Abstract
Background and Clinical Significance: Gastrointestinal bleeding is a critical medical emergency, with upper gastrointestinal bleeding occurring approximately five times more frequently than lower gastrointestinal bleeding (LGIB). The incidence of LGIB tends to increase with age, likely due to a greater prevalence of vascular and diverticular diseases among older patients. However, there are rare or extremely rare causes of LGIB that demand significant diagnostic and therapeutic efforts, some of which may pose unexpected challenges during surgery. Case report: We present the case of a 75-year-old woman, previously treated for a cecal neoplasm 15 years ago, who was hospitalized due to intermittent lower gastrointestinal bleeding over the past three months. Initially, the patient declined a colonoscopic examination, and the bleeding stopped spontaneously. She was then discharged at her own request in stable condition. However, she returned with a recurrence of the bleeding. While preparing for a colonoscopy, she experienced subocclusive symptoms, abdominal distension, and vomiting. During emergency surgery, a floating coprolith, which was attached to one of the anastomosis sutures, was sensed through palpation and later confirmed via colotomy. The coprolith was removed, and hemostasis was achieved in situ, leading to a favorable postoperative recovery and normalization of intestinal transit. A literature review identified 24 articles that met the eligibility criteria concerning rare causes of LGIB. Appendiceal bleeding (due to erosions, arteriovenous malformations, or endometriosis) was the most common cause, whereas the rarest causes included jejunal hemangiomas and rectal ulcers resulting from mucormycosis. Diagnosing these conditions is often challenging, typically requiring CT scans, colonoscopy, and angiography, with surgical treatment being the primary method to ensure hemostasis. In conclusion, the diagnosis and management of LGIB present significant challenges for clinicians, and successful outcomes are usually achieved through a collaborative multidisciplinary team approach.
1. Introduction and Clinical Significance
Lower gastrointestinal bleeding (LGIB) is a significant pathology in emergency admissions, accounting for approximately 30–40% of all gastrointestinal bleeding cases in the USA [1,2]. The most common causes of LGIB, in order of prevalence, include diverticular disease, angiodysplasia, ischemic colitis, colorectal neoplasms, hemorrhoidal disease, bleeding after polypectomy, post-radiotherapy enteritis, and gastrointestinal inflammatory disease [3,4]. Less common causes encompass colorectal varices, intussusception, Meckel’s diverticulum, and aortoenteric fistula [3,4].
The mortality rate in people with LGIB is 2.4–3.9% and can reach 40% in elderly patients with multiple associated comorbidities [5].
This has led to ongoing concerns about accurately diagnosing the cause of GI bleeding, particularly when selecting the appropriate treatment. In the early 1900s, the diagnosis and treatment of LGIB were almost exclusively the responsibility of surgeons. However, gastroenterologists have become increasingly involved with the introduction of diagnostic and interventional endoscopic procedures. Today, in addition to endoscopic techniques, new treatment methods have emerged, including those from interventional radiology and nuclear medicine, while surgery remains a last resort when other methods are no longer effective [5,6,7,8,9]. The diverse array of diagnostic and treatment options has led to a tailored approach for managing LGIB patients, especially concerning treatment and diagnosis [10]. Despite the significant advancements that have been made in recent years, the diagnosis and treatment of LGIB continue to spark various controversies, primarily due to the unusual or extremely rare causes of these hemorrhages. Such cases necessitate close collaboration among multidisciplinary medical teams, including ICU staff, gastroenterologists, radiologists, and surgeons, to accurately establish the diagnosis and the most appropriate treatment strategy.
2. Case Presentation
A 75-year-old female patient was referred to the General Surgery Clinic of Dr. Carol Davila Nephrology Hospital in Bucharest due to the appearance of bloody stools two days prior to admission.
The patient was hemodynamically stable but presented with anemia (hemoglobin 10.2 g/dL), hypoalbuminemia, and hypoproteinemia. All other laboratory test values were normal.
Upon admission, the patient was in poor general condition, had a pale complexion, and exhibited a soft, painless abdomen with stools that appeared reddish-burgundy. She has a history of cecal neoplasm, which was surgically treated 15 years ago (right hemicolectomy with manual anastomosis), followed by six chemotherapy sessions, and was declared cured after five years of oncological follow-up (documents unavailable). There are no chronic illnesses, and she is not receiving any chronic treatment. Over the past three months, she has experienced abdominal discomfort characterized by distention and intermittent colicky pain, accompanied by diarrhea. She has had 2–3 episodes of rectorrhea, which were self-limiting. The current episode started 2 days ago, with repeated stools (3–4 times a day) exhibiting a bloody, vein-like appearance. She was admitted for diagnostic and therapeutic management.
