Effect of the Rovatti Method® (Physiotherapeutic Scoliosis-Specific Exercises) in an Adolescent Patient with Idiopathic Scoliosis: A Case Report
Abstract
1. Introduction and Clinical Significance
2. Case Presentation
2.1. Methods
2.2. Results
3. Discussion
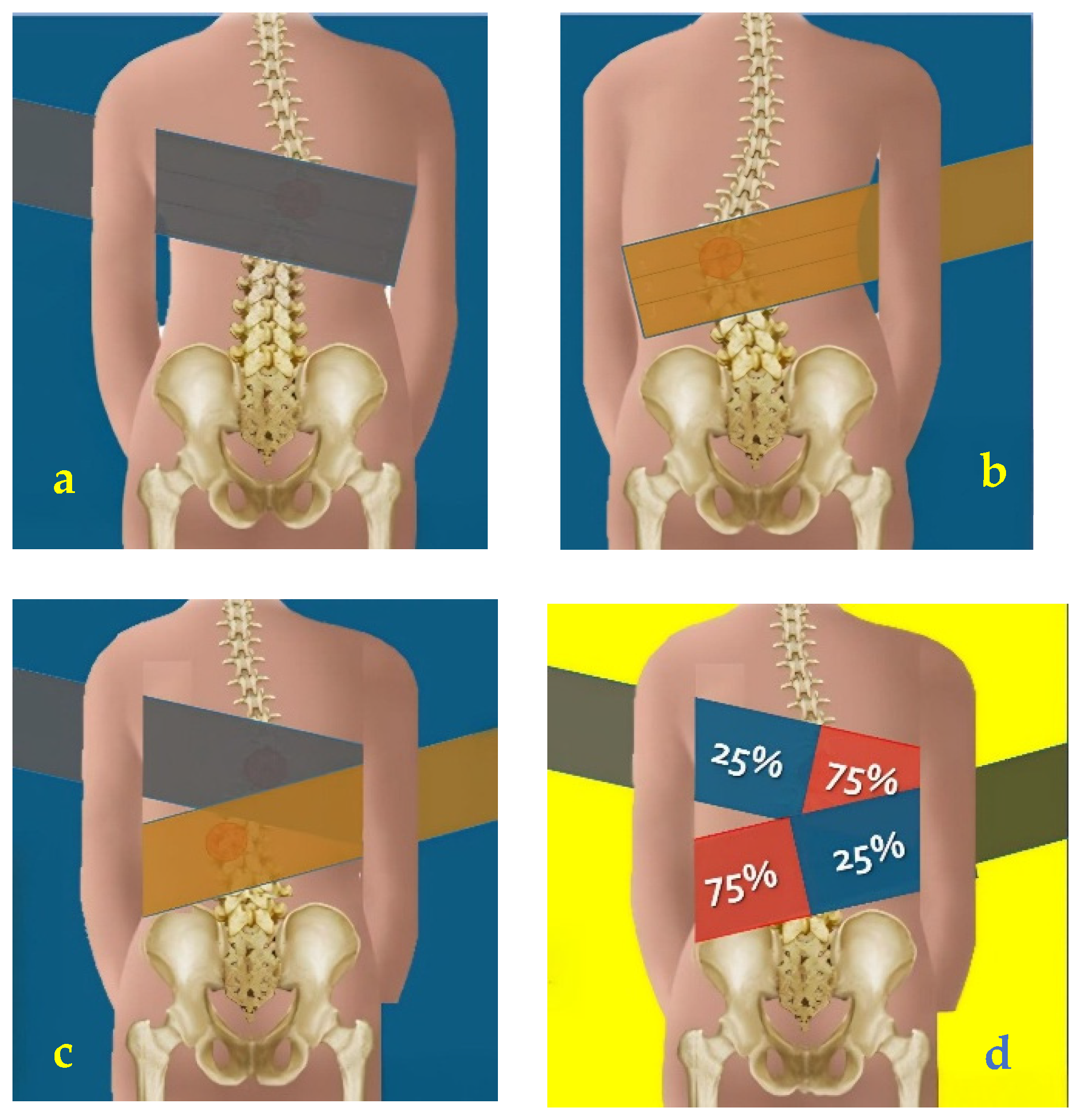
- Direct vectors: the tension of the elastic band is applied in such a way as to guide the body in the direction of correction, providing support that facilitates reaching the correct position. This approach is useful in patients who need more structured guidance and constant reinforcement of self-correction [43,44].
