Poor Subjective Sleep Quality Is Associated with Poor Occupational Outcomes in Elite Soldiers
Abstract
1. Introduction
1.1. Sleep and Emotional Exhaustion
1.2. Sleep and Functional Impairment
1.3. Sleep and Role Overload
1.4. Daytime Sleepiness
1.5. The Current Study
2. Results
3. Discussion
3.1. Implications and Future Directions
3.2. Study Limitations
4. Materials and Methods
4.1. Participants
4.2. Study Design
4.3. Survey Measures
4.4. Statistical Analyses
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| PSQI | Pittsburgh Sleep Quality Index |
| EE | Emotional exhaustion |
| FI | Functional impairment |
| RO | Role overload |
| DS | Daytime sleepiness |
References
- O’Leary, K.; Bylsma, L.M.; Rottenberg, J. Why might poor sleep quality lead to depression? A role for emotion regulation. Cogn. Emot. 2017, 31, 1698–1706. [Google Scholar] [CrossRef]
- Ulmer, C.S.; Edinger, J.D.; Calhoun, P.S. A Multi-Component Cognitive-Behavioral Intervention for Sleep Disturbance in Veterans with PTSD: A Pilot Study. JCSM Off. Publ. Am. Acad. Sleep Med. 2011, 7, 57. [Google Scholar] [CrossRef]
- Bryant, P.A.; Trinder, J.; Curtis, N. Sick and tired: Does sleep have a vital role in the immune system? Nat. Rev. Immunol. 2004, 4, 457–467. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.J.; Hu, F.B.; Patel, S.R.; Mantzoros, C.S. Sleep duration and snoring in relation to biomarkers of cardiovascular disease risk among women with type 2 diabetes. Diabetes Care 2007, 30, 1233–1240. [Google Scholar] [CrossRef] [PubMed]
- Zencirci, A.D.; Arslan, S. Morning-evening type and burnout level as factors influencing sleep quality of shift nurses: A questionnaire study. Croat. Med. J. 2011, 52, 527–537. [Google Scholar] [CrossRef]
- Scott, L.D.; Arslanian-Engoren, C.; Engoren, M.C. Association of sleep and fatigue with decision regret among critical care nurses. Am. J. Crit. Care 2014, 23, 13–23. [Google Scholar] [CrossRef]
- Suzuki, K.; Ohida, T.; Kaneita, Y.; Yokoyama, E.; Uchiyama, M. Daytime sleepiness, sleep habits and occupational accidents among hospital nurses. J. Adv. Nurs. 2005, 52, 445–453. [Google Scholar] [CrossRef]
- Goldberg, R.; Boss, R.W.; Chan, L.; Goldberg, J.; Mallon, W.K.; Moradzadeh, D.; Goodman, E.A.; McConkie, M.L. Burnout and its correlates in emergency physicians: Four years’ experience with a wellness booth. Acad. Emerg. Med. 1996, 3, 1156–1164. [Google Scholar] [CrossRef]
- Vela-Bueno, A.; Moreno-Jiménez, B.; Rodríguez-Muñoz, A.; Olavarrieta-Bernardino, S.; Fernández-Mendoza, J.; De la Cruz-Troca, J.J.; Bixler, E.O.; Vgontzas, A.N. Insomnia and sleep quality among primary care physicians with low and high burnout levels. J. Psychosom. Res. 2008, 64, 435–442. [Google Scholar] [CrossRef]
