Cognitive Analytic Therapy for Functional/Dissociative Seizures in an Adolescent: Case Report and Mixed-Methods Single-Case Evaluation
Abstract
1. Introduction and Clinical Significance
2. Case Presentation
2.1. Physical Health, Mental Health, and Functional/Dissociative Seizures
2.2. Design
2.3. Idiographic Outcome Measures and Analysis Strategy
2.4. Nomothetic Outcome Measures and Analysis Strategy
2.5. Change Interview
2.6. Treatment
2.7. Results and Outcomes
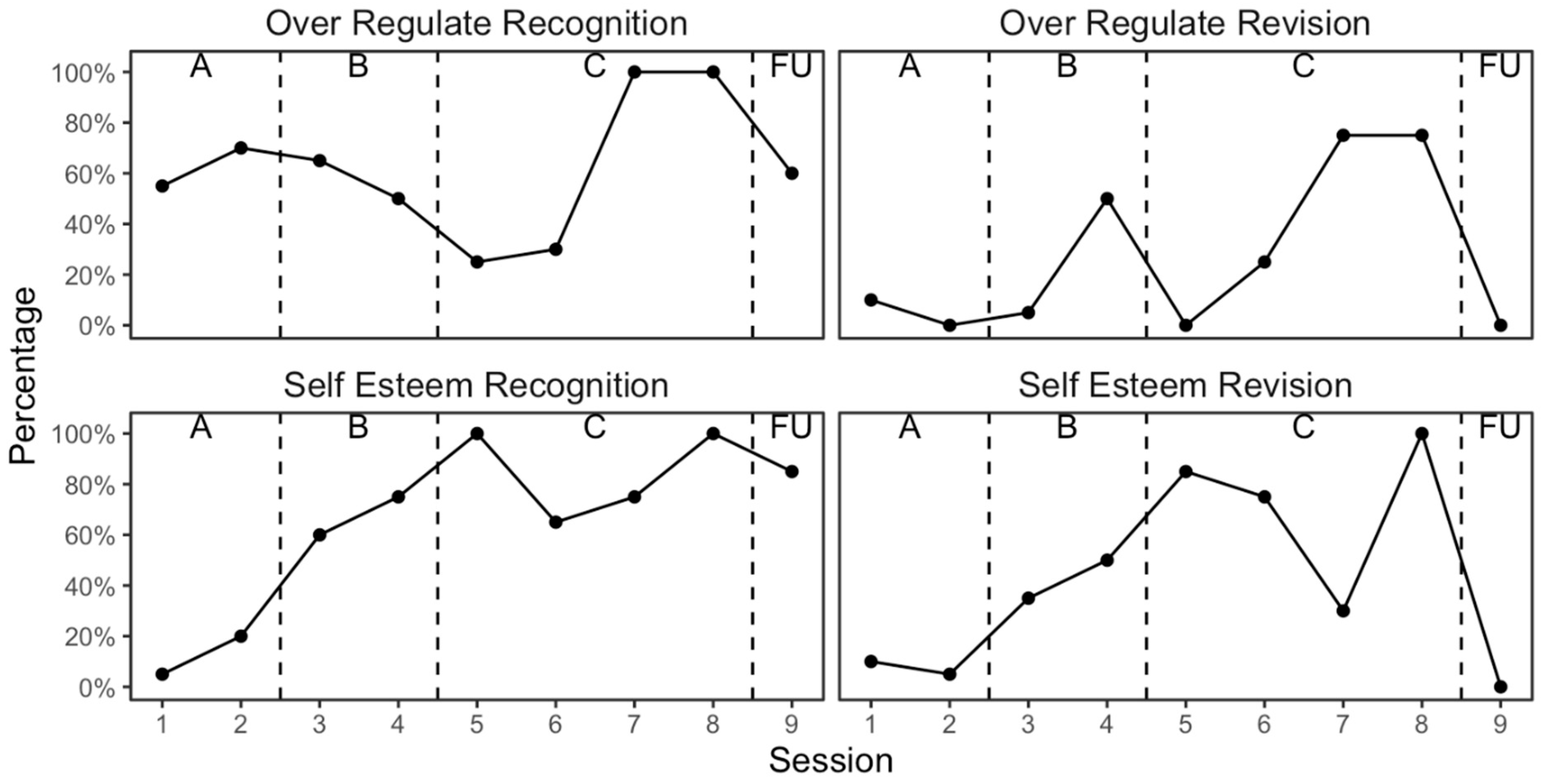
2.8. Changes in Target Problems and Target Problem Procedures
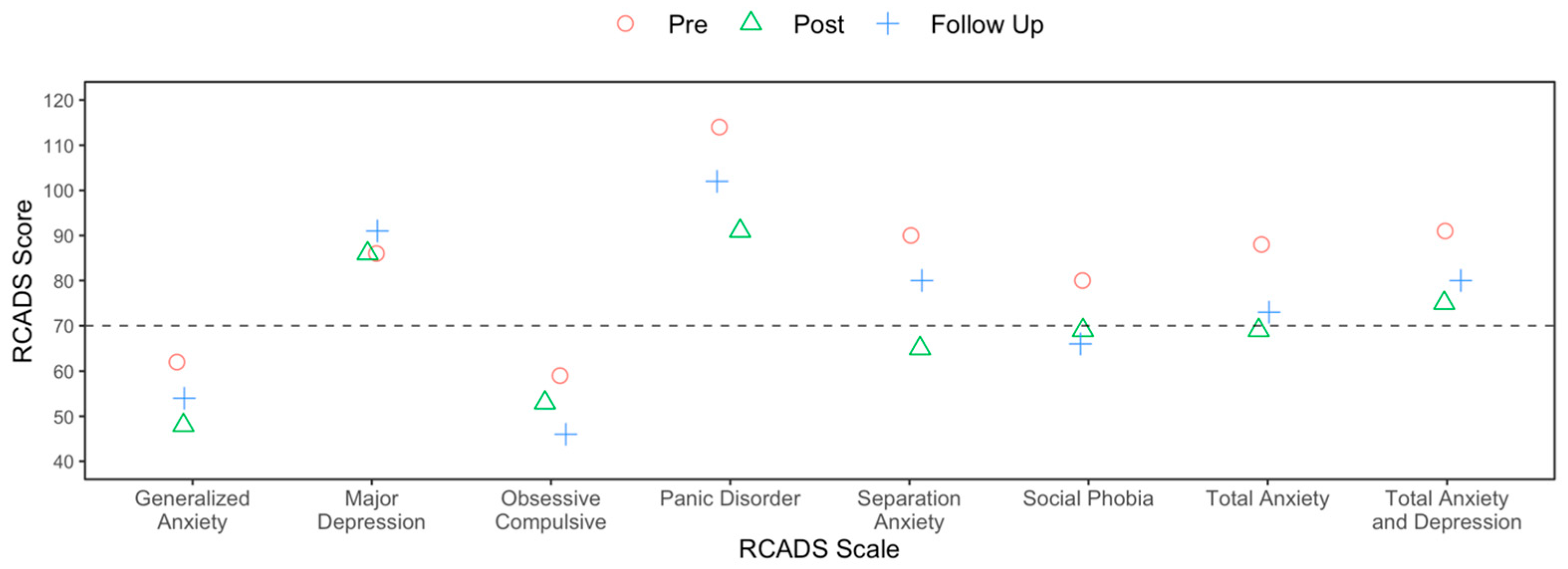
2.9. Nomothetic Outcomes
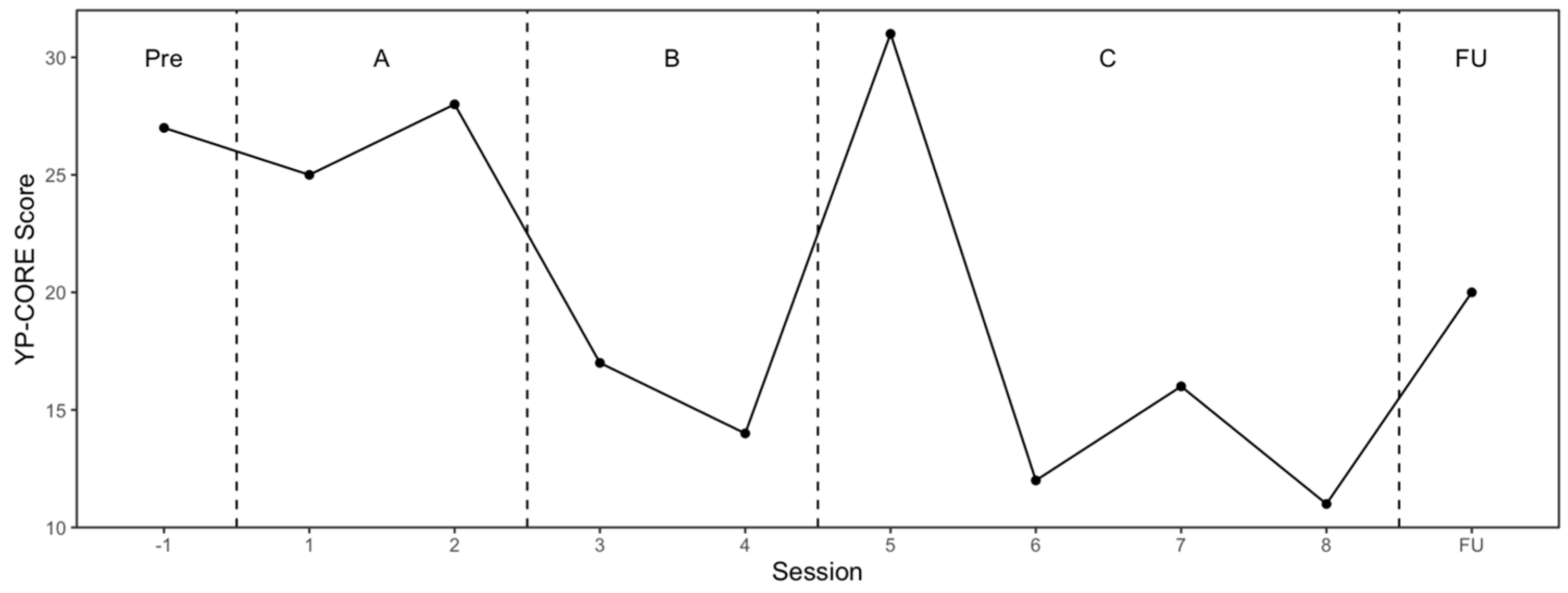
2.10. Session Impact
2.11. Change Interview Results
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CAT | Cognitive analytic therapy |
| SCED | Single case experimental design |
| SES | Session Evaluation Scale |
| FDS | Functional dissociative seizure |
| FND | Functional neurological disorder |
| YP-CORE | Young Persons Clinical Outcome Routine Evaluation |
| RCADS | Revised Children’s Anxiety and Depression Scale |
| DES-II | Dissociative Experiences Scale-II |
| NR | Narrative reformulation |
| SDR | Sequential diagrammatic reformulation |
| TP | Target problem |
| TPP | Target problem procedure |
References
- Drane, D.L.; Fani, N.; Hallett, M.; Khalsa, S.S.; Perez, D.L.; Roberts, N.A. A framework for understanding the pathophysiology of Functional Neurological Disorder. CNS Spectr. 2021, 26, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Ani, C.; Reading, R.; Lynn, R.; Forlee, S.; Garralda, E. Incidence and 12-month outcome of non-transient childhood Conversion Disorder in the UK and Ireland. Br. J. Psychiatry 2013, 202, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Reuber, M.; Rawlings, G.H. Nonepileptic seizures—Subjective phenomena. Handb. Clin. Neurol. 2016, 139, 283–296. [Google Scholar] [CrossRef]
- Yong, K.; Chin, R.F.M.; Shetty, J.; Hogg, K.; Burgess, K.; Lindsay, M.; McLellan, A.; Stone, J.; Kamath Tallur, K.; Baxter, A.; et al. Functional Neurological Disorder in children and young people: Incidence, clinical features, and prognosis. Dev. Med. Child Neurol. 2023, 65, 1238–1246. [Google Scholar] [CrossRef] [PubMed]
- Kozlowska, K.; Nunn, K.P.; Rose, D.; Morris, A.; Ouvrier, R.A.; Varghese, J. Conversion Disorder in Australian pediatric practice. J. Am. Acad. Child Adolesc. Psychiatry 2007, 46, 68–75. [Google Scholar] [CrossRef]
