Czeisler, C.A.; Gooley, J.J. Sleep and Circadian Rhythms in Humans; Cold Spring Harbor Laboratory Press: Cold Spring Harbor, NY, USA, 2007; pp. 579–597. [Google Scholar]
- Santhi, N.; Horowitz, T.S.; Duffy, J.F.; Czeisler, C.A. Acute sleep deprivation and circadian misalignment associated with transition onto the first night of work impairs visual selective attention. PLoS ONE 2007, 2, e1233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Åkerstedt, T. Work hours, sleepiness and accidents Introduction and summary. J. Sleep Res. 1995, 4, 1–3. [Google Scholar] [CrossRef]
- Knauth, P.; Landau, K.; Dröge, C.; Schwitteck, M.; Widynski, M.; Rutenfranz, J. Duration of sleep depending on the type of shift work. Int. Arch. Occup. Environ. Health 1980, 46, 167–177. [Google Scholar] [CrossRef]
- Lamond, N.; Dorrian, J.; Burgess, H.; Holmes, A.; Roach, G.; McCulloch, K.; Fletcher, A.; Dawson, D. Adaptation of performance during a week of simulated night work. Ergonomics 2004, 47, 154–165. [Google Scholar] [CrossRef] [PubMed]
- Saksvik, I.B.; Bjorvatn, B.; Hetland, H.; Sandal, G.M.; Pallesen, S. Individual differences in tolerance to shift work—A systematic review. Sleep Med. Rev. 2011, 15, 221–235. [Google Scholar] [CrossRef] [PubMed]
- Fischer, D.; Lombardi, D.A.; Marucci-Wellman, H.; Roenneberg, T. Chronotypes in the US—Influence of age and sex. PLoS ONE 2017, 12, e0178782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social jetlag: Misalignment of biological and social time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef]
- Roenneberg, T.; Kuehnle, T.; Juda, M.; Kantermann, T.; Allebrandt, K.; Gordijn, M.; Merrow, M. Epidemiology of the human circadian clock. Sleep Med. Rev. 2007, 11, 429–438. [Google Scholar] [CrossRef] [Green Version]
- Roenneberg, T.; Wirz-Justice, A.; Merrow, M. Life between clocks: Daily temporal patterns of human chronotypes. J. Biol. Rhythm. 2003, 18, 80–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adan, A.; Archer, S.N.; Hidalgo, M.P.; Di Milia, L.; Natale, V.; Randler, C. Circadian typology: A comprehensive review. Chronobiol. Int. 2012, 29, 1153–1175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gamble, K.L.; Young, M.E. Circadian biology: The early bird catches the morning shift. Curr. Biol. 2015, 25, R269–R271. [Google Scholar] [CrossRef] [Green Version]