- Indirect Vectors (Reactive Neuromuscular Training—RNT): in this case, the resistance of the elastic band is applied in the opposite direction to the correction, inducing an active compensatory response from the patient [45]. This type of stimulus exploits the principle of neuromuscular hyper-correction, forcing the patient to counteract the force of the rubber band and respond with a more intense active correction. The RNT method is particularly effective in those patients who respond better to counterfactual stimuli, improving neuromuscular control and active stabilization of the spine [46,47,48].
3.1. Advantages of the Rovatti Method
- -
- Better cost–benefit ratio, since it is not a one-to-one, therapist-patient, exclusively manual treatment, allowing work in small groups. This approach reduces costs and permits treatment to be extended in the medium to long term, a key aspect for a condition such as scoliosis, which requires a continuous approach over time.
- -
- Ability to create small groups, fostering mutual support among patients and improving the therapeutic experience, both in terms of motivation and effectiveness.
- -
- Increased therapeutic adherence, thanks to a method that actively involves the patient in the rehabilitation process, making them more aware and responsible for their own postural correction. The corrective approach in the Rovatti Method® is based on three-dimensional management of scoliosis, intervening in the different planes of movement:
- (a)
- Sagittal plane: The main objective is to restore the physiological curves of the spine, providing balance between lumbar lordosis, dorsal kyphosis, and cervical lordosis [1,51]. Scoliosis, being a three-dimensional deformity, often alters the natural alignment of the vertebral curves, making their restoration essential to improve the biomechanics and stability of the spine [27].
- (b)
- (c)
3.2. Limitations of the Rovatti Method
3.3. Limitations of the Study
3.4. Patient Perspective
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; De Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Richards, B.S.; Bernstein, R.M.; D’Amato, C.R.; Thompson, G.H. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on bracing and nonoperative management. Spine 2005, 30, 2068–2075; discussion 2076–2077. [Google Scholar] [CrossRef] [PubMed]
- Burwell, R.G.; James, N.J.; Johnson, F.; Webb, J.K.; Wilson, Y.G. Standardised trunk asymmetry scores. A study of back contour in healthy school children. J. Bone Jt. Surg. Br. Vol. 1983, 65, 452–463. [Google Scholar] [CrossRef] [PubMed]
- Brooks, H.L.; Azen, S.P.; Gerberg, E.; Brooks, R.; Chan, L. Scoliosis: A prospective epidemiological study. J. Bone Jt. Surg. 1975, 57, 968–972. [Google Scholar] [CrossRef] [PubMed]
- Parent, S.; Newton, P.O.; Wenger, D.R. Adolescent idiopathic scoliosis: Etiology, anatomy, natural history, and bracing. Instr. Course Lect. 2005, 54, 529–536. [Google Scholar] [PubMed]
