Perceptions Regarding Daith Piercing in Migraine, A Survey of Pediatric Patients
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Descriptive Statistics
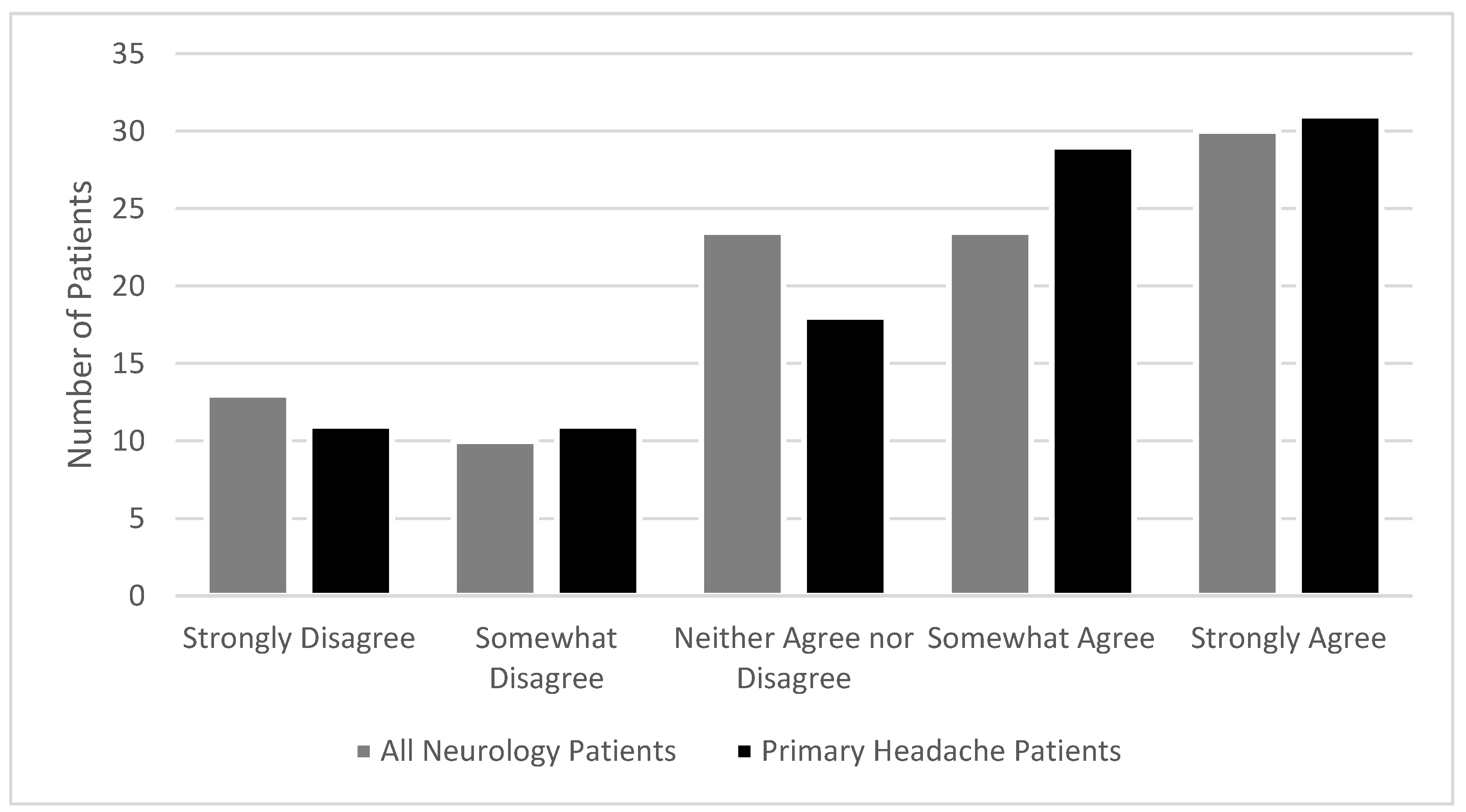
3.2. Knowledge of and Willingness to Try Daith Piercing
3.3. Experiences of Participants Having Undergone Daith Piercings
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Vos, T.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.; Abd-Allah, F.; Abdulkader, R.S.; Abdulle, A.M.; Abebo, T.A.; Abera, S.F.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef]
- Kabbouche, M.A.; Powers, S.W.; Vockell, A.-L.B.; LeCates, S.L.; Ellinor, P.L.; Segers, A.; Manning, P.; Burdine, D.; Hershey, A.D. Outcome of a Multidisciplinary Approach to Pediatric Migraine at 1, 2, and 5 years. Headache 2005, 45, 1298–1303. [Google Scholar] [CrossRef] [PubMed]
- Powers, S.W.; Patton, S.R.; Hommel, K.A.; Hershey, A.D. Quality of life in childhood migraines: Clinical impact and comparison to other chronic illnesses. Pediatrics 2003, 112, e1–e5. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, M.H.; Esper, G.J.; Bashir, F.F. When to Consider Prophylactic Antimigraine Therapy in Children with Migraine. Curr. Treat. Options Neurol. 2019, 21, 15. [Google Scholar] [CrossRef] [PubMed]
- Kacperski, J.; Kabbouche, M.A.; O’Brien, H.L.; Weberding, J.L. The optimal management of headaches in children and adolescents. Ther. Adv. Neurol. Disord. 2016, 9, 53–68. [Google Scholar] [CrossRef] [PubMed]
- Hepp, Z.; Dodick, D.W.; Varon, S.F.; Gillard, P.; Hansen, R.N.; Devine, E.B. Adherence to oral migraine-preventive medications among patients with chronic migraine. Cephalalgia 2015, 35, 478–488. [Google Scholar] [CrossRef]
- Bachur, R.; Monuteaux, M.C.; Neuman, M.I. A Comparison of Acute Treatment Regimens for Migraine in the Emergency Department. Pediatrics 2015, 135, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Richer, L.; Graham, L.; Klassen, T.; Rowe, B. Emergency Department Management of Acute Migraine in Children in Canada: A Practice Variation Study. Headache 2007, 47, 703–710. [Google Scholar] [CrossRef]
- Klim, S.; Krieser, D.; Kelly, A. Sub-optimal treatment of paediatric migraine in an emergency department: An observational study. Emerg. Med. Australas. 2019, 31, 879–881. [Google Scholar] [CrossRef]
- Groenewald, C.B.; Beals-Erickson, S.E.; Ralston-Wilson, J.; Rabbitts, J.A.; Palermo, T.M. Complementary and Alternative Medicine Use by Children With Pain in the United States. Acad. Pediatr. 2017, 17, 785–793. [Google Scholar] [CrossRef]
