Rural and Urban Population Differences in the Association of Dietary Calcium with Blood Pressure and Hypertension Occurrence: Analysis of Longitudinal Data from the China Health and Nutrition Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Outcome Variables
2.2.1. Hypertension Occurrence
2.2.2. Blood Pressure
2.3. DCI
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Variable Characteristics
3.2. Hypertension Prevalence and DCI in Both the RP and the UP
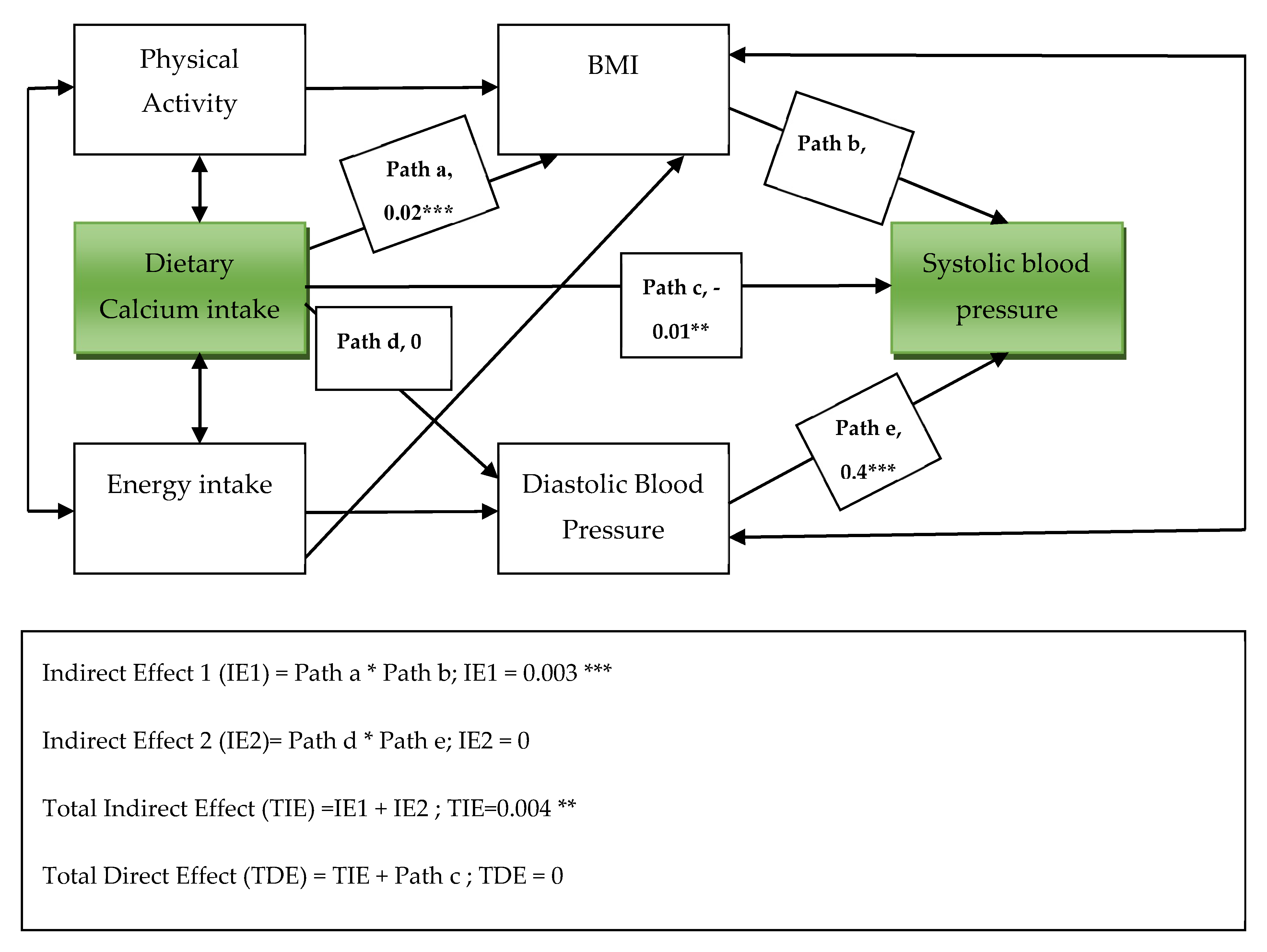
3.3. Association between DCI and Blood Pressure in the General Population
3.4. Association between DCI and HTN
3.4.1. Association between DCI and HTN among the RP and the UP
3.4.2. Dietary Calcium Intake and HTN in the Populations by Sex
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- O’Connell, S. Assessing and managing primary hypertension. Nurs. Times 2014, 110, 1–14. [Google Scholar]
- Castro, I.; Waclawovsky, G.; Marcadenti, A. Nutrition and physical activity on hypertension: Implication of current evidence and guidelines. Curr. Hypertens. Rev. 2015, 11, 91–99. [Google Scholar] [CrossRef]
- Osman, S.; Costanian, C.; Annan, N.B.; Fouad, F.M.; Jaffa, M.; Sibai, A.M. Urbanization and Socioeconomic Disparities in Hypertension among Older Adult Women in Sudan. Ann. Glob. Health 2019, 85, 29. [Google Scholar] [CrossRef] [PubMed]
- Bâ, H.O.; Camara, Y.; Menta, I.; Sangaré, I.; Sidibé, N.; Diall, I.B.; Coulibaly, S.; Kéita, M.A.; Millogo, G.R.C. Hypertension and Associated Factors in Rural and Urban Areas Mali: Data from the STEP 2013 Survey. Int. J. Hypertens. 2018, 2018, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Mills, K.T.; Bundy, J.D.; Kelly, T.N.; Reed, J.E.; Kearney, P.M.; Reynolds, K.; Chen, J.; He, J. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation 2016, 134, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Egan, K.B.; Suh, M.; Rosen, R.C.; Burnett, A.L.; Ni, X.; Wong, D.G.; McVary, K.T. Rural vs. urban disparities in association with lower urinary tract symptoms and benign prostatic hyperplasia in ageing men, NHANES 2001–2008. Int. J. Clin. Pract. 2015, 69, 1316–1325. [Google Scholar] [CrossRef]