- Plaszewski, M.; Nowobilski, R.; Kowalski, P.; Cieslinski, M. Screening for scoliosis: Different countries’ perspectives and evidence-based health care. Int. J. Rehabil. Res. 2012, 35, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Grivas, T.B.; Vasilidis, E.; Savvidou, O.; Mouzakis, V.; Koufopouloset, G. Geographic latitude and prevalence of adolescent idiopathic scoliosis. Stud. Health Technol. Inform. 2006, 123, 84–89. [Google Scholar] [PubMed]
- Dimeglio, A.; Canavese, F. The immature spine: Growth and idiopathic scoliosis. Ann. Transl. Med. 2020, 8, 22. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gallego-Siles, J.R.; Siles-Fuentes, M.J.; Ibáñez-Vera, A.J.; Cortés-Pérez, I.; Obrero-Gaitán, E.; Lomas-Vega, R. Idiopathic scoliosis in subjects with eye diseases: A systematic review with meta-analysis. Ann. N. Y. Acad. Sci. 2024, 1533, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Cortés-Pérez, I.; Salamanca-Montilla, L.; Gámiz-Bermúdez, F.; Obrero-Gaitán, E.; Ibáñez-Vera, A.J.; Lomas-Vega, R. Vestibular Morphological Alterations in Adolescent Idiopathic Scoliosis: A Systematic Review of Observational Studies. Children 2022, 10, 35. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gámiz-Bermúdez, F.; Ibáñez-Vera, A.J.; Obrero-Gaitán, E.; Cortés-Pérez, I.; Zagalaz-Anula, N.; Lomas-Vega, R. Relationship between stomatognathic alterations and idiopathic scoliosis: A systematic review with meta-analysis of observational studies. EFORT Open Rev. 2023, 8, 771–780. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhu, Q.; Chen, J.; Chen, C.; Wang, H.; Yang, S. Association between calcium-phosphorus balance and adolescent idiopathic scoliosis: A meta-analysis. Acta Orthop. Traumatol. Turc. 2019, 53, 468–473. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Qiu, X.S.; Tang, N.L.; Yeung, H.Y.; Lee, K.M.; Hung, V.W.; Ng, B.K.; Ma, S.L.; Kwok, R.H.; Qin, L.; Qiu, Y.; et al. Melatonin receptor 1B (MTNR1B) gene polymorphism is associated with the occurrence of adolescent idiopathic scoliosis. Spine 2007, 32, 1748–1753. [Google Scholar] [CrossRef] [PubMed]
- Van Blarcum, G.S.; Wagner, S.C.; Meyer, R.M.; Kang, D.G.; Lehmann, R.A. The Biomechanics of Spinal Deformity in Adolescent Idiopathic Scoliosis. J. Spine 2014, 4, 197. [Google Scholar] [CrossRef]
- Hefti, F. Pathogenesis and biomechanics of adolescent idiopathic scoliosis (AIS). J. Child. Orthop. 2013, 7, 17–24. [Google Scholar] [CrossRef]