- Vinson, R.; Yeh, G.; Davis, R.B.; Logan, D. Correlates of Complementary and Alternative Medicine Use in a Pediatric Tertiary Pain Center. Acad. Pediatr. 2014, 14, 491–496. [Google Scholar] [CrossRef]
- Tsao, J.C.I.; Meldrum, M.; Kim, S.C.; Jacob, M.C.; Zeltzer, L.K. Treatment Preferences for CAM in Children with Chronic Pain. Evidence-Based Complement. Altern. Med. 2007, 4, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Daith Piercing for Migraines: Does It Work and Is It Safe? Available online: https://www.healthline.com/health/migraine/daith-piercing-for-migraines (accessed on 28 July 2020).
- Can Daith Piercing Stop Migraines? Here’s What You Need to Know about the Ear Piercing Trend HuffPost UK Life. Available online: https://www.huffingtonpost.co.uk/2016/01/07/daith-piercing-migraine-relief_n_8531022.html?ec_carp=3403506313360899636&guccounter=1&guce_referrer=aHR0cHM6Ly9kdWNrZHVja2dvLmNvbS8&guce_referrer_sig=AQAAAEhHicnxfP6S3QD6bysPRw_ikAP2oo9b1z27J7vB4xUbF4iBdxvi170l6wRMJUoW1QUIGCSq_7FQ7TVpnli6f8fC749ABiPPI9AJdSBcIj5HSYdQGt0o0X3Hr9SdPzcGHMqvrvcPq8P33Drka3auR9twGJOzSsyoFq1ShPDJaY9r (accessed on 23 July 2020).
- Rizzo, A.C.; Paolucci, M.; Altavilla, R.; Brunelli, N.; Assenza, F.; Altamura, C.; Vernieri, F. Daith Piercing in a Case of Chronic Migraine: A Possible Vagal Modulation. Front. Neurol. 2017, 8. [Google Scholar] [CrossRef]
- Bhandari, P.; Ranjit, E.; Sapra, A.; Davis, D.; Brenham, C. Daith Piercing: Wonder Treatment or Untested Fad? Cureus 2020, 12, e6978. [Google Scholar] [CrossRef] [PubMed]
- Bethell, C.; Kemper, K.J.; Gombojav, N.; Koch, T.K. Complementary and Conventional Medicine Use Among Youth With Recurrent Headaches. Pediatrics 2013, 132, e1173–e1183. [Google Scholar] [CrossRef]
- Zhang, Y.; Dennis, J.A.; Leach, M.J.; Bishop, F.L.; Cramer, H.; Chung, V.C.H.; Moore, C.; Lauche, R.; Cook, R.; Sibbritt, D.; et al. Complementary and Alternative Medicine Use Among US Adults With Headache or Migraine: Results from the 2012 National Health Interview Survey. Headache 2017, 57, 1228–1242. [Google Scholar] [CrossRef] [PubMed]
- Blatchley, C.; Wilkins, A. International Surveys of the Effects of Daith Piercing on Migraines-a Report Ear Piercing for Migraines: Three Medical Surveys Examining the Effects of Daith Piercing on Migraines Preliminary Report with Detailed Analysis of the Initial Survey of 1262 Patients. 2017. Available online: www.migraine-research.org (accessed on 23 July 2020).