- Patterson, P.D.; Weaver, M.D.; Frank, R.C.; Warner, C.W.; Martin-Gill, C.; Guyette, F.X.; Fairbanks, R.J.; Hubble, M.W.; Songer, T.J.; Callaway, C.W. Association between poor sleep, fatigue, and safety outcomes in emergency medical services providers. Prehosp. Emerg. Care 2012, 16, 86–97. [Google Scholar] [CrossRef]
- Orasanu, J.M.; Backer, P. Stress and Military Performance; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1996. [Google Scholar]
- Wilcox, V.L. Burnout in military personnel. Mil. Psychiatry Prep. Peace War 2000, 31–49. [Google Scholar]
- Maslach, C.; Jackson, S.E.; Leiter, M.P.; Schaufeli, W.B.; Schwab, R.L. Maslach Burnout Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1986; Volume 21. [Google Scholar]
- Schutte, N.; Toppinen, S.; Kalimo, R.; Schaufeli, W. The factorial validity of the Maslach Burnout Inventory-General Survey (MBI-GS) across occupational groups and nations. J. Occup. Organ. Psychol. 2000, 73, 53–66. [Google Scholar] [CrossRef]
- Figueiredo-Ferraz, H.; Grau-Alberola, E.; Gil-Monte, P.R.; García-Juesas, J.A. Burnout and job satisfaction among nursing professionals. Psicothema 2012, 24, 271–276. [Google Scholar] [PubMed]
- Lizano, E.L.; Barak, M.M. Job burnout and affective wellbeing: A longitudinal study of burnout and job satisfaction among public child welfare workers. Child. Youth Serv. Rev. 2015, 55, 18–28. [Google Scholar] [CrossRef]
- Wright, T.A.; Cropanzano, R. Emotional exhaustion as a predictor of job performance and voluntary turnover. J. Appl. Psychol. 1998, 83, 486. [Google Scholar] [CrossRef]
- Saxton, M.J.; Phillips, J.S.; Blakeney, R.N. Antecedents and consequences of emotional exhaustion in the airline reservations service sector. Hum. Relat. 1991, 44, 583–595. [Google Scholar] [CrossRef]
- Demerouti, E.; Le Blanc, P.M.; Bakker, A.B.; Schaufeli, W.B.; Hox, J. Present but sick: A three-wave study on job demands, presenteeism and burnout. Career Dev. Int. 2009, 14, 50–68. [Google Scholar] [CrossRef]
- Ahola, K.; Toppinen-Tanner, S.; Huuhtanen, P.; Koskinen, A.; Väänänen, A. Occupational burnout and chronic work disability: An eight-year cohort study on pensioning among Finnish forest industry workers. J. Affect. Disord. 2009, 115, 150–159. [Google Scholar] [CrossRef]
- Ahola, K.; Väänänen, A.; Koskinen, A.; Kouvonen, A.; Shirom, A. Burnout as a predictor of all-cause mortality among industrial employees: A 10-year prospective register-linkage study. J. Psychosom. Res. 2010, 69, 51–57. [Google Scholar] [CrossRef]
- Palmer, C.A.; Alfano, C.A. Sleep and Emotion Regulation: An Organizing, Integrative Review. Sleep Med. Rev. 2016, 31, 6–16. [Google Scholar]
- Mantua, J.; Helms, S.M.; Weymann, K.B.; Capaldi, V.F.; Lim, M.M. Sleep quality and emotion regulation interact to predict anxiety in veterans with PTSD. Behav. Neurol. 2018, 2018. [Google Scholar] [CrossRef]