- Kantermann, T.; Eastman, C.I. Circadian phase, circadian period and chronotype are reproducible over months. Chronobiol. Int. 2018, 35, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.; Tanigawa, T.; Takahashi, M.; Mutou, K.; Tachibana, N.; Kage, Y.; Iso, H. Shiftwork locus of control, situational and behavioural effects on sleepiness and fatigue in shiftworkers. Ind. Health 2005, 43, 151–170. [Google Scholar] [CrossRef] [Green Version]
- Gamble, K.L.; Motsinger-Reif, A.A.; Hida, A.; Borsetti, H.M.; Servick, S.V.; Ciarleglio, C.M.; Robbins, S.; Hicks, J.; Carver, K.; Hamilton, N.; et al. Shift work in nurses: Contribution of phenotypes and genotypes to adaptation. PLoS ONE 2011, 6, e18395. [Google Scholar] [CrossRef] [Green Version]
- Vetter, C.; Fischer, D.; Matera, J.L.; Roenneberg, T. Aligning work and circadian time in shift workers improves sleep and reduces circadian disruption. Curr. Biol. 2015, 25, 907–911. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Newey, C.A.; Hood, B.M. Determinants of shift-work adjustment for nursing staff: The critical experience of partners. J. Prof. Nurs. 2004, 20, 187–195. [Google Scholar] [CrossRef]
- Reinke, L.; Ozbay, Y.; Dieperink, W.; Tulleken, J.E. The effect of chronotype on sleepiness, fatigue, and psychomotor vigilance of ICU nurses during the night shift. Intensive Care Med. 2015, 41, 657–666. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horne, J.A.; Ostberg, O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int. J. Chronobiol. 1976, 4, 97–110. [Google Scholar]
- Roenneberg, T.; Keller, L.K.; Fischer, D.; Matera, J.L.; Vetter, C.; Winnebeck, E.C. Human activity and rest in situ. Methods Enzymol. 2015, 552, 257–283. [Google Scholar]
- Burgess, H.J.; Eastman, C.I. The dim light melatonin onset following fixed and free sleep schedules. J. Sleep Res. 2005, 14, 229–237. [Google Scholar] [CrossRef]
- Ritchie, H.K.; Burke, T.M.; Dear, T.B.; McHill, A.W.; Axelsson, J.; Wright, K.P., Jr. Impact of sleep inertia on visual selective attention for rare targets and the influence of chronotype. J. Sleep Res. 2017, 26, 551–558. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kantermann, T.; Sung, H.; Burgess, H.J. Comparing the morningness-eveningness questionnaire and munich chronotype questionnaire to the dim light melatonin onset. J. Biol. Rhythm. 2015, 30, 449–453. [Google Scholar] [CrossRef] [Green Version]
- Dinges, D.F.; Powell, J.W. Microcomputer analyses of performance on a portable, simple visual RT task during sustained operations. Behav. Res. Methods Instrum. Comput. 1985, 17, 652–655. [Google Scholar] [CrossRef]