- Le Berre, M.; Pradeau, C.; Brouillard, A.; Coget, M.; Massot, C.; Catanzariti, J.F. Do Adolescents With Idiopathic Scoliosis Have an Erroneous Perception of the Gravitational Vertical? Spine Deform. 2019, 7, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Hresko, T.M.; O’Brien, J.P.; Price, N.; SOSORT Boards; SRS Non-Operative Committee. Recommendations for research studies on treatment of idiopathic scoliosis: Consensus 2014 between SOSORT and SRS non-operative management committee. Scoliosis 2015, 10, 8. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Negrini, S.; Donzelli, S.; Negrini, A.; Parzini, S.; Romano, M.; Zaina, F. Specific exercises reduce the need for bracing in adolescents with idiopathic scoliosis: A practical clinical trial. Ann. Phys. Rehabil. Med. 2019, 62, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Minozzi, S.; Bettany-Saltikov, J.; Chockalingam, N.; Grivas, T.B.; Kotwicki, T.; Maruyama, T.; Romano, M.; Zaina, F. Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst. Rev. 2015, 2015, CD006850. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Romano, M.; Minozzi, S.; Bettany-Saltikov, J.; Zaina, F.; Chockalingam, N.; Kotwicki, T.; Maier-Hennes, A.; Arienti, C.; Negrini, S. Therapeutic exercises for idiopathic scoliosis in adolescents. Cochrane Database Syst. Rev. 2024, 2, CD007837. [Google Scholar] [CrossRef] [PubMed]
- Seleviciene, V.; Cesnaviciute, A.; Strukcinskiene, B.; Marcinowicz, L.; Strazdiene, N.; Genowska, A. Physiotherapeutic Scoliosis-Specific Exercise Methodologies Used for Conservative Treatment of Adolescent Idiopathic Scoliosis, and Their Effectiveness: An Extended Literature Review of Current Research and Practice. Int. J. Environ. Res. Public Health 2022, 19, 9240. [Google Scholar] [CrossRef]
- Bettany-Saltikov, J.; Parent, E.; Romano, M.; Villagrasa, M.; Negrini, S. Physiotherapeutic Scoliosis-Specific Exercises for Adolescents with Idiopathic Scoliosis. Eur. J. Phys. Rehabil. Med. 2014, 50, 111–121. [Google Scholar] [PubMed]
- Berdishevsky, H.; Lebel, V.A.; Bettany-Saltikov, J.; Rigo, M.; Lebel, A.; Hennes, A.; Romano, M.; Białek, M.; M’hango, A.; Betts, T.; et al. Physiotherapy Scoliosis-Specific Exercises—A Comprehensive Review of Seven Major Schools. Scoliosis Spinal Disord. 2016, 11, 20. [Google Scholar] [CrossRef]
- Weiss, H.-R.; Negrini, S.; Hawes, M.C.; Rigo, M.; Kotwicki, T.; Grivas, T.B.; Maruyama, T.; Sosort, M.O.T. Physical exercises in the treatment of idiopathic scoliosis at risk of brace treatment—SOSORT consensus paper 2005. Scoliosis 2006, 1, 6. [Google Scholar] [CrossRef]
- Ward, W.T.; Friel, N.A.; Kenkre, T.S.; Brooks, M.M.; Londino, J.A.; Roach, J.V. SRS-22r Scores in non-operated adolescent idiopathic scoliosis patients with curves greater than forty degrees. Spine 2017, 42, 1233–1240. [Google Scholar] [CrossRef]
- Weiss, H.R.; Kravidas, N.; Moramarco, M.; Moramarco, K. Long terms effects of untreated adolescents idiopathic scoliosis: A review of the literature. Asian Spine J. 2016, 10, 1163–1169. [Google Scholar] [CrossRef]