- Chow, C.K.; Teo, K.K.; Rangarajan, S.; Islam, S.; Gupta, R.; Avezum, A.; Bahonar, A.; Chifamba, J.; Dagenais, G.; Diaz, R.; et al. Prevalence, Awareness, Treatment, and Control of Hypertension in Rural and Urban Communities in High-, Middle-, and Low-Income Countries. JAMA 2013, 310, 959–968. [Google Scholar] [CrossRef]
- Downey, L.H. Rural Populations and Health: Determinants, Disparities, and Solutions. Prev. Chronic Dis. 2013, 10. [Google Scholar] [CrossRef][Green Version]
- Darmawan, J.; Valkenburg, H.A.; Muirden, K.D.; Wigley, R.D. Epidemiology of rheumatic diseases in rural and urban populations in Indonesia: A World Health Organisation International League against Rheumatism COPCORD study, stage I, phase 2. Ann. Rheum. Dis. 1992, 51, 525–528. [Google Scholar] [CrossRef]
- Omidvar, N.; Tirang, R.N.; Hajifaraji, M.; Eshraghian, M.-R.; Rezazadeh, A.; Armin, S.; Haidari, H.; Zowghi, T.; Neyestani, T.R. Calcium Intake, Major Dietary Sources and Bone Health Indicators in Iranian Primary School Children. Iran. J. Pediatr. 2015, 25, e177. [Google Scholar] [CrossRef]
- Center, National Institutes of Health Osteoporosis and Related Bone Diseases National Resource. Calcium and Vitamin D: Importance at Every Age. National Institutes of Health Webpage. Available online: https://www.bones.nih.gov/sites/bones/files/pdfs/cal-vit-d-important-any-age-508.pdf. (accessed on 6 December 2019).
- Daily News for Senior Citizens. Senior Journal. Senior Citizens at High Risk of Bone Fractures May Find Safety Taking Vitamin D with Calcium. Available online: http://www.seniorjournal.com/NEWS/Health/2014/20140604 (accessed on 3 October 2019).