Because the patient’s history includes a right hemicolectomy with ileo-transverse manual termino-lateral anastomosis for cecal neoplasm, performed 15 years ago, tumor markers CA 19-9 and carcinoembryonic antigen—both of which showed normal results—were also collected. According to the patient’s reports, not every stool was bloody, and the last stool was no longer red. After admission, the next stool appeared normal, and the patient was advised to start a digestive preparation for colonoscopy, which she refused. During the hospitalization (5 days inpatient), the patient’s stool remained normal, leading to the conclusion.
According to the patient’s reports, not every stool was bloody, and the last stool was no longer red. After admission, the next stool appeared normal, and the patient was advised to start a digestive preparation for the colonoscopy, which she refused. During the hospitalization of five days, the stool remained normal, leading to the conclusion that the bleeding stopped spontaneously, as is common in many cases of LGIB.
After approximately three months, the patient returned to our clinic, again presenting with bloody stools and hematochezia. This time, the hemoglobin level was lower (8.7 g/dL), and the patient was admitted to the ICU with hypotension (blood pressure 80 mmHg). Upon clinical examination, there was moderate abdominal distension but no pain. A rectal exam revealed traces of red blood on the glove. Hydroelectrolyte rebalancing treatment was initiated, to which the patient responded positively. The patient was again recommended to undergo colonoscopy after appropriate bowel preparation; this time, she accepted.
During the digestive preparation, the patient experienced nausea and vomiting, which interrupted the ingestion of the purgative solution. As in the previous admission, the stool color normalized the following day. To establish a diagnosis, a computerized tomography (CT) examination with angiographic timing was recommended to identify the bleeding site.
During the CT examination, it was not possible to determine the source of the hemorrhage, since the digestive bleeding had ceased. However, a 1.5 cm foreign body was observed in the colon (right iliac fossa) along with multiple hydroaeric images (Figure 1).
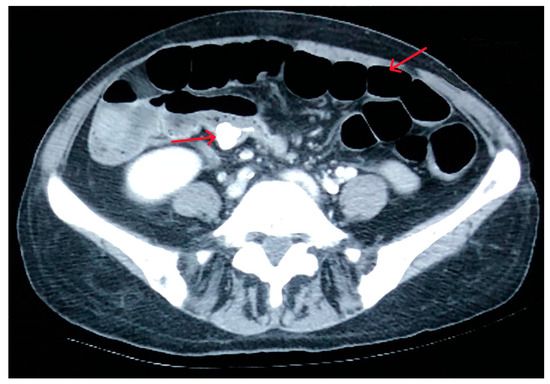
Figure 1.
CT image with the foreign body (left arrow) and hydroaeric images (right arrow).
Later, the lower gastrointestinal hemorrhage resumed, resulting in stools with burgundy-colored blood and a 1 g/dL decrease in hemoglobin levels. In light of this situation, the decision was made to carry out an emergency surgical intervention to clarify the diagnosis and perform surgical hemostasis.
We performed surgery using an iterative median laparotomy and found a stenotic ileo-colic anastomosis accompanied by perianastomotic adhesions and dilated small bowel loops, with the colon appearing normal. Upon palpation, we detected a hard, approximately 2 cm floating mass within the colon. A colotomy was executed, focusing on the foreign body. Intraoperatively, we were surprised to identify the foreign body, as shown in the CT scan, located within the colonic lumen next to the ileocolic anastomosis, floating a few centimeters between the transverse colon and the terminal ileum.
At the same time, the ileocolic anastomosis was entangled in a perianastomotic adhesion process that partially twisted it, which explained the hydroaeric levels noted in the CT scan and the challenges in preparing the colon for the colonoscopic examination.
The foreign body was removed through colotomy and consisted of a coprolith attached to one of the sutures used for the anastomosis (silk thread) (Image 2). The mucosa of the colon and terminal ileum showed numerous erosions covered with blood clots, though there was no active bleeding during the surgery (biopsies taken). The histopathological findings are as follows: the pathological material includes multiple fragments of colonic mucosa with preserved morphology and mucous secretion, accompanied by significant lymphoplasmacytic inflammatory infiltration distributed both diffusely and in follicular lymphoid aggregates. No signs indicating malignancy were found.
Thus, the source of the digestive bleeding was identified, and definitive hemostasis was achieved by applying in situ hemostasis threads—polysorb. No 3/0 (Figure 2).

Figure 2.