- Monticone, M.; Ambrosini, E.; Cazzaniga, D.; Rocca, B.; Ferrante, S. Active self-correction and task-orientated exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis. Results of randomized controlled trial. Eur. Spine J. 2014, 23, 1204–1214. [Google Scholar] [CrossRef]
- Rovatti, E.; Rovatti, M. Scoliosi Idiopatica: Trattamento Conservativo con le Bande Elastiche: Manuale Pratico del Metodo Rovatti®; Edizioni Edi Ermes: Milan, Italy, 2014. [Google Scholar]
- Belli, G.; Toselli, S.; Latessa, P.M.; Mauro, M. Evaluation of Self-Perceived Body Image in Adolescents with Mild Idiopathic Scoliosis. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 319–333. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Belli, G.; Russo, L.; Mauro, M.; Toselli, S.; Maietta Latessa, P. Relation between Photogrammetry and Spinal Mouse for Lumbopelvic Assessment in Adolescents with Thoracic Kyphosis. J. Funct. Morphol. Kinesiol. 2023, 8, 68. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Côté, P.; Kreitz, B.G.; Cassidy, J.D.; Dzus, A.K.; Martel, J. A study of the diagnostic accuracy and reliability of the Scoliometer and Adam’s forward bend test. Spine 1998, 23, 796–802, discussion 803. [Google Scholar] [CrossRef] [PubMed]
- Monticone, M.; Carabalona, R.; Negrini, S. Reliability of the Scoliosis Research Society-22 Patient Questionnaire (Italian version) in mild adolescent vertebral deformities. Eur. Medicophysica 2004, 40, 191–197. [Google Scholar] [PubMed]
- Zaina, F.; Negrini, S.; Atanasio, S. TRACE (Trunk Aesthetic Clinical Evaluation), a routine clinical tool to evaluate aesthetics in scoliosis patients: Development from the Aesthetic Index (AI) and repeatability. Scoliosis 2009, 4, 3. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schreiber, S.; Parent, E.C.; Hill, D.L.; Hedden, D.M.; Moreau, M.J.; Southon, S.C. Patients with adolescent idiopathic scoliosis perceive positive improvements regardless of change in the Cobb angle—Results from a randomized controlled trial comparing a 6-month Schroth intervention added to standard care and standard care alone. SOSORT 2018 Award winner. BMC Musculoskelet. Disord. 2019, 20, 319. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zuo, W.; Li, Y.; Zhang, Z.; Jia, G.; Huang, H.; Zhang, G.; Wang, C.; Lo, W.L.A.; Liu, P. The efficacy of combined physiotherapeutic scoliosis-specific exercises and manual therapy in adolescent idiopathic scoliosis. BMC Musculoskelet. Disord. 2024, 25, 874. [Google Scholar] [CrossRef] [PubMed]
- Monticone, M.; Ambrosini, E.; Rocca, B.; Foti, C.; Ferrante, S. Responsiveness and Minimal Important Changes of the Scoliosis Research Society-22 Patient Questionnaire in Subjects With Mild Adolescent and Moderate Adult Idiopathic Scoliosis Undergoing Multidisciplinary Rehabilitation. Spine 2017, 42, E672–E679. [Google Scholar] [CrossRef] [PubMed]