- Espay, A.J.; Aybek, S.; Carson, A.; Edwards, M.J.; Goldstein, L.H.; Hallett, M.; LaFaver, K.; LaFrance, W.C.; Lang, A.E.; Nicholson, T.; et al. Current concepts in diagnosis and treatment of functional neurological disorders. JAMA Neurol. 2018, 75, 1132–1141. [Google Scholar] [CrossRef]
- Raper, J.; Currigan, V.; Fothergill, S.; Stone, J.; Forsyth, R.J. Long-term outcomes of Functional Neurological Disorder in children. Arch. Dis. Child. 2019, 104, 1155–1160. [Google Scholar] [CrossRef]
- Leary, P.M. Conversion Disorder in childhood--diagnosed too late, investigated too much? J. R. Soc. Med. 2003, 96, 436–438. [Google Scholar] [CrossRef]
- Operto, F.F.; Coppola, G.; Mazza, R.; Pastorino, G.M.G.; Campanozzi, S.; Margari, L.; Roccella, M.; Marotta, R.; Carotenuto, M. Psychogenic nonepileptic seizures in pediatric population: A review. Brain Behav. 2019, 9, e01406. [Google Scholar] [CrossRef]
- Villagrán, A.; Eldøen, G.; Duncan, R.; Aaberg, K.M.; Hofoss, D.; Lossius, M.I. Incidence and prevalence of psychogenic nonepileptic seizures in a Norwegian county: A 10-year population-based study. Epilepsia 2021, 62, 1528–1535. [Google Scholar] [CrossRef]
- Stone, J.; Hallett, M.; Carson, A.; Bergen, D.; Shakir, R. Functional disorders in the neurology section of ICD-11: A landmark opportunity. Neurology 2014, 83, 2299–2301. [Google Scholar] [CrossRef] [PubMed]
- ICD-11 International Classification of Diseases 11th Revision, World Health Organization (WHO). Available online: https://icd.who.int/en/ (accessed on 20 May 2025).
- Asadi-Pooya, A.A.; Brigo, F.; Kozlowska, K.; Perez, D.L.; Pretorius, C.; Sawchuk, T.; Saxena, A.; Tolchin, B.; Valente, K.D. Social aspects of life in patients with functional seizures: Closing the gap in the biopsychosocial formulation. Epilepsy Behav. 2021, 117, 107903. [Google Scholar] [CrossRef] [PubMed]
- Vassilopoulos, A.; Mohammad, S.; Dure, L.; Kozlowska, K.; Fobian, A.D. Treatment approaches for functional neurological disorders in children. Curr. Treat. Options Neurol. 2022, 24, 77–97. [Google Scholar] [CrossRef] [PubMed]
- Varley, D.; Sweetman, J.; Brabyn, S.; Lagos, D.; van der Feltz-Cornelis, C. The clinical management of Functional Neurological Disorder: A scoping review of the literature. J. Psychosom. Res. 2023, 165, 111121. [Google Scholar] [CrossRef]