Coprolith attached to the suture thread.
The patient’s postoperative recovery was positive, with digestive tolerance and bowel movement resuming by day 4. There were no signs of recurring lower gastrointestinal bleeding or obstruction. We followed up with the patient 5 years postoperatively and she was without signs of digestive disorder. Essentially, we viewed this case as a late complication of the postoperative period, with no indicators of neoplastic recurrence, resulting from the formation of a coprolith that eroded the intestinal mucosa and led to repeated bleeding.
3. Literature Review
We conducted a literature review by searching the following databases: PubMed, PubMed Central, Google Scholar, and Cochrane according to the following criteria: “rare” [All Fields] AND (“etiology” [Subheading] OR “etiology” [All Fields] OR “causes” [All Fields] OR “causality” [MeSH Terms] OR “causality” [All Fields]) AND lower [All Fields] AND (“gastrointestinal hemorrhage” [MeSH Terms] OR (“gastrointestinal” [All Fields] AND “hemorrhage” [All Fields]) OR “gastrointestinal hemorrhage” [All Fields] OR (“gastrointestinal” [All Fields] AND “bleeding” [All Fields]) OR “gastrointestinal bleeding” [All Fields]).
The search yielded 35,608 articles. The study took place from 15 October 2024 to 15 February 2025.
After the initial search, which produced a vast number of results (35,608), we attempted to refine it using the LGIB criteria and obtained 3247 results. The criteria remained the same, focusing on “lower gastrointestinal bleeding” while excluding “gastrointestinal hemorrhage”. It became apparent that some articles previously included in the review were no longer available, significantly decreasing the pool of eligible articles. Consequently, we decided to perform the narrative literature review following the first search.
The inclusion criteria were as follows: English full-text articles, case reports, and reports of rare causes of lower gastrointestinal bleeding. We excluded articles for which only abstracts were available, those not written in English, and studies that covered other digestive bleeding causes.
The criteria for inclusion and exclusion specified that articles must be in English, involve patients over 18 years of age, report on rare causes of LGIB, and include case presentations or series of cases.
4. Discussion
Only 24 articles meeting the eligibility criteria were identified [11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34].
Unexpectedly, the most frequently reported rare cases of LGIB involved appendiceal bleeding. We found 11 cases with various causes: mucosal erosion (4), arteriovenous malformation (3), and 1 case each of diverticula of the appendix, appendicular stump after appendectomy, appendicular endometriosis, and Dieulafoi’s lesion of the appendix. The diagnosis was established in most cases via colonoscopy; CT was rarely needed (2 cases). Even when appendiceal bleeding was confirmed colonoscopically, the final diagnosis was made through a pathological examination of the appendix following appendectomy. Laparoscopic appendectomy was the definitive treatment (unitary in all cases), although in two cases, endoscopic clipping was attempted [13,14,17,18,19,30,31].
Other rare causes of LGIB included anorectal hemangioma (3), colonic varices (2), colonic amyloidosis, Osler Rendu syndrome, jejunal hemangioma, Kasabach–Merrit syndrome, lung adenocarcinoma metastasis in the colon, inflammatory cloacogenic polyp mimicking rectal cancer, caecum lipoma, and rectal ulcer induced by mucormycosis. For diagnosing these rare causes of LGIB, the entire available arsenal was utilized: colonoscopy, CT, and angiography. In most cases, it was necessary to combine diagnostic methods to reach the final diagnosis—Colonoscopy + CT(5), Colonoscopy + Angiography(6), Colonoscopy + CT + Angiography (2). Thus, personalized treatment was tailored to the diagnosis of each case, with most requiring surgery (7), colonoscopic (3), and angiographic (1) hemostasis [15,16,20,21,22,23,24,25,26,27,28,29,34].
Most authors suggest utilizing the full range of diagnostic tools to establish the most accurate diagnosis, thereby ensuring the appropriate choice of treatment [14,17,20,21,22,23,24,27,31,32,34].
5. Conclusions
Rare causes of LGIB continue to present a significant challenge for clinicians, and establishing an accurate diagnosis requires a multidisciplinary team to ensure effective personalized treatment.