- Corleone, J. Live Well. Percentage of Daily Values Based on a 2000 Calorie Diet. Available online: https://livewell.jillianmichaels.com/percentage-daily-values-based-2000-calorie-diet-5401.html (accessed on 4 October 2019).
- Schrager, S. Dietary Calcium Intake and Obesity. J. Am. Board Fam. Pract. 2005, 18, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Wang, X.-F.; Li, D.-Y.; Chen, Y.-C.; Zhao, L.-J.; Liu, X.-G.; Guo, Y.-F.; Shen, J.; Lin, X.; Deng, J.; et al. The good, the bad, and the ugly of calcium supplementation: A review of calcium intake on human health. Clin. Interv. Aging 2018, 13, 2443–2452. [Google Scholar] [CrossRef] [PubMed]
- Mayo Clinic Staff. Nutrition and Healthy Eating. Mayoclinic. Available online: https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/calcium-supplements/art-20047097 (accessed on 12 December 2019).
- Behuliak, M.; Bencze, M.; Vaneckova, I.; Kunes, J.; Zicha, J. Basal and Activated Calcium Sensitization Mediated by RhoA/Rho Kinase Pathway in Rats with Genetic and Salt Hypertension. BioMed Res. Int. 2017, 2017, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Pörsti, I.; Mäkynen, H. Dietary calcium intake: Effects on central blood pressure control. Semin. Nephrol. 1995, 15, 550–563. [Google Scholar]
- Dickinson, H.O.; Nicolson, N.; Cook, J.V.; Campbell, F.; Beyer, F.R.; Ford, G.A.; Mason, J.M. Calcium supplementation for the management of primary hypertension in adults. Cochrane Database Syst. Rev. 2006, 2, CD004639. [Google Scholar] [CrossRef]
- Magalhães, E.I.D.S.; Pessoa, M.C.; Franceschini, S.D.C.C.; De Novaes, J.F. Dietary calcium intake is inversely associated with blood pressure in Brazilian children. Int. J. Food Sci. Nutr. 2016, 68, 1–8. [Google Scholar] [CrossRef]
- Bostick, R.M.; Kushi, L.H.; Wu, Y.; Meyer, K.A.; Sellers, T.A.; Folsom, A.R. Relation of calcium, vitamin D, and dairy food intake to ischemic heart disease mortality among postmenopausal women. Am. J. Epidemiology 1999, 149, 151–161. [Google Scholar] [CrossRef]
- Liu, Z.; Fang, A.; He, J.; Shen, X.; Gao, R.; Zhao, X.; Li, K. Association of Habitually Low Intake of Dietary Calcium with Blood Pressure and Hypertension in a Population with Predominantly Plant-Based Diets. Nutr. 2018, 10, 603. [Google Scholar] [CrossRef]
- Wang, L.; Manson, J.E.; Buring, J.E.; Lee, I.-M.; Sesso, H.D. Dietary Intake of Dairy Products, Calcium, and Vitamin D and the Risk of Hypertension in Middle-Aged and Older Women. Hypertension 2008, 51, 1073–1079. [Google Scholar] [CrossRef]
- Daily, J.W.; Kim, B.C.; Liu, M.; Park, S. People with the major alleles of ATP2B1 rs17249754 increases the risk of hypertension in high ratio of sodium and potassium, and low calcium intakes. J. Hum. Hypertens. 2017, 31, 787–794. [Google Scholar] [CrossRef]