- Daith Piercing Evidence for Migraine from 1107 Respondents-MigrainePal. Available online: https://migrainepal.com/daith-piercing-evidence-for-migraine/ (accessed on 23 July 2020).
- WHO. The WHO-W Standard Acupuncture Point Locations in, 2008 Undefined. WHO Standard Acupuncture Point Locations in the Western Pacific Region; WHO: Switzerland, Geneva, 2008. [Google Scholar]
- Allais, G.; Romoli, M.; Rolando, S.; Airola, G.; Gabellari, I.C.; Allais, R.; Benedetto, C. Ear acupuncture in the treatment of migraine attacks: A randomized trial on the efficacy of appropriate versus inappropriate acupoints. Neurol. Sci. 2011, 32, 173–175. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhang, X.; Guo, J.; Liu, H.; Zhang, Y.; Liu, C.-Z.; Yi, J.-H.; Wang, L.-P.; Zhao, J.-P.; Li, S.-S. Efficacy of Acupuncture for Acute Migraine Attack: A Multicenter Single Blinded, Randomized Controlled Trial. Pain Med. 2012, 13, 623–630. [Google Scholar] [CrossRef]
- Murakami, M.; Fox, L.; Dijkers, M.P. Ear Acupuncture for Immediate Pain Relief—A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Pain Med. 2017. [Google Scholar] [CrossRef]
- Li, Y.; Liang, F.; Yang, X.; Tian, X.; Yan, J.; Sun, G.; Chang, X.; Tang, Y.; Ma, T.; Zhou, L.; et al. Acupuncture for Treating Acute Attacks of Migraine: A Randomized Controlled Trial. Headache 2009, 49, 805–816. [Google Scholar] [CrossRef]
- Graff, D.M.; McDonald, M.J. Auricular Acupuncture for the Treatment of Pediatric Migraines in the Emergency Department. Pediatr. Emerg. Care 2018, 34, 258–262. [Google Scholar] [CrossRef] [PubMed]
- Soliman, N.; Frank, B.L. Auricular acupuncture and auricular medicine. Phys. Med. Rehabilitation Clin. North Am. 1999, 10, 544–554. [Google Scholar]
- Romoli, M.; Allais, G.; Airola, G.; Benedetto, C.; Mana, O.; Giacobbe, M.; Pugliese, A.M.; Battistella, G.; Fornari, E. Ear acupuncture and fMRI: A pilot study for assessing the specificity of auricular points. Neurol. Sci. 2014, 35, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Dhond, R.P.; Yeh, C.; Park, K.; Kettner, N.; Napadow, V. Acupuncture modulates resting state connectivity in default and sensorimotor brain networks. Pain 2008, 136, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Tassorelli, C.; Grazzi, L.; De Tommaso, M.; Pierangeli, G.; Martelletti, P.; Rainero, I.; Dorlas, S.; Geppetti, P.; Ambrosini, A.; Sarchielli, P.; et al. Noninvasive vagus nerve stimulation as acute therapy for migraine. Neurology 2018, 91, e364–e373. [Google Scholar] [CrossRef]
- Mitsikostas, D.D.; Rapoport, A.M. Chronic migraine prevention with non-invasive vagus nerve stimulation in a prospective pilot study (the event study): Report from the open-label phase. Headache 2014, 13, 279. [Google Scholar]
- Lipman, J.J.; Miller, B.E.; Mays, K.S.; Miller, M.N.; North, W.C.; Byrne, W.L. Peak B endorphin concentration in cerebrospinal fluid: Reduced in chronic pain patients and increased during the placebo response. Psychopharmacology 1990, 102, 112–116. [Google Scholar] [CrossRef]
- Benedetti, F.; Pollo, A.; Lopiano, L.; Lanotte, M.; Vighetti, S.; Rainero, I. Conscious Expectation and Unconscious Conditioning in Analgesic, Motor, and Hormonal Placebo/Nocebo Responses. J. Neurosci. 2003, 23, 4315–4323. [Google Scholar] [CrossRef]