- Cunningham, T.J.; Payne, J.D. Emotional memory consolidation during sleep. In Cognitive Neuroscience of Memory Consolidation; Springer: Gewerbestrasse, Cham, Switzerland, 2017; pp. 133–159. [Google Scholar]
- Mantua, J.; Henry, O.; Garskovas, N.; Spencer, R.M.C. Mild Traumatic Brain Injury Chronically Impacts Sleep-dependent Emotional Processing. Sleep 2017, 40, zsx062. [Google Scholar] [CrossRef] [PubMed]
- Brand, S.; Beck, J.; Hatzinger, M.; Harbaugh, A.; Ruch, W.; Holsboer-Trachsler, E. Associations between satisfaction with life, burnout-related emotional and physical exhaustion, and sleep complaints. World J. Biol. Psychiatry 2010, 11, 744–754. [Google Scholar] [CrossRef] [PubMed]
- Pagnin, D.; de Queiroz, V.; Carvalho, Y.T.M.S.; Dutra, A.S.S.; Amaral, M.B.; Queiroz, T.T. The relation between burnout and sleep disorders in medical students. Acad. Psychiatry 2014, 38, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Wolf, M.R.; Rosenstock, J.B. Inadequate sleep and exercise associated with burnout and depression among medical students. Acad. Psychiatry 2017, 41, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Sonnenschein, M.; Sorbi, M.J.; Verbraak, M.J.; Schaufeli, W.B.; Maas, C.J.; Van Doornen, L.J. Influence of sleep on symptom improvement and return to work in clinical burnout. Scand. J. Work Environ. Health 2008, 34, 23–32. [Google Scholar] [CrossRef][Green Version]
- Goldman, S.E.; Stone, K.L.; Ancoli-Israel, S.; Blackwell, T.; Ewing, S.K.; Boudreau, R.; Cauley, J.A.; Hall, M.; Matthews, K.A.; Newman, A.B. Poor sleep is associated with poorer physical performance and greater functional limitations in older women. Sleep 2007, 30, 1317–1324. [Google Scholar] [CrossRef]
- Boland, E.M.; Alloy, L.B. Sleep disturbance and cognitive deficits in bipolar disorder: Toward an integrated examination of disorder maintenance and functional impairment. Clin. Psychol. Rev. 2013, 33, 33–44. [Google Scholar] [CrossRef]
- Herrell, R.K.; Edens, E.N.; Riviere, L.A.; Thomas, J.L.; Bliese, P.D.; Hoge, C.W. Assessing functional impairment in a working military population: The Walter Reed Functional Impairment Scale. Psychol. Serv. 2014, 11, 254. [Google Scholar] [CrossRef] [PubMed]
- Barger, L.K.; Ayas, N.T.; Cade, B.E.; Cronin, J.W.; Rosner, B.; Speizer, F.E.; Czeisler, C.A. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med. 2006, 3, e487. [Google Scholar] [CrossRef] [PubMed]
- Swanson, L.M.; Arnedt, J.T.; Rosekind, M.R.; Belenky, G.; Balkin, T.J.; Drake, C. Sleep disorders and work performance: Findings from the 2008 National Sleep Foundation Sleep in America poll. J. Sleep Res. 2011, 20, 487–494. [Google Scholar] [CrossRef]
- Cammann, C.; Fichman, M.; Jenkins, D.; Klesh, J. The Michigan Organizational Assessment Questionnaire; Unpublshed Manuscript; University of Michigan: Ann Arbor, MI, USA, 1979. [Google Scholar]