- Sygit, K.M.; Sygit, M.; Wojtyła, C.; Lubiniec, O.; Stelmach, W.; Krakowiak, J. Physical activity as an important element in organizing and managing the lifestyle of populations in urban and rural environments. Ann. Agric. Environ. Med. 2018, 26, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Harinarayan, C.V.; Ramalakshmi, T.; Prasad, U.V.; Sudhakar, D.; Srinivasarao, P.V.; Sarma, K.V.; Kumar, E.G. High prevalence of low dietary calcium, high phytate consumption, and vitamin D deficiency in healthy south Indians. Am. J. Clin. Nutr. 2007, 85, 1062–1067. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Li, W.; Yin, L.; Jian, B.; Peng, Y.G.; Wang, Y. Comparison of healthy lifestyle behaviors among individuals with and without cardiovascular diseases from urban and rural areas in China: A cross-sectional study. PLoS ONE 2017, 12, e0181981. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Zhai, F.Y.; Du, S.F.; Popkin, B.M. The China Health and Nutrition Survey, 1989-2011. Obes. Rev. 2014, 15, 2–7. [Google Scholar] [CrossRef]
- Fang, A.; Li, K.; Li, H.; Guo, M.; He, J.; Shen, X.; Song, J. Low Habitual Dietary Calcium and Linear Growth from Adolescence to Young Adulthood: Results from the China Health and Nutrition Survey. Sci. Rep. 2017, 7, 9111. [Google Scholar] [CrossRef]
- Ershow, A.G.; Wong-Chen, K. Chinese food composition tables. J. Food Compos. Anal. 1990, 3, 191–434. [Google Scholar] [CrossRef]
- Bennett, D.A. How can I deal with missing data in my study? Aust. N. Z. J. Public Health 2001, 25, 464–469. [Google Scholar] [CrossRef]
- Jorde, R.; Sundsfjord, J.; Haug, E.; Bønaa, K.H. Relation between low calcium intake, parathyroid hormone, and blood pressure. Hypertension 2000, 35, 1154–1159. [Google Scholar] [CrossRef]
- Jayedi, A.; Zargar, M.S. Dietary calcium intake and hypertension risk: A dose–response meta-analysis of prospective cohort studies. Eur. J. Clin. Nutr. 2018, 73, 969–978. [Google Scholar] [CrossRef]
- Kamycheva, E.; Sundsfjord, J.; Jorde, R. Serum parathyroid hormone levels predict coronary heart disease: The Tromsø Study. Eur. J. Cardiovasc. Prev. Rehabilitation 2004, 11, 69–74. [Google Scholar] [CrossRef]
- Michaelsson, K.; Melhus, H.; Lemming, E.W.; Wolk, A.; Byberg, L. Long term calcium intake and rates of all cause and cardiovascular mortality: Community based prospective longitudinal cohort study. BMJ 2013, 346, f228. [Google Scholar] [CrossRef]
- Dastan, I.; Erem, A.; Çetinkaya, V. Urban and rural differences in hypertension risk factors in Turkey. Anatol. J. Cardiol. 2017, 18, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Waib, P.H.; Papini-Berto, S.J.; Habermann, F.; Burini, R.C. Calcium-intake assessment in essential-arterial hypertensive patients. Rev. Saúde Pública 1992, 26, 27–33. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wang, Y.-M.; Mo, B.-Q.; Takezaki, T.; Imaeda, N.; Kimura, M.; Wang, X.-R.; Tajima, K. Geographical variation in nutrient intake between urban and rural areas of Jiangsu province, China and development of a semi-quantitative food frequency questionnaire for middle-aged inhabitants. J. Epidemiology 2003, 13, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Roberts, M.E.; Doogan, N.J.; Kurti, A.N.; Redner, R.; Gaalema, D.E.; Stanton, C.A.; White, T.J.; Higgins, S.T. Rural tobacco use across the United States: How rural and urban areas differ, broken down by census regions and divisions. Health Place 2016, 39, 153–159. [Google Scholar] [CrossRef]