- Elliott, L.; Carberry, C. Treatment of pediatric Functional Neurological Symptom Disorder: A review of the state of the literature. Semin. Pediatr. Neurol. 2022, 41, 100952. [Google Scholar] [CrossRef]
- Bodde, N.M.G.; Lazeron, R.H.C.; Wirken, J.M.A.; van der Kruijs, S.J.; Aldenkamp, A.P.; Boon, P.A.J.M. Patients with psychogenic non-epileptic seizures referred to a tertiary epilepsy centre: Patient characteristics in relation to diagnostic delay. Clin. Neurol. Neurosurg. 2012, 114, 217–222. [Google Scholar] [CrossRef]
- Ryle, A.; Kerr, I.B. Introducing Cognitive Analytic Therapy: Principles and Practice of a Relational Approach to Mental Health, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2020. [Google Scholar]
- Nasiri, H.; Ebrahimi, A.; Zahed, A.; Arab, M.; Samouei, R. Cognitive-Analytical Therapy for a patient with Functional Neurological Symptom Disorder-Conversion Disorder (psychogenic myopia): A case study. J. Res. Med. Sci. 2015, 20, 522–524. [Google Scholar] [CrossRef]
- Tinlin-Dixon, R. Using Cognitive Analytic Therapy as a transdiagnostic intervention for comorbid personality disorder, Posttraumatic Stress Disorder, and Functional Neurological Symptom Disorder: A case report of a 68 woman’s journey toward the integration of dissociated self-states. Clin. Case Stud. 2023, 23, 146–164. [Google Scholar] [CrossRef]
- Kellett, S.; Gaskill, C.; Dunning, I.; Pope, J.; Simmonds-Buckley, M.; Lorimor, B. Inpatient cognitive analytic therapy for functional neurological disorder. Psychol. Psychother. 2025; under review. [Google Scholar]
- Hersen, M. Single-Case Experimental Designs. In International Handbook of Behavior Modification and Therapy, 2nd ed.; Hersen, M., Kazdin, A.E., Eds.; Springer: Boston, MA, USA, 1990; pp. 175–210. [Google Scholar] [CrossRef]
- British Psychological Society. Available online: https://www.bps.org.uk/guideline/functional-neurological-disorder-neuropsychological-and-psychological-management-children (accessed on 25 February 2025).
- Wardrope, A.; Dworetzky, B.A.; Barkley, G.L.; Baslet, G.; Buchhalter, J.; Doss, J.; Goldstein, L.H.; Hallett, M.; Kozlowska, K.; LaFrance, W.C., Jr.; et al. How to do things with words: Two seminars on the naming of functional (psychogenic, non-epileptic, dissociative, conversion, …) seizures. Seizure 2021, 93, 102–110. [Google Scholar] [CrossRef]