- Jones, E.; Chonko, L.; Rangarajan, D.; Roberts, J. The role of overload on job attitudes, turnover intentions, and salesperson performance. J. Bus. Res. 2007, 60, 663–671. [Google Scholar] [CrossRef]
- Kim, H.; Stoner, M. Burnout and turnover intention among social workers: Effects of role stress, job autonomy and social support. Adm. Soc. Work 2008, 32, 5–25. [Google Scholar] [CrossRef]
- Pearson, Q.M. Role overload, job satisfaction, leisure satisfaction, and psychological health among employed women. J. Couns. Dev. 2008, 86, 57–63. [Google Scholar] [CrossRef]
- Shultz, K.S.; Wang, M.; Olson, D.A. Role overload and underload in relation to occupational stress and health. Stress Health J. Int. Soc. Investig. Stress 2010, 26, 99–111. [Google Scholar] [CrossRef]
- Williams, C. Work-Life Balance of Shift Workers; Statistics Canada: Ottawa, ON, Canada, 2008. [Google Scholar]
- Jones III, A.; Norman, C.S.; Wier, B. Healthy lifestyle as a coping mechanism for role stress in public accounting. Behav. Res. Account. 2010, 22, 21–41. [Google Scholar] [CrossRef]
- Zare, R.; Choobineh, A.; Keshavarzi, S. Association of amplitude and stability of circadian rhythm, sleep quality, and occupational stress with sickness absence among a gas company employees—A cross sectional study from Iran. Saf. Health Work 2017, 8, 276–281. [Google Scholar] [CrossRef]
- Lu, J.L. Organizational role stress indices affecting burnout among nurses. J. Int. Womens Stud. 2008, 9, 63–78. [Google Scholar]
- Ng, S.I.; Sambasivan, M.; Zubaidah, S. Antecedents and outcomes of flight attendants’ job satisfaction. J. Air Transp. Manag. 2011, 17, 309–313. [Google Scholar] [CrossRef]
- Johns, M. Rethinking the assessment of sleepiness. Sleep Med. Rev. 1998, 2, 3–15. [Google Scholar] [CrossRef]
- Vennelle, M.; Engleman, H.M.; Douglas, N.J. Sleepiness and sleep-related accidents in commercial bus drivers. Sleep Breath. 2010, 14, 39–42. [Google Scholar] [CrossRef] [PubMed]
- McCartt, A.T.; Rohrbaugh, J.W.; Hammer, M.C.; Fuller, S.Z. Factors associated with falling asleep at the wheel among long-distance truck drivers. Accid. Anal. Prev. 2000, 32, 493–504. [Google Scholar] [CrossRef]
- Melamed, S.; Ugarten, U.; Shirom, A.; Kahana, L.; Lerman, Y.; Froom, P. Chronic burnout, somatic arousal and elevated salivary cortisol levels. J. Psychosom. Res. 1999, 46, 591–598. [Google Scholar] [CrossRef]
- Rupp, T.L.; Wesensten, N.J.; Bliese, P.D.; Balkin, T.J. Banking sleep: Realization of benefits during subsequent sleep restriction and recovery. Sleep 2009, 32, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Patterson, P.D.; Ghen, J.D.; Antoon, S.F.; Martin-Gill, C.; Guyette, F.X.; Weiss, P.M.; Turner, R.L.; Buysse, D.J. Does evidence support “banking/extending sleep” by shift workers to mitigate fatigue, and/or to improve health, safety, or performance? A systematic review. Sleep Health 2019. [Google Scholar] [CrossRef] [PubMed]