- O’Connor, A.; Wellenius, G.A. Rural–urban disparities in the prevalence of diabetes and coronary heart disease. Public Health 2012, 126, 813–820. [Google Scholar] [CrossRef]
- Xing, L.; Jing, L.; Tian, Y.; Lin, M.; Du, Z.; Yan, H.; Ren, G.; Dong, Y.; Sun, Q.; Liu, S. Urban-Rural disparities in status of hypertension in northeast China: A population-based study, 2017-2019. Clin. Epidemiol. 2019, 11, 801–820. [Google Scholar] [CrossRef]
- Li, J.; Shi, L.; Li, S.; Xu, L.; Qin, W.; Wang, H. Urban-rural disparities in hypertension prevalence, detection, and medication use among Chinese Adults from 1993 to 2011. Int. J. Equity Health 2017, 16, 50. [Google Scholar] [CrossRef]
- Li, M.; Shi, Z. Dietary Pattern during 1991–2011 and Its Association with Cardio Metabolic Risks in Chinese Adults: The China Health and Nutrition Survey. Nutrients 2017, 9, 1218. [Google Scholar] [CrossRef]
| Variables | Urban 876 | Rural 1342 | p-Value | ||
|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | ||
| Sex (%) | 0.53 | ||||
| Male | 55 | 55 | 55.6 | 55.6 | - |
| Female | 45 | 45 | 44.4 | 44.4 | - |
| Age in years | 49.4 (12.8) | 58.4 (12.9) | 48.8 (11.4) | 57.8 (11.4) | 0.012 |
| Smoking status (%) | 0.001 | ||||
| Non-smoking | 67.5 | 70.9 | 63.1 | 66.2 | - |
| Smoking | 32.5 | 29.1 | 36.9 | 33.8 | - |
| Frequency of alcohol consumption (%) | <0.0001 | ||||
| Non-drinkers | 60.3 | 61.0 | 63.4 | 65.4 | - |
| 1 to 4 times/week | 36.9 | 33.1 | 34.1 | 31.8 | - |
| More than 5 times/week | 2.9 | 5.9 | 2.6 | 2.8 | - |
| Hypertension diagnostics (%) | <0.0001 | ||||
| No | 94.3 | 85.3 | 90.2 | 78.2 | - |
| Yes | 5.7 | 14.7 | 9.8 | 21.8 | - |
| Dietary calcium intake (mg/day) | 433.8 (594.5) | 429.8 (243.3) | 403.5 (321.82) | 388.5 (243.3) | <0.0001 |
| Systolic blood pressure (mmHg) | 123.1 (17.6) | 130.3 (18.6) | 121.1 (17.7) | 129.5 (19.22) | <0.0001 |
| Diastolic blood pressure (mmHg) | 79.1 (11.4) | 82.3 (10.8) | 78.4 (10.7) | 81.30 (10.9) | 0.02 |
| BMI | 23.6 (3.3) | 23.9 (3.5) | 22.9 (3.2) | 23.4 (3.5) | <0.0001 |
| Energy intake (kcal/day) | 2206.2 (1343.7) | 2102.1 (1118.8) | 2346.8 (1029.9) | 2345.2 (1480.3) | <0.0001 |
| Physical activity (%) | 0.009 | ||||
| Few | 21.6 | 21.6 | 12.9 | 12.9 | - |
| Moderate | 16.8 | 16.9 | 22.8 | 22.7 | - |
| High | 61.4 | 61.4 | 64.3 | 64.3 | - |
| Survey Years | 2000 | 2004 | 2006 | 2009 | ||
|---|---|---|---|---|---|---|
| Hypertension Occurrence—Mean rank (Chi square) | Male | Urban N = 441 | 803.5 | 804.1 | 705.2 | 846.9 |
| Rural N = 1102 | 759.4 | 786.5 | 696.0 | 812.8 | ||
| χ2 (p-value) | ἠ | ἠ | ἠ | ἠ | ||
| FeMale | Urban N = 876 | 567.8 | 673.0 | 614.9 | 712.1 | |
| Rural | 606.91 | 630.6 | 580.5 | 644.1 | ||
| χ2 | 5.1 * | ἠ | ἠ | 8.7 ** | ||