- Tate, R.L.; Perdices, M.; Rosenkoetter, U.; McDonald, S.; Togher, L.; Shadish, W.; Horner, R.; Kratochwill, T.; Barlow, D.H.; Kazdin, A.; et al. The Single-Case Reporting guideline In BEhavioural interventions (SCRIBE) 2016: Explanation and elaboration. Arch. Sci. Psychol. 2016, 4, 10–31. [Google Scholar] [CrossRef]
- Ma, H.-H. An alternative method for quantitative synthesis of single-subject: Percentage of data points exceeding the median. Behav. Modif. 2006, 30, 598–617. [Google Scholar] [CrossRef] [PubMed]
- Parker, R.I.; Hagan-Burke, S.; Vannest, K. Percentage of All Non-overlapping Data (PAND): An alternative to PND. J. Spec. Educ. 2007, 40, 194–204. [Google Scholar] [CrossRef]
- Parker, R.I.; Vannest, K. An improved effect size for single-case research: Nonoverlap of All Pairs. Behav. Ther. 2009, 40, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Scruggs, T.E.; Mastropieri, M.A. Summarizing single-subject research: Issues and Applications. Behav. Modif. 1998, 22, 221–242. [Google Scholar] [CrossRef]
- Jacobson, N.S.; Truax, P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 1991, 59, 12–19. [Google Scholar] [CrossRef]
- Carlson, E.B.; Putnam, F.W. An update on the Dissociative Experiences Scale. Dissociation Prog. Dissociative Disord. 1993, 6, 16–27. [Google Scholar]
- Van Ijzendoorn, M.H.; Schuengel, C. The measurement of dissociation in normal and clinical populations: Meta-analytic validation of the Dissociative Experiences Scale (DES). Clin. Psychol. Rev. 1996, 16, 365–382. [Google Scholar] [CrossRef]
- Chorpita, B.F.; Moffitt, C.E.; Gray, J. Psychometric properties of the Revised Child Anxiety and Depression Scale in a clinical sample. Behav. Res. Ther. 2005, 43, 309–322. [Google Scholar] [CrossRef]
- Twigg, E.; Cooper, M.; Evans, C.; Freire, E.; Mellor-Clark, J.; McInnes, B.; Barkham, M. Acceptability, reliability, referential distributions and sensitivity to change in the Young Person’s Clinical Outcomes in Routine Evaluation (YP-CORE) outcome measure: Replication and refinement. Child Adolesc. Ment. Health 2016, 21, 115–123. [Google Scholar] [CrossRef]
- Duncan, B.L.; Miller, S.D.; Sparks, J.A.; Claud, D.A.; Reynolds, L.R.; Brown, J.; Jhonson, L.D. The Session Rating Scale: Preliminary psychometric properties of a “working” alliance measure. J. Brief Ther. 2003, 3, 3–12. [Google Scholar]