- Larson, J.E.; Meyer, M.A.; Boody, B.; Sarwark, J.F. Evaluation of angle trunk rotation measurements to improve quality and safety in the management of adolescent idiopathic scoliosis. J. Orthop. 2018, 15, 563–565. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fernandez-Gamez, B.; Pulido-Muñoz, Á.; Olvera-Rojas, M.; Solis-Urra, P.; Corral-Pérez, J.; Morales, J.S.; Jiménez-Pavón, D.; Mora-Gonzalez, J.; Esteban-Cornejo, I. Examining Elastic Band Properties for Exercise Prescription: AGUEDA Equations. Physiother. Res. Int. 2025, 30, e70010. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Uchida, M.C.; Nishida, M.M.; Sampaio, R.A.; Moritani, T.; Arai, H. Thera-band(®) elastic band tension: Reference values for physical activity. J. Phys. Ther. Sci. 2016, 28, 1266–1271. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ko, K.J.; Kang, S.J. Effects of 12-week core stabilization exercise on the Cobb angle and lumbar muscle strength of adolescents with idiopathic scoliosis. J. Exerc. Rehabil. 2017, 13, 244–249. [Google Scholar] [CrossRef]
- Russo, L.; Belli, G.; Di Blasio, A.; Lupu, E.; Larion, A.; Fischetti, F.; Montagnani, E.; Di Biase Arrivabene, P.; De Angelis, M. The Impact of Nordic Walking Pole Length on Gait Kinematic Parameters. J. Funct. Morphol. Kinesiol. 2023, 8, 50. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dufvenberg, M.; Diarbakerli, E.; Charalampidis, A.; Öberg, B.; Tropp, H.; Aspberg Ahl, A.; Möller, H.; Gerdhem, P.; Abbott, A. Six-Month Results on Treatment Adherence, Physical Activity, Spinal Appearance, Spinal Deformity, and Quality of Life in an Ongoing Randomised Trial on Conservative Treatment for Adolescent Idiopathic Scoliosis (CONTRAIS). J. Clin. Med. 2021, 10, 4967. [Google Scholar] [CrossRef] [PubMed]
- Shim, G.; Yang, D.; Cho, W.; Kim, J.; Ryu, H.; Choi, W.; Kim, J. Elastic Resistance and Shoulder Movement Patterns: An Analysis of Reaching Tasks Based on Proprioception. Bioengineering 2023, 11, 1. [Google Scholar] [CrossRef]
- Anderson, D.I. The discrimination, acquisition, and retention of aiming movements made with and without elastic resistance. Hum. Factors 1999, 41, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Guido, J.A., Jr.; Stemm, J. Reactive Neuromuscular Training: A Multi-level Approach to Rehabilitation of the Unstable Shoulder. N. Am. J. Sports Phys. Ther. 2007, 2, 97–103. [Google Scholar] [PubMed] [PubMed Central]
- Proske, U.; Gandevia, S.C. The proprioceptive senses: Their roles in signaling body shape, body position and movement, and muscle force. Physiol. Rev. 2012, 92, 1651–1697. [Google Scholar] [CrossRef] [PubMed]
- Jull, G.A.; Richardson, C.A. Motor Control Problems in Patients With Spinal Pain: A New Direction for Therapeutic Exercise. J. Manip. Physiol. Ther. 2000, 23, 115–117. [Google Scholar] [CrossRef] [PubMed]
- Riemann, B.L.; Lephart, S.M. The Sensorimotor System, Part I: The Physiologic Basis of Functional Joint Stability. J. Athl. Train. 2002, 37, 71–79. [Google Scholar] [PubMed] [PubMed Central]