| Dietary Calcium intake—Mean rank (Chi square) | Male | Urban | 878.3 | 930.2 | 893.4 | 910.4 |
| Rural | 818.8 | 797.8 | 812.7 | 805.8 | ||
| χ2 | 5.2 * | 25.8 *** | 9.6 ** | 16.1 *** | ||
| FeMale | Urban | 733.5 | 753.3 | 758.4 | 751.9 | |
| Rural | 645.7 | 637.5 | 625.4 | 638.0 | ||
| χ2 | 14.3 *** | 24.9 *** | 28.0 *** | 24.0 *** | ||
| Model | Living Location | |
|---|---|---|
| Rural | Urban | |
| Model 1 | - | - |
| OR | 1.03 | 1.13 |
| 95% CI | (0.96–1.09) | (1.04–1.22) |
| Model 2 | - | - |
| OR | 1.05 | 1.14 |
| 95% CI | (0.98–1.12) | (1.06–1.24) |
| Model 3 | - | - |
| OR | 1.04 | 1.16 |
| 95% CI | (0.97–1.12) | (1.06–1.26) |
| Models | Living Locations | Female | Male | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | ||
| Model 1 | Urban | 1 | 1.8 | 1.73 | 1.77 | 1 | n1.4 | n1.1 | 1.9 |
| OR (95% CI) | (1.2–2.7) | (1.2–2.6) | (1.2–2.6) | (0.9–2.1) | (0.7–1.6) | (1.3–2.8) | |||
| Rural | 1 | 1.2 | 0.9 | 0.9 | 1 | 1.0 | 1.4 | 1.6 | |
| OR (95% CI) | (0.9–1.6) | (0.6–1.2) | (0.7–1.2) | (0.7–1.4) | (1.1–1.9) | (1.2–2.1) | |||
| Model 2 | Urban | 1 | 2 | 1.98 | 1.88 | 1 | 1.6 | 1.2 | 2.3 |
| OR (95% CI) | (1.3–3) | (1.2–2.9) | (1.2–2.7) | (1.0–2.4) | (0.8–1.9) | (1.56–3.5) | |||
| Rural | 1 | 1.3 | 0.9 | 0.9 | 1 | 1.1 | 1.6 | 1.7 | |
| OR (95% CI) | (0.9–1.7) | (0.7–1.3) | (0.7–1.3) | (0.8–1.5) | (1.2–1.3) | (1.3–2.3) | |||
| Model 3 | Urban | 1 | 2.0 | 1.8 | 1.9 | 1 | 1.4 | 1.2 | 2.3 |
| OR (95% CI) | (1.3–3.2) | (1.2–2.8) | (1.2–2.8) | (0.9–2.3) | (0.7–1.9) | (1.6–3.6) | |||
| Rural | 1 | 1.2 | 0.8 | 0.9 | 1 | 1.1 | 1.4 | 1.6 | |
| OR (95% CI) | (0.9–1.6) | (0.6–1.1) | (0.6–1.2) | (0.7–1.5) | (1.0–1.9) | (1.1–2.1) | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ngo Nkondjock, V.-R.; Li, Y.; Thérèse Martin, C.W.; Reem, A. Rural and Urban Population Differences in the Association of Dietary Calcium with Blood Pressure and Hypertension Occurrence: Analysis of Longitudinal Data from the China Health and Nutrition Survey. J 2020, 3, 90-99. https://doi.org/10.3390/j3010009
Ngo Nkondjock V-R, Li Y, Thérèse Martin CW, Reem A. Rural and Urban Population Differences in the Association of Dietary Calcium with Blood Pressure and Hypertension Occurrence: Analysis of Longitudinal Data from the China Health and Nutrition Survey. J. 2020; 3(1):90-99. https://doi.org/10.3390/j3010009
Chicago/Turabian StyleNgo Nkondjock, Victorine-Raïssa, Ying Li, Cheteu Wabo Thérèse Martin, and Alariqi Reem. 2020. "Rural and Urban Population Differences in the Association of Dietary Calcium with Blood Pressure and Hypertension Occurrence: Analysis of Longitudinal Data from the China Health and Nutrition Survey" J 3, no. 1: 90-99. https://doi.org/10.3390/j3010009
APA StyleNgo Nkondjock, V.-R., Li, Y., Thérèse Martin, C. W., & Reem, A. (2020). Rural and Urban Population Differences in the Association of Dietary Calcium with Blood Pressure and Hypertension Occurrence: Analysis of Longitudinal Data from the China Health and Nutrition Survey. J, 3(1), 90-99. https://doi.org/10.3390/j3010009