- Murphy, M.G.; Rakes, S.; Harris, R.M. The psychometric properties of the Session Rating Scale: A narrative review. J. Evid.-Based Soc. Work. 2020, 17, 279–299. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, B.; Elliott, R. Qualitative methods in psychotherapy outcome research. In Psychotherapy Research; Gelo, O., Pritz, A., Rieken, B., Eds.; Springer: Vienna, Austria, 2015; pp. 559–578. [Google Scholar] [CrossRef]
- Elliott, R. Qualitative methods for studying psychotherapy change processes. In Qualitative Research Methods in Mental Health and Psychotherapy: A Guide for Students and Practitioners; Harper, D., Thompson, A.R., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2012; pp. 69–81. [Google Scholar] [CrossRef]
- Hallam, C.; Simmonds-Buckley, M.; Kellett, S.; Greenhill, B.; Jones, A. The acceptability, effectiveness, and durability of Cognitive Analytic Therapy: Systematic review and meta-analysis. Psychol. Psychother. Theory Res. Pract. 2021, 94, 8–35. [Google Scholar] [CrossRef] [PubMed]
- Simmonds-Buckley, M.; Osivwemu, E.-O.; Kellett, S.; Taylor, C. The acceptability of Cognitive Analytic Therapy (CAT): Meta-analysis and benchmarking of treatment refusal and treatment dropout rates. Clin. Psychol. Rev. 2022, 96, 102187. [Google Scholar] [CrossRef]
- Kellett, S. The treatment of Dissociative Identity Disorder with Cognitive Analytic Therapy: Experimental evidence of sudden gains. J. Trauma Dissociation 2005, 6, 55–81. [Google Scholar] [CrossRef]
- Wildgoose, A.; Clarke, S.; Waller, G. Treating personality fragmentation and dissociation in Borderline Personality Disorder: A pilot study of the impact of Cognitive Analytic Therapy. Br. J. Med. Psychol. 2001, 74, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Bearman, N. Cognitive analytic therapy and functional neurological disorders. Int. J. Cogn. Anal. Ther. Relational Ment. Health 2019, 3, 35–50. [Google Scholar]
- Ludwig, L.; Pasman, J.A.; Nicholson, T.; Aybek, S.; David, A.S.; Tuck, S.; Kanaan, R.A.; Roelofs, K.; Carson, A.; Stone, J. Stressful life events and maltreatment in Conversion (functional neurological) Disorder: Systematic review and meta-analysis of case-control studies. Lancet Psychiatry 2018, 5, 307–320. [Google Scholar] [CrossRef]