| Variables | Primary Headache Patients (n = 119) | Non-Headache Patients (n = 51) | Total Patients (n = 170) | Missing |
|---|---|---|---|---|
| Age (Median, Standard Deviation) | 14 (3.14) | 12 (6.67) | 14 (4.18) | 43 (25%) |
| Female/Male | 74 (62%)/34 (29%) | 33 (65%)/13 (26%) | 108 (63%)/47 (27.5%) | 16 (9.4%) |
| Caucasian race | 90 (75.6) | 39 (77%) | 130 (76%) | 18 (10.5%) |
| Hispanic or Latino ethnicity | 3 (2.5% | 3 (5.9%) | 6 (3.5%) | 28 (16.4%) |
| Internet access at home | 102 (86%) | 41 (80%) | 144 (84%) | 17 (9.9%) |
| Cell phone owners | 101 (85%) | 40 (78%) | 142 (83%) | 17 (10%) |
| Highest level of education (Father) | ||||
| Some high school | 10 (8.4%) | 6 (12%) | 16 (9.4%) | 24 (14%) |
| High school | 21 (17.6%) | 7 (14%) | 28 (16.4%) | - |
| Some college/technical school | 39 (32.8%) | 13 (26%) | 53 (31%) | - |
| College degree | 23 (19.8%) | 11 (22%) | 34 (19.9%) | - |
| Post college degree | 9 (7.6%) | 7 (14%) | 16 (9.4%) | - |
| Highest level of education (Mother) | ||||
| Some high school | 3 (2.5%) | 3 (6%) | 6 (3.5%) | 18 (10.5%) |
| High school | 19 (16%) | 4 (8%) | 23 (13.5%) | - |
| Some college/technical school | 28 (23.5%) | 18 (35%) | 46 (26.9%) | - |
| College degree | 45 (37.8%) | 14 (28%) | 59 (34.5%) | - |
| Post college degree | 12 (10.1%) | 7 (14%) | 19 (11.1%) | - |
| Median household income (category) | $70,000–$79,999 | $50,000–59,999 | 8 (16%) |
| Variables | Prior Knowledge of Daith | Personal Contact with Someone with Daith | Has Had A Daith | Willing to Try Daith |
|---|---|---|---|---|
| Chi Square Analyses | ||||
| Female sex | 5.96 (0.015) | 3.52 (0.061) | 2.52 (0.284) | 7.0 (0.008) |
| Caucasian race | 2.23 (0.693) | 7.08 (0.069) | 0.47 (0.925) | 7.32 (0.676) |
| Owning a cell phone | 2.054 (0.152) | 0.019 (0.890) | 0.508 (0.776) | 17.46 (0.002) |
| Internet access | 0.005 (0.944) | 0.847 (0.357) | 0.586 (0.746) | 4.402 (0.354) |
| Correlations (Point-Biserial) | ||||
| Age | 0.124 (0.165) | 0.125 (0.247) | 0.114 (0.286) | 0.245 (0.007) |
| Highest level of education of the father | 0.017 (0.840) | −0.03 (0.972) | −0.068 (0.491) | −0.065 (0.45) |
| Highest level of education of the mother | −0.028 (0.734) | −0.134 (0.168) | −0.066 (0.495) | −0.14 (0.093) |
| Family’s annual household income | −0.081 (0.332) | −0.176 (0.074) | −0.072 (0.465) | −0.199 (0.019) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gerson, T.; Connelly, M.; Boorigie, M.; Bickel, J.; Dilts, J. Perceptions Regarding Daith Piercing in Migraine, A Survey of Pediatric Patients. J 2020, 3, 289-298. https://doi.org/10.3390/j3030022
Gerson T, Connelly M, Boorigie M, Bickel J, Dilts J. Perceptions Regarding Daith Piercing in Migraine, A Survey of Pediatric Patients. J. 2020; 3(3):289-298. https://doi.org/10.3390/j3030022
Chicago/Turabian StyleGerson, Trevor, Mark Connelly, Madeline Boorigie, Jennifer Bickel, and Jennifer Dilts. 2020. "Perceptions Regarding Daith Piercing in Migraine, A Survey of Pediatric Patients" J 3, no. 3: 289-298. https://doi.org/10.3390/j3030022
APA StyleGerson, T., Connelly, M., Boorigie, M., Bickel, J., & Dilts, J. (2020). Perceptions Regarding Daith Piercing in Migraine, A Survey of Pediatric Patients. J, 3(3), 289-298. https://doi.org/10.3390/j3030022