- Mantua, J.; Skeiky, L.; Prindle, N.; Trach, S.; Doty, T.J.; Balkin, T.J.; Brager, A.J.; Capaldi, V.F.; Simonelli, G. Sleep extension reduces fatigue in healthy, normally-sleeping young adults. Sleep Sci. 2019, 12, 21. [Google Scholar] [CrossRef] [PubMed]
- Ritland, B.M.; Simonelli, G.; Gentili, R.J.; Smith, J.C.; He, X.; Mantua, J.; Balkin, T.J.; Hatfield, B.D. Effects of sleep extension on cognitive/motor performance and motivation in military tactical athletes. Sleep Med. 2019, 58, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Simonelli, G.; Mantua, J.; Gad, M.; St Pierre, M.; Moore, L.; Yarnell, A.M.; Quartana, P.J.; Braun, A.; Balkin, T.J.; Brager, A.J. Sleep extension reduces pain sensitivity. Sleep Med. 2019, 54, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Reifman, J.; Ramakrishnan, S.; Liu, J.; Kapela, A.; Doty, T.J.; Balkin, T.J.; Kumar, K.; Khitrov, M.Y. 2B-Alert App: A mobile application for real-time individualized prediction of alertness. J. Sleep Res. 2018, e12725. [Google Scholar] [CrossRef]
- Matsangas, P.; Mysliwiec, V. The utility of the Pittsburgh Sleep Quality Index in US military personnel. Mil. Psychol. 2018, 30, 360–369. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Shattuck, N.L.; Matsangas, P. Psychomotor vigilance performance predicted by Epworth Sleepiness Scale scores in an operational setting with the United States N avy. J. Sleep Res. 2015, 24, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Sauter, C.; Kowalski, J.T.; Stein, M.; Roettger, S.; Danker-Hopfe, H. Effects of a Workplace-Based Sleep Health Program on Sleep in Members of the German Armed Forces. J. Clin. Sleep Med. 2019, 15, 417–429. [Google Scholar] [CrossRef]
- Vernalis, M. Army Reserve Component Personal Empowerment Program# 2 (ARCPEP 2); The Henry M. Jackson Foundation for the Advancement of Military Medicine: Bethesda, MD, USA, 2015. [Google Scholar]
- Rice, V.J.; Schroeder, P.J. Self-reported sleep, anxiety, and cognitive performance in a sample of US Military active duty and veterans. Mil. Med. 2019, 184, 488–497. [Google Scholar] [CrossRef] [PubMed]
- Luxton, D.D.; Greenburg, D.; Ryan, J.; Niven, A.; Wheeler, G.; Mysliwiec, V. Prevalence and Impact of Short Sleep Duration in Redeployed OIF Soldiers. Sleep 2011, 34, 1189–1195. [Google Scholar] [CrossRef]
- Adler, A.B.; Gunia, B.C.; Bliese, P.D.; Kim, P.Y.; LoPresti, M.L. Using actigraphy feedback to improve sleep in soldiers: An exploratory trial. Sleep Health 2017, 3, 126–131. [Google Scholar] [CrossRef]
- Mantua, J.; Bessey, A.F.; Ritland, B.M.; Naylor, J.A.; Chabuz, R.; McKeon, A.B.; Capaldi, V.F.; Sowden, W.J. Sleep loss is related to unstable stationary balance in US Army Soldiers in an operationally-relevant context. Sleep Med. 2020, in press. [Google Scholar] [CrossRef]