- Parry, G.; Bennett, D.; Roth, A.D.; Kellett, S. Developing a competence framework for Cognitive Analytic Therapy. Psychol. Psychother. Theory Res. Pract. 2021, 94, 151–170. [Google Scholar] [CrossRef]
- Kellett, S.; Young, A.D.; Hepple, J.; White, S. Eight session CAT: The evidence and the approach. In The Oxford Handbook of Cognitive Analytic Therapy; Brummer, L., Cavieres, M., Tan, R., Eds.; Oxford University Press: Oxford, UK, 2024; pp. 248–262. [Google Scholar] [CrossRef]
- Taylor, P.J.; Adeyemi, I.; Marlow, K.; Cottam, S.; Airnes, Z.; Hartley, S.; Howells, V.; Dunn, B.D.; Elliott, R.A.; Hann, M.; et al. The Relational Approach to Treating Self-Harm (RELATE): Study protocol for a feasibility randomised controlled trial study of Cognitive Analytic Therapy for adults who self-harm versus treatment at usual. Pilot Feasibility Stud. 2024, 10, 101. [Google Scholar] [CrossRef]
- Kazdin, A.E. Methodological and interpretive problems of single-case experimental designs. J. Consult. Clin. Psychol. 1978, 46, 629–642. [Google Scholar] [CrossRef]
- de Haan, A.M.; Boon, A.E.; de Jong, J.T.V.M.; Hoeve, M.; Vermeiren, R.R.J.M. A Meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clin. Psychol. Rev. 2013, 33, 698–711. [Google Scholar] [CrossRef] [PubMed]
- Ebesutani, C.; Chorpita, B.F.; Higa-McMillan, C.K.; Nakamura, B.J.; Regan, J.; Lynch, R.E. A psychometric analysis of the Revised Child Anxiety and Depression Scales--parent version in a school sample. J. Abnorm. Child Psychol. 2011, 39, 173–185. [Google Scholar] [CrossRef] [PubMed]
- Kellett, S.; Gausden, J.; Gaskell, C. The effectiveness of Cognitive Analytic Therapy for Borderline Personality Disorder: Utilizing a withdrawal experimental design to improve sensitivity to abandonment. Psychol. Psychother. Theory Res. Pract. 2020, 94, 96–119. [Google Scholar] [CrossRef] [PubMed]
- Krasny-Pacini, A.; Evans, J. Single-case experimental designs to assess intervention effectiveness in rehabilitation: A practical guide. Ann. Phys. Rehabil. Med. 2018, 61, 164–179. [Google Scholar] [CrossRef]
- Armstrong, J.G.; Putnam, F.W.; Carlson, E.B.; Libero, D.Z.; Smith, S.R. Development and validation of a measure of adolescent dissociation: The Adolescent Dissociative Experiences Scale. J. Nerv. Ment. Dis. 1997, 185, 491–497. [Google Scholar] [CrossRef]
- Bennett, D.; Parry, G. A measure of psychotherapeutic competence derived from Cognitive Analytic Therapy. Psychother. Res. 2004, 14, 176–192. [Google Scholar] [CrossRef]