- Kiers, H.; Van Dieën, J.; Dekkers, H.; Wittink, H.; Vanhees, L. A systematic review of the relationship between physical activities in sports or daily life and postural sway in upright stance. Sports Med. 2013, 43, 1171–1189. [Google Scholar] [CrossRef]
- Gámiz-Bermúdez, F.; Obrero-Gaitán, E.; Zagalaz-Anula, N.; Lomas-Vega, R. Corrective exercise-based therapy for adolescent idiopathic scoliosis: Systematic review and meta-analysis. Clin. Rehabil. 2022, 36, 597–608. [Google Scholar] [CrossRef]
- Mac-Thiong, J.-M.; Labelle, H.; Charlebois, M.; Huot, M.-P.; de Guise, J.A. Sagittal plane analysis of the spine and pelvis in adolescent idiopathic scoliosis according to the coronal curve type. Spine 2003, 28, 1404–1409. [Google Scholar] [CrossRef] [PubMed]


| Session duration | 60 min |
| Frequency | 2×/week (occasionally 3×) |
| Structure | ~12 exercises, 5 min each – Active phase: ~30 s/rep – Rest 1:2 ratio (half the active duration), or 1:1 for more intense exercises |
| Principles | Rovatti Method®: self-correction + elastic bands (direct/indirect), guided breathing, controlled return |
| Focus | Sagittal alignment, lumbopelvic stabilization, core strengthening |
| Setting | Small AIS groups, supervised by experienced physiotherapists, comfortable environment |
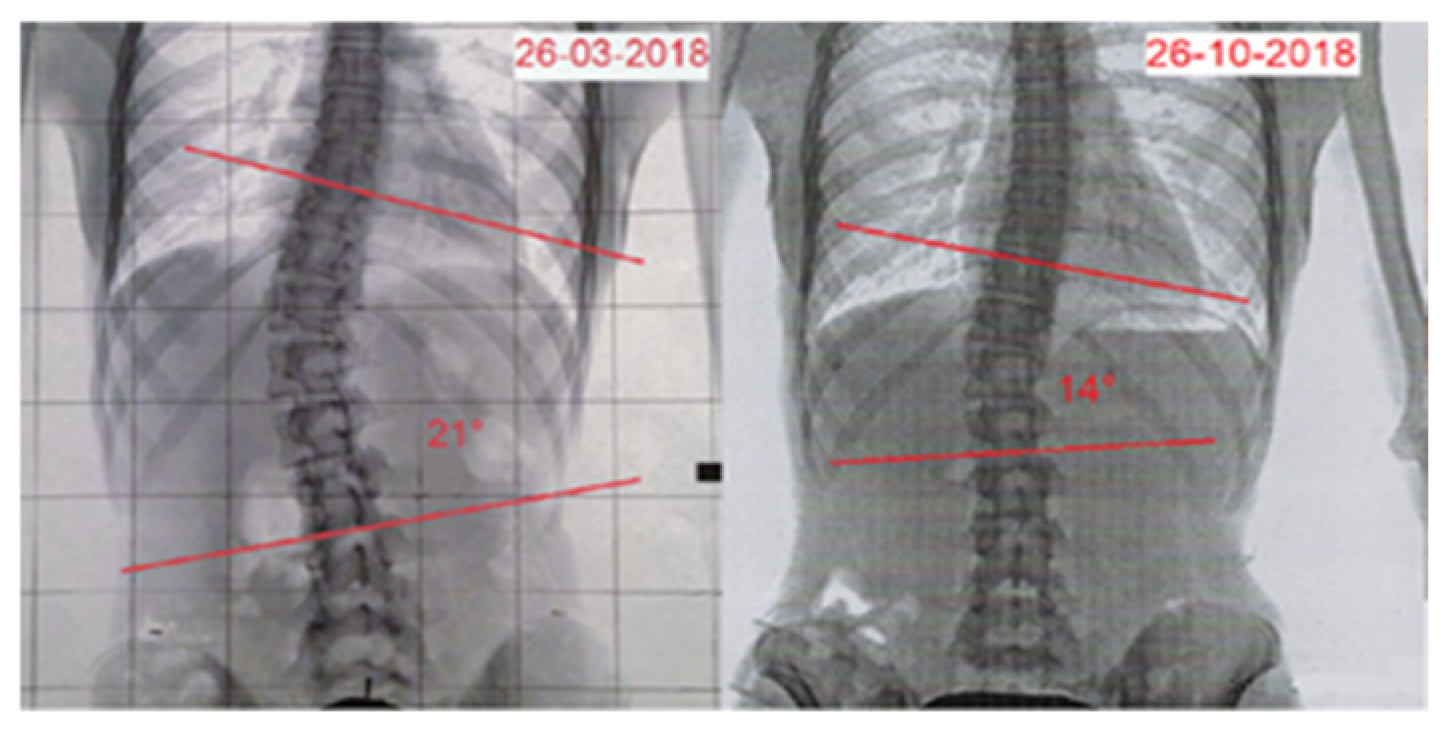
| Time | Age | Standing Height | Sitting Height | Weight | Cobb Angle | Risser | ATR | SRS-22 | TRACE |
|---|---|---|---|---|---|---|---|---|---|
| Pre | 13.4 | 156 cm | 81 cm | 42 kg | 21° | 2/3+ | 10° | 2.27 | 8 |
| Post | 13.11 | 157 cm | 82 cm | 45 kg | 14° | 3/4+ | 8° | 3.05 | 4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rovatti, M.; Rovatti, E.; Belli, G.; Baldoni, N.; Maietta Latessa, P. Effect of the Rovatti Method® (Physiotherapeutic Scoliosis-Specific Exercises) in an Adolescent Patient with Idiopathic Scoliosis: A Case Report. Reports 2025, 8, 171. https://doi.org/10.3390/reports8030171
Rovatti M, Rovatti E, Belli G, Baldoni N, Maietta Latessa P. Effect of the Rovatti Method® (Physiotherapeutic Scoliosis-Specific Exercises) in an Adolescent Patient with Idiopathic Scoliosis: A Case Report. Reports. 2025; 8(3):171. https://doi.org/10.3390/reports8030171
Chicago/Turabian StyleRovatti, Marco, Emanuele Rovatti, Guido Belli, Niccolò Baldoni, and Pasqualino Maietta Latessa. 2025. "Effect of the Rovatti Method® (Physiotherapeutic Scoliosis-Specific Exercises) in an Adolescent Patient with Idiopathic Scoliosis: A Case Report" Reports 8, no. 3: 171. https://doi.org/10.3390/reports8030171
APA StyleRovatti, M., Rovatti, E., Belli, G., Baldoni, N., & Maietta Latessa, P. (2025). Effect of the Rovatti Method® (Physiotherapeutic Scoliosis-Specific Exercises) in an Adolescent Patient with Idiopathic Scoliosis: A Case Report. Reports, 8(3), 171. https://doi.org/10.3390/reports8030171