- Vetter, C.; Juda, M.; Roenneberg, T. The influence of internal time, time awake, and sleep duration on cognitive performance in shiftworkers. Chronobiol. Int. 2012, 29, 1127–1138. [Google Scholar] [CrossRef] [PubMed]
- Basner, M.; Dinges, D.F. Maximizing sensitivity of the psychomotor vigilance test (PVT) to sleep loss. Sleep 2011, 34, 581–591. [Google Scholar] [CrossRef]
- Rajaratnam, S.M.; Arendt, J. Health in a 24-h society. Lancet 2001, 358, 999–1005. [Google Scholar] [CrossRef]
- Lim, J.; Dinges, D.F. Sleep deprivation and vigilant attention. Ann. N. Y. Acad. Sci. 2008, 1129, 305–322. [Google Scholar] [CrossRef] [PubMed]
- Isherwood, C.M.; Chinoy, E.D.; Murphy, A.S.; Kim, J.H.; Wang, W.; Duffy, J.F. Scheduled afternoon-evening sleep leads to better night shift performance in older adults. Occup. Environ. Med. 2020, 77, 179–184. [Google Scholar] [CrossRef]
- Chinoy, E.D.; Harris, M.P.; Kim, M.J.; Wang, W.; Duffy, J.F. Scheduled evening sleep and enhanced lighting improve adaptation to night shift work in older adults. Occup. Environ. Med. 2016, 73, 869–876. [Google Scholar] [CrossRef] [PubMed]
- Kosmadopoulos, A.; Zhou, X.; Roach, G.D.; Darwent, D.; Sargent, C. No first night shift effect observed following a nocturnal main sleep and a prophylactic 1-h afternoon nap. Chronobiol. Int. 2016, 33, 716–720. [Google Scholar] [CrossRef] [PubMed]
- Van Dongen, H.P.; Vitellaro, K.M.; Dinges, D.F. Individual differences in adult human sleep and wakefulness: Leitmotif for a research agenda. Sleep 2005, 28, 479–496. [Google Scholar] [CrossRef] [Green Version]
- Lo, J.C.; Groeger, J.A.; Santhi, N.; Arbon, E.L.; Lazar, A.S.; Hasan, S.; von Schantz, M.; Archer, S.N.; Dijk, D.J. Effects of partial and acute total sleep deprivation on performance across cognitive domains, individuals and circadian phase. PLoS ONE 2012, 7, e45987. [Google Scholar] [CrossRef] [Green Version]
- Voultsios, A.; Kennaway, D.J.; Dawson, D. Salivary melatonin as a circadian phase marker: Validation and comparison to plasma melatonin. J. Biol. Rhythm. 1997, 12, 457–466. [Google Scholar] [CrossRef] [PubMed]
- Akerstedt, T.; Gillberg, M. Subjective and objective sleepiness in the active individual. Int. J. Neurosci. 1990, 52, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Dorrian, J.; Lamond, N.; Holmes, A.L.; Burgess, H.J.; Roach, G.D.; Fletcher, A.; Dawson, D. The ability to self-monitor performance during a week of simulated night shifts. Sleep 2003, 26, 871–877. [Google Scholar] [CrossRef] [Green Version]