- Kenward, M.G.; Jones, B. Crossover trials. In Methods and Applications of Statistics in Clinical Trials: Concepts, Principles, Trials, and Design; Balakrishnan, N., Ed.; John Wiley & Sons: Hoboken, NJ, USA, 2014; Volume 1, pp. 310–319. [Google Scholar] [CrossRef]

| Session 1 (Reformulation A SCED Phase) | Session 2 (Reformulation A SCED Phase) | Session 3 (Recognition B SCED Phase) | Session 4 (Recognition B SCED Phase) | Session 5 (Recognition B SCED Phase) | Session 6 (Revision C SCED Phase) | Session 7 (Revision C SCED Phase) | Session 8 (Revision C SCED Phase) | Follow-Up (Revision) |
|---|---|---|---|---|---|---|---|---|
| SRS | SRS | SRS | SRS | SRS | SRS | SRS | SRS | SRS |
| YP-CORE | YP-CORE | YP-CORE | YP-CORE | YP-CORE | YP-CORE | YP-CORE | YP-CORE | YP-CORE |
| DES-II | DES-II | DES-II | ||||||
| R-CADS | R-CADS | R-CADS | ||||||
| TP/TPP recognition rating | TP/TPP recognition rating | TP/TPP recognition rating | TP/TPP recognition rating | TP/TPP recognition rating | TP/TPP recognition rating | TP/TPP recognition rating | TP/TPP recognition rating | TP/TPP recognition rating |
| TP/TPP recognition rating | TP/TPP recognition rating | TP/TPP recognition rating | TP/TPP recognition rating | TP/TPP recognition rating | TP/TPP recognition rating | TP/TPP recognition rating | TP/TPP recognition rating | TP/TPP recognition rating |
| qualitative: change interview conducted 13 weeks after CAT completion |
| NAP (95% CI) | PAND | PND | PEM | |
|---|---|---|---|---|
| Reformulation (A) vs. Recognition (B) | ||||
| Self-Esteem—Recognition | 100% (100% to 100%) | 100% | 100% | 100% |
| Self-Esteem—Revision | 100% (100% to 100%) | 100% | 100% | 100% |
| Over-Regulate—Recognition | 17% (2% to 69%) | 60% 60 | 0% | 33% |
| Over-Regulate—Revision | 58% (17% to 90%) | 60% | 33% | 50% |
| Reformulation (A) vs. Revision (C) | ||||
| Self-Esteem—Recognition | 100% (100% to 100%) | 100% | 100% | 100% |
| Self-Esteem—Revision | 100% (100% to 100%) | 100% | 100% | 100% |
| Over-Regulate—Recognition | 67% (21% to 93%) | 80% | 67% | 67% |
| Over-Regulate—Revision | 100% (100% to 100%) | 100% | 100% | 100% |
| Reformulation (A) vs. Follow-Up (FU) | ||||
| Self-Esteem—Recognition | 100% (100% to 100%) | 100% | 100% | 100% |
| Self-Esteem—Revision | 0% (0% to 0%) | 67% | 0% | 0% |