Author Contributions
Conceptualization, C.I. and C.R.I.; methodology, C.I. and C.R.I.; formal analysis, C.I. and C.R.I.; investigation C.I.; review C.I.; writing—original draft preparation C.I. and C.R.I.; writing—review and editing, C.I. and C.R.I.; visualization, C.I. and C.R.I.; supervision, C.R.I.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki. Ethical review and approval of this study—No. 85/17.02.2025 by the Ethics Committee of Dr. Carol Davila Clinical Nephrology Hospital.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Acknowledgments
The authors have reviewed and edited the output and take full responsibility for the content of this publication.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| CT | Computed tomography. |
| ICU | Intensive Care Unit. |
| GI | Gastrointestinal. |
| LGIB | Lower gastrointestinal bleeding. |
References
- Peery, A.F.; Crockett, S.D.; Barritt, A.S.; Dellon, E.S.; Eluri, S.; Gangarosa, L.M.; Jensen, E.T.; Lund, J.L.; Pasricha, S.; Runge, T.; et al. Burden of Gastrointestinal, Liver, and Pancreatic Diseases in the United States. Gastroenterology 2015, 149, 1731–1741.e3. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Laine, L.; Yang, H.; Chang, S.C.; Datto, C. Trends for incidence of hospitalization and death due to GI complications in the United States from 2001 to 2009. Am. J. Gastroenterol. 2012, 107, 1190–1195. [Google Scholar] [CrossRef] [PubMed]
- Frost, J.; Sheldon, F.; Kurup, A.; Disney, B.R.; Latif, S.; Ishaq, S. An approach to acute lower gastrointestinal bleeding. Frontline Gastroenterol. 2017, 8, 174–182. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Strate, L.L.; Ayanian, J.Z.; Kotler, G.; Syngal, S. Risk factors for mortality in lower intestinal bleeding. Clin. Gastroenterol. Hepatol. 2008, 6, 1004–1010. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Serur, A.; Rhee, R.; Ramjist, J. Current Nonoperative Therapeutic Interventions for Lower Gastrointestinal Hemorrhage. Clin. Colon. Rectal Surg. 2020, 33, 22–27. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Judd, E.S.; Pollock, L.W. DIVERTICULITIS OF THE COLON. Ann. Surg. 1924, 80, 425–438. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Smith, W.R.; Berne, C.J. SEVERE COLONIC BLEEDING. Calif. Med. 1964, 101, 235–239. [Google Scholar] [PubMed] [PubMed Central]
- Whitlow, C.B. Endoscopic treatment for lower gastrointestinal bleeding. Clin. Colon. Rectal Surg. 2010, 23, 31–36. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Adegboyega, T.; Rivadeneira, D. Lower GI Bleeding: An Update on Incidences and Causes. Clin. Colon. Rectal Surg. 2020, 33, 28–34. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cerruti, T.; Maillard, M.H.; Hugli, O. Acute Lower Gastrointestinal Bleeding in an Emergency Department and Performance of the SHA2PE Score: A Retrospective Observational Study. J. Clin. Med. 2021, 10, 5476. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fernandes, A.; Ferreira, A.M.; Serra, P.; Carvalho, L. Intestinal ganglioneuromatosis: An unusual aetiology for occult gastrointestinal bleeding. BMJ Case Rep. 2015, 2015, bcr2015211764. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pyakurel, S.; Bohara, S.; Bhattarai, S.; Regmi, S.; Karki, S.; Adhikari, M.; Gurung, B.; Shrestha, U. Osler-Weber-Rendu syndrome: A case report on a rare vascular malformation presented with lower gastrointestinal bleeding. Clin. Case Rep. 2023, 11, e6965. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Murakami, D.; Harada, H.; Amano, Y. An unexpected cause of lower gastrointestinal bleeding. Clin. Case Rep. 2020, 9, 586–587. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Waleed, M.; Ali, A.M.; Saraj, O.; Babu, S.; Morgan, R. A rare cause of lower GI bleeding. BMJ Case Rep. 2012, 2012, bcr0320126086. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pospisilova, B.; Frydrych, J.; Krajina, A.; Örhalmi, J.; Kajzrlikova, I.M.; Vitek, P. Anorectal hemangioma, a rare cause of lower gastrointestinal bleeding, treated with selective embolization: A case report. World J. Gastrointest. Surg. 2024, 16, 2735–2741. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kitagawa, S.; Sato, T.; Hirayama, A. Colonic Varices Due to Chronic Pancreatitis: A Rare Cause of Lower Gastrointestinal Bleeding. ACG Case Rep. J. 2015, 2, 168–170. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Khan, F.; Lu, S.; Parajuli, D. A Rare Cause of Massive Hematochezia: Arteriovenous Malformation of the Appendix. ACG Case Rep. J. 2021, 8, e00679. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vesa, T.S.; Hosseini-Carroll, P.; Manas, K. Diverticular hemorrhage of the appendix. Gastroenterol. Hepatol. 2014, 10, 394–395. [Google Scholar] [PubMed] [PubMed Central]