| Reported Differences between Chronotypes When Working Night Shift | Reference |
|---|---|
| Early chronotypes showed shorter daytime sleep duration and higher levels of daytime sleep disturbance than late chronotypes. | [4] |
| Early chronotypes showed lower daytime sleep quality and higher night shift drowsiness than late chronotypes. | [19] |
| Early chronotypes showed lower self-reported adaptation to the shift than late chronotypes. | [20] |
| Extreme early chronotypes whose rosters were adjusted to exclude night shifts showed increased sleep duration, sleep quality, and well-being compared to when their rosters included night shifts. | [21] |
| No effect of chronotype on daytime sleep problems. | [22] |
| No effect of chronotype on daytime sleep quality or duration, performance on psychomotor tests, mathematical tasks, subjective sleepiness, or subjective fatigue. | [23] |
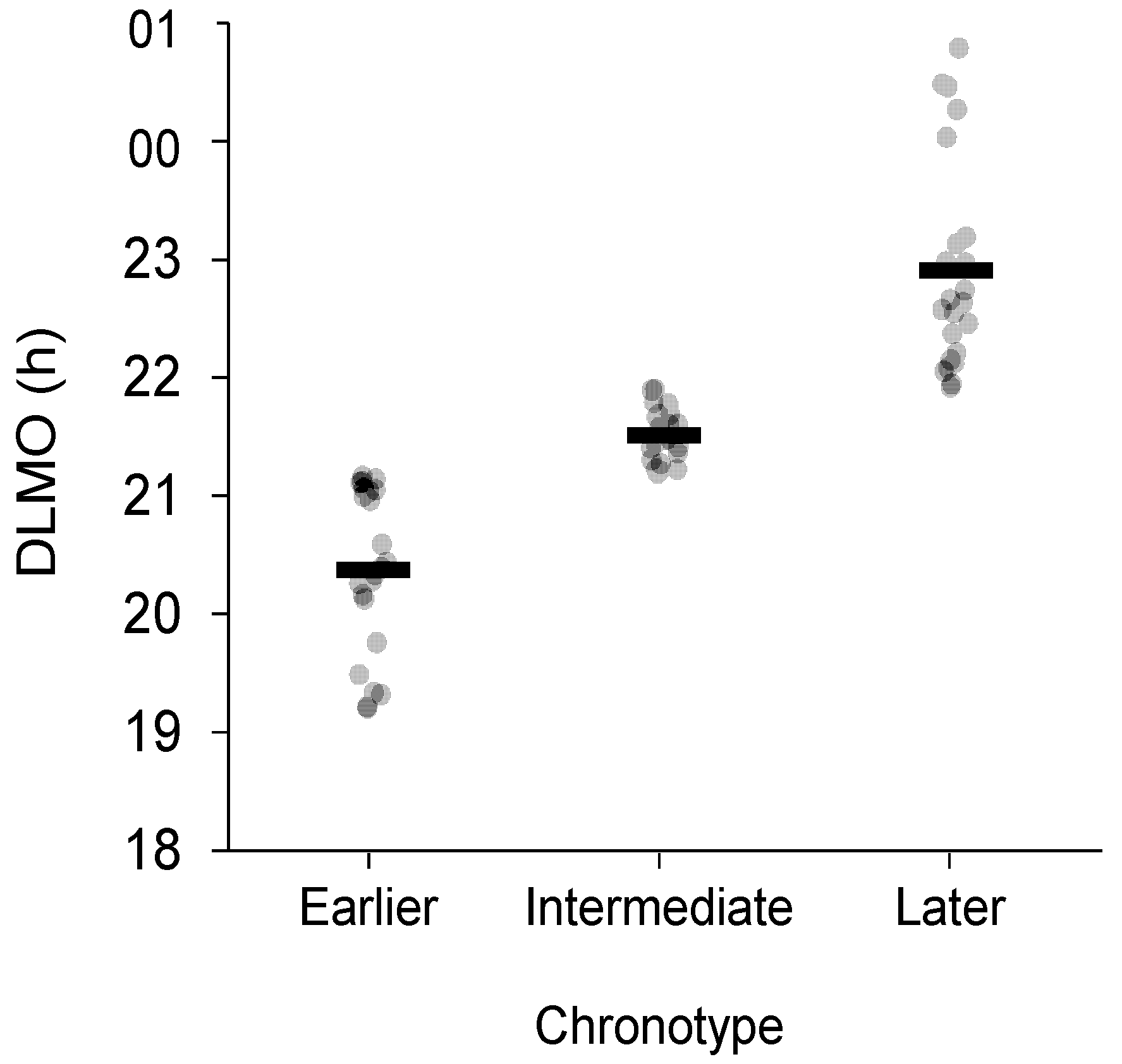
| Chronotype | N | DLMO M(SD), (Range) (hh:mm) | Habitual Sleep Onset b M(SD) (hh:mm) | Habitual Sleep Offset b M(SD) (hh:mm) |
|---|---|---|---|---|
| Earlier | 23 (11f, 12m) | 20:22(0:42), (19:12–21:10) | 23:06(0:53) | 07:16(0:49) |
| Intermediate | 24 (11f, 13m) | 21:31(0:13), (21:11–21:53) | 23:42(0:46) | 08:24(0:56) |
| Later | 23 (12f, 11m) | 22:54(0:54), (21:54–00:47) | 00:16(0:59) | 08:51(1:14) |
| Total | 70 (35f, 35m) a | 21:35(1:13), (19:12–00:47) | 23:41(0:59) | 08:10(1:11) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reiter, A.M.; Sargent, C.; Roach, G.D. No Effect of Chronotype on Sleepiness, Alertness, and Sustained Attention during a Single Night Shift. Clocks & Sleep 2021, 3, 377-386. https://doi.org/10.3390/clockssleep3030024
Reiter AM, Sargent C, Roach GD. No Effect of Chronotype on Sleepiness, Alertness, and Sustained Attention during a Single Night Shift. Clocks & Sleep. 2021; 3(3):377-386. https://doi.org/10.3390/clockssleep3030024
Chicago/Turabian StyleReiter, Andrew M., Charli Sargent, and Gregory D. Roach. 2021. "No Effect of Chronotype on Sleepiness, Alertness, and Sustained Attention during a Single Night Shift" Clocks & Sleep 3, no. 3: 377-386. https://doi.org/10.3390/clockssleep3030024
APA StyleReiter, A. M., Sargent, C., & Roach, G. D. (2021). No Effect of Chronotype on Sleepiness, Alertness, and Sustained Attention during a Single Night Shift. Clocks & Sleep, 3(3), 377-386. https://doi.org/10.3390/clockssleep3030024