| Over-Regulate—Recognition | 50% (8% to 92%) | 67% | 0% | 0% |
| Over-Regulate—Revision | 25% (2% to 84%) | 67% | 0% | 0% |
| Recognition (B) vs. Follow-Up (FU) | ||||
| Self-Esteem—Recognition | 33% (4% to 85%) | 75% | 0% | 0% |
| Self-Esteem—Revision | 100% (100% to 100%) | 100% | 100% | 100% |
| Over-Regulate—Recognition | 33% (4% to 85%) | 75% | 0% | 0% |
| Over-Regulate—Revision | 83% (23% to 99%) | 75% | 0% | 100% |
| Description of Personal Changes | Change Was: 1—Expected by Me, 2—Somewhat Expected by Me, 3—Neither Expected or Surprising, 4—I Was Somewhat Surprised, 5—I Was Very Surprised by. | Importance of This Change to Me: 1—Not at All, 2—Slightly, 3—Moderately, 4—Very, 5—Extremely. | Ability to Apply This Change in Everyday Life: 1—Can’t Apply, 2—Can Somewhat Apply, 3—Can Apply Some Aspects, 4—Can Apply Most Aspects, 5—Can Apply All Aspects. | Likelihood of This Change Without Therapy 1—Very Unlikely, 2—Somewhat Unlikely, 3—Neither, 4—Somewhat Likely, 5—Likely. |
|---|---|---|---|---|
| No seizures for two months | 4 | 5 | 5 | 1 |
| Stopped ‘exploding’ emotionally and feel calmer | 1 | 4 | 3 | 2 |
| Taking more time to be with self and not constantly needing to be around people | 4 | 5 | 4 | 3 |
| Better model of relationships | 2 | 4 | 4 | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Horan, A.; Kellett, S.; Gaskell, C.; Morris, C. Cognitive Analytic Therapy for Functional/Dissociative Seizures in an Adolescent: Case Report and Mixed-Methods Single-Case Evaluation. Reports 2025, 8, 93. https://doi.org/10.3390/reports8020093
Horan A, Kellett S, Gaskell C, Morris C. Cognitive Analytic Therapy for Functional/Dissociative Seizures in an Adolescent: Case Report and Mixed-Methods Single-Case Evaluation. Reports. 2025; 8(2):93. https://doi.org/10.3390/reports8020093
Chicago/Turabian StyleHoran, Andrew, Stephen Kellett, Chris Gaskell, and Conor Morris. 2025. "Cognitive Analytic Therapy for Functional/Dissociative Seizures in an Adolescent: Case Report and Mixed-Methods Single-Case Evaluation" Reports 8, no. 2: 93. https://doi.org/10.3390/reports8020093
APA StyleHoran, A., Kellett, S., Gaskell, C., & Morris, C. (2025). Cognitive Analytic Therapy for Functional/Dissociative Seizures in an Adolescent: Case Report and Mixed-Methods Single-Case Evaluation. Reports, 8(2), 93. https://doi.org/10.3390/reports8020093