- Mondal, P.; Gjevre, J.A.; Taylor-Gjevre, R.M.; Lim, H.J. Relationship between the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in a sleep laboratory referral population. Nat. Sci. Sleep 2013, 5, 15. [Google Scholar]
- Bonnet, M.H. Performance and sleepiness as a function of frequency and placement of sleep disruption. Psychophysiology 1986, 23, 263–271. [Google Scholar] [CrossRef]
- Danker-Hopfe, H.; Sauter, C.; Kowalski, J.T.; Kropp, S.; Ströhle, A.; Wesemann, U.; Zimmermann, P.L. Sleep quality of German soldiers before, during and after deployment in Afghanistan—A prospective study. J. Sleep Res. 2017, 26, 353–363. [Google Scholar] [CrossRef]
- Shattuck, N.L.; Matsangas, P.; Saitzyk, A. Improving Work and Rest Patterns of Military Personnel in Operational Settings with Frequent Unplanned Events. In Proceedings of the Proceedings of the Human Factors and Ergonomics Society Annual Meeting; SAGE Publications Sage CA: Los Angeles, CA, 2018; Volume 62, pp. 772–776. [Google Scholar]
- Mantua, J.; Bessey, A.; Sowden, W.J.; Chabuz, R.; Brager, A.J.; Capaldi, V.F.; Simonelli, G. A review of environmental barriers to obtaining adequate sleep in the military operational context. Mil. Med. 2019. [Google Scholar] [CrossRef] [PubMed]
- Arnal, P.J.; Sauvet, F.; Leger, D.; van Beers, P.; Bayon, V.; Bougard, C.; Rabat, A.; Millet, G.Y.; Chennaoui, M. Benefits of Sleep Extension on Sustained Attention and Sleep Pressure Before and During Total Sleep Deprivation and Recovery. Sleep 2015, 38, 1935–1943. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.; Cohen, P.; West, S.G.; Aiken, L.S. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences, 3rd ed.; Riegert, D., Ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2013. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2013; ISBN 1-134-74270-3. [Google Scholar]
- Stordeur, S.; D’hoore, W.; Vandenberghe, C. Leadership, organizational stress, and emotional exhaustion among hospital nursing staff. J. Adv. Nurs. 2001, 35, 533–542. [Google Scholar] [CrossRef]
- Seery, B.L.; Corrigall, E.A. Emotional labor: Links to work attitudes and emotional exhaustion. J. Manag. Psychol. 2009, 24, 797–813. [Google Scholar] [CrossRef]
- Ekstedt, M.; Söderström, M.; Akerstedt, T.; Nilsson, J.; Søndergaard, H.-P.; Aleksander, P. Disturbed sleep and fatigue in occupational burnout. Scand. J. Work. Environ. Health 2006, 32, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Johns, M.W. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep 1992, 15, 376–381. [Google Scholar] [CrossRef] [PubMed]
| Component | Predictor | Outcome | B | Lower CI | Upper CI | R2 | p | f2 |
|---|---|---|---|---|---|---|---|---|
| -- | Global Score | EE | 0.49 | −0.99 | 1.98 | 0.09 | 0.06 | 0.10 |