- Kecmanovic, D.M.; Bulajic, M.M.; Pavlov, M.J.; Micev, M.T.; Sepetkovski, A.V.; Ceranic, M.S.; Petrovic, M.N.; Stamenkovic, A.B. Recurrent rectal bleeding from an appendiceal stump granuloma: A rare late complication of appendectomy. Endoscopy. 2005, 37, 1161. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pérez, J.S.; Cintrón, D.; Deyá-Quinquilla, A.; Molina, J.; Pagán, V.B.; Vargas-Otero, P.; Rivera, E.; Tirado-Gómez, M.; Pacheco, E.; Costas, P. Lower Gastrointestinal Bleeding Because of Kasabach-Merritt Syndrome Showing an Impressive Response to Sirolimus. ACG Case Rep. J. 2022, 9, e00688. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Abdulghaffar, S.; AlMulla, M.; AlNuaimi, D.; AlKetbi, R.; Khairi, T.E. A rectosigmoid haemangioma: A rare etiology of rectal bleeding. BJR Case Rep. 2022, 8, 20220084. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Papanikolaou, I.S.; Gkolfakis, P.; Tziatzios, G.; Grammatikos, K.; Panayiotides, I.G.; Tsakiraki, Z.; Zinovieva, I.; Dimitriadis, G.D.; Triantafyllou, K. An unusual cause of acute lower gastrointestinal bleeding: Lung adenocarcinoma metastasis to the descending colon. Clin. Case Rep. 2017, 5, 1411–1413. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- El Eulj, O.; Koulali, H.; El Mqaddem, O.; Ismaili, Z.; Kharrasse, G. A rare cause of rectal bleeding in a 48-year-old lupus patient. Radiol. Case Rep. 2023, 19, 315–318. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cheng, H.H.; Chen, T.W.; Chou, J.W. A rare cause of rectal bleeding. Turk. J. Gastroenterol. 2019, 30, 984–985. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kóder, G.; Dinya, T.; Tóth, D.; Damjanovich, L.; Ágoston, L.; Tanyi, M. Rare case of successfully operated idiopathic colonic varicosity. Int. J. Surg. Case Rep. 2024, 123, 110196. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Martinez-Mier, G.; Ortiz-Bayliss, A.B.; Alvarado-Arenas, R.; Carrasco-Arroniz, M.A. Caecum lipoma: A rare cause of lower gastrointestinal bleeding. BMJ Case Rep. 2014, 2014, bcr2014206526. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chiang, T.H.; Lee, Y.W.; Tan, J.H.; Kao, C.C.; Chang, C.C.; Fang, K.C. Mucormycosis causing massive lower gastrointestinal bleeding: A case report. BMC Gastroenterol. 2021, 21, 272. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Khalid, A.; Abdelrahman, H.; Ali, S.M.; Latif, E.A.; Al-Thani, H.; El-Menyar, A. Dieulafoy’s Lesion of the Anal Canal: A Rare Cause of Lower Gastrointestinal Bleeding. Am. J. Case Rep. 2017, 18, 677–681. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hui, Y.Y.; Zhu, L.P.; Yang, B.; Zhang, Z.Y.; Zhang, Y.J.; Chen, X.; Wang, B.M. Gastrointestinal bleeding caused by jejunal angiosarcoma: A case report. World J. Clin. Cases. 2020, 8, 4565–4571. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhou, S.Y.; Guo, M.D.; Ye, X.H. Appendiceal bleeding: A case report. World J. Clin. Cases. 2022, 10, 6314–6318. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chung, K.S.; Gao, J.P. Massive lower gastrointestinal bleeding from the appendix. Gut Liver. 2011, 5, 234–237. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ma, Q.; Du, J.J. Appendiceal bleeding caused by vascular malformation: A case report. World J. Clin. Cases. 2024, 12, 2457–2462. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Baek, S.K.; Kim, Y.H.; Kim, S.P. Acute lower gastrointestinal bleeding due to appendiceal mucosal erosion. Surg. Laparosc. Endosc. Percutan Tech. 2010, 20, e110–e113. [Google Scholar] [CrossRef] [PubMed]
- de Santana Neto, W.B.; Neto, G.T.; da Cunhaa, C.M.Q.; Brasil, A.C.; Feitosa, J.N.P. Anorectal hemangioma—differential diagnosis of anal bleeding. J. Coloproctol. 2017, 37, 44–46. [Google Scholar] [CrossRef][Green Version]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).