| FI | 0.26 | −0.34 | 0.87 | 0.05 | 0.38 | 0.05 | ||
| RO | 0.25 | −0.19 | 0.68 | 0.18 | 0.13 | 0.22 | ||
| DS | 0.86 | 0.33 | 1.39 | 0.36 | 0.017 | 0.56 | ||
| 1 | Overall Sleep Quality | EE | 2.75 | −3.51 | 8.99 | 0.10 | 0.21 | 0.11 |
| FI | 0.55 | −1.98 | 3.01 | 0.02 | 0.79 | 0.02 | ||
| RO | −0.61 | −2.75 | 1.53 | 0.04 | 0.57 | 0.04 | ||
| DS | 3.36 | 0.84 | 5.87 | 0.26 | 0.026 | 0.35 | ||
| 2 | Sleep Latency | EE | −2.33 | −5.42 | 0.74 | 0.14 | 0.22 | 0.16 |
| FI | 0.06 | −1.23 | 1.35 | 0.01 | 0.43 | 0.01 | ||
| RO | −0.10 | −1.21 | 1.00 | 0.03 | 0.81 | 0.03 | ||
| DS | 0.63 | −0.90 | 2.17 | 0.06 | 0.64 | 0.06 | ||
| 3 | Sleep Duration | EE | 1.20 | −2.38 | 4.80 | 0.08 | 0.18 | 0.09 |
| FI | 0.60 | −0.84 | 2.03 | 0.04 | 0.92 | 0.04 | ||
| RO | 0.65 | −0.57 | 1.87 | 0.06 | 0.27 | 0.06 | ||
| DS | 1.84 | 0.38 | 3.30 | 0.23 | 0.031 | 0.30 | ||
| 4 | Sleep Efficiency | EE | −3.12 | −7.66 | 1.42 | 0.14 | 0.49 | 0.16 |
| FI | 0.83 | −0.90 | 2.55 | 0.08 | 0.50 | 0.09 | ||
| RO | 0.33 | −1.10 | 1.75 | 0.12 | 0.47 | 0.18 | ||
| DS | 2.17 | 0.36 | 3.98 | 0.23 | 0.004 | 0.30 | ||
| 5 | Sleep Disturbance | EE | 4.48 | −2.20 | 11.17 | 0.12 | 0.25 | 0.18 |
| FI | −0.26 | −3.03 | 2.51 | 0.01 | 0.85 | 0.02 | ||
| RO | −0.01 | −2.40 | 2.39 | 0.03 | 0.72 | 0.03 | ||
| DS | −0.03 | −3.19 | 2.12 | 0.03 | 0.47 | 0.03 | ||
| 6 | Sleep Medication | EE | 3.58 | −2.39 | 9.53 | 0.11 | 0.27 | 0.12 |
| FI | 2.08 | −0.24 | 4.40 | 0.12 | 0.20 | 0.14 | ||
| RO | 0.26 | −1.89 | 2.42 | 0.03 | 0.80 | 0.03 | ||
| DS | −0.96 | −3.80 | 1.86 | 0.05 | 0.43 | 0.05 | ||
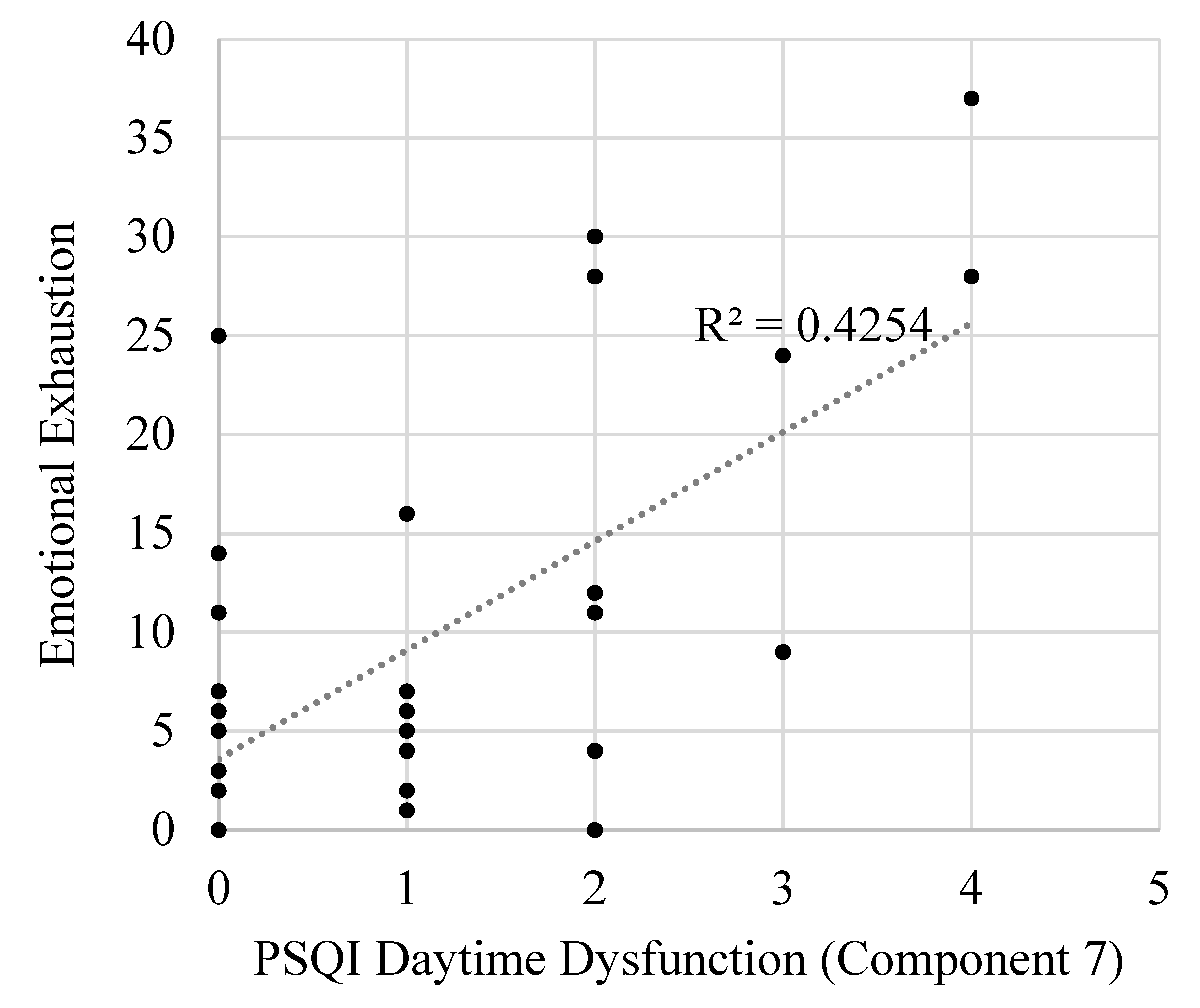
| 7 | Daytime Dysfunction | EE | 3.43 | 1.71 | 5.16 | 0.41 | <0.001 | 0.70 |
| FI | 1.54 | 0.13 | 2.95 | 0.16 | 0.003 | 0.19 | ||
| RO | 1.50 | 0.32 | 2.67 | 0.22 | 0.019 | 0.28 | ||
| DS | 0.22 | −0.77 | 1.22 | 0.04 | 0.79 | 0.04 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mantua, J.; Bessey, A.F.; Sowden, W.J. Poor Subjective Sleep Quality Is Associated with Poor Occupational Outcomes in Elite Soldiers. Clocks & Sleep 2020, 2, 182-193. https://doi.org/10.3390/clockssleep2020015
Mantua J, Bessey AF, Sowden WJ. Poor Subjective Sleep Quality Is Associated with Poor Occupational Outcomes in Elite Soldiers. Clocks & Sleep. 2020; 2(2):182-193. https://doi.org/10.3390/clockssleep2020015
Chicago/Turabian StyleMantua, Janna, Alexxa F. Bessey, and Walter J. Sowden. 2020. "Poor Subjective Sleep Quality Is Associated with Poor Occupational Outcomes in Elite Soldiers" Clocks & Sleep 2, no. 2: 182-193. https://doi.org/10.3390/clockssleep2020015
APA StyleMantua, J., Bessey, A. F., & Sowden, W. J. (2020). Poor Subjective Sleep Quality Is Associated with Poor Occupational Outcomes in Elite Soldiers. Clocks & Sleep, 2(2), 182-193. https://doi.org/10.3390/clockssleep2020015





