Integrating Telerehabilitation into the Prehabilitation and Rehabilitation Pathway in Colorectal Cancer: A Case Series
Abstract
1. Introduction and Clinical Significance
2. Case Presentation
2.1. Eligibility Criteria
2.2. Cases Characteristics
2.3. Procedure
2.4. Intervention
2.5. Outcomes
2.5.1. Primary Outcome
2.5.2. Secondary Outcomes
Body Composition
Muscle Strength
Quality of Life EuroQol 5D
2.6. Results
Postoperative Complications and Safety Monitoring
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CRC | Colorectal Cancer |
| WHO | World Health Organization |
| QoL | Quality of Life |
| ERAS | Enhanced Recovery After Surgery |
| ASA | American Society of Anaesthesiologists |
| BMI | Body Mass Index |
| 6MWT | Six-Minute Walk Test |
| ATS | American Thoracic Society |
| ERS | European Respiratory Society |
| BIA | Bioelectrical Impedance Analysis |
| HGS | Handgrip Strength Test |
| 5R-STS | Five-Repetition Sit-to-Stand Test |
| MAC | Mental Adjustment to Cancer |
| HADS | Hospital Anxiety and Depression Scale |
| HRQoL | Health-Related Quality of Life |
| EQ-5D | EuroQol-5D |
| EQ-VAS | Visual Analogue Scale |
| T1 | Pre-prehabilitation |
| T2 | Post-prehabilitation |
| T3 | Pre-rehabilitation |
| T4 | Post-rehabilitation |
| T5 | Follow-up |
| FS | Fighting Spirit |
| AP | Anxious Preoccupation |
| FA | Fatalism |
| HH | Helplessness/Hopelessness |
| CA | Cognitive Avoidance |
| MDC | Minimum Detectable Change |
References
- Roshandel, G.; Ghasemi-Kebria, F.; Malekzadeh, R. Colorectal Cancer: Epidemiology, Risk Factors, and Prevention. Cancers 2024, 16, 1530. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Wagle, N.S.; Cercek, A.; Smith, R.A.; Jemal, A. Colorectal cancer statistics, 2023. CA A Cancer J. Clin. 2023, 73, 233–254. [Google Scholar] [CrossRef]
- Vainio, H.; Miller, A.B. Primary and Secondary Prevention in Colorectal Cancer. Acta Oncol. 2003, 42, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Geng, S.; Luo, H.; Wang, W.; Mo, Y.-Q.; Luo, Q.; Wang, L.; Song, G.-B.; Sheng, J.-P.; Xu, B. Signaling pathways involved in colorectal cancer: Pathogenesis and targeted therapy. Signal Transduct. Target. Ther. 2024, 9, 266. [Google Scholar] [CrossRef] [PubMed]
- Wheelwright, S.; Permyakova, N.V.; Calman, L.; Din, A.; Fenlon, D.; Richardson, A.; Sodergren, S.; Smith, P.W.F.; Winter, J.; Foster, C.; et al. Does quality of life return to pre-treatment levels five years after curative intent surgery for colorectal cancer? Evidence from the ColoREctal Wellbeing (CREW) study. PLoS ONE 2020, 15, e0231332. [Google Scholar] [CrossRef]
- Miyamoto, Y.; Hiyoshi, Y.; Tokunaga, R.; Akiyama, T.; Daitoku, N.; Sakamoto, Y.; Yoshida, N.; Baba, H. Postoperative complications are associated with poor survival outcome after curative resection for colorectal cancer: A propensity-score analysis. J. Surg. Oncol. 2020, 122, 344–349. [Google Scholar] [CrossRef]
- Bojesen, R.D.; Grube, C.; Buzquurz, F.; Miedzianogora, R.E.G.; Eriksen, J.R.; Gögenur, I. Effect of modifying high-risk factors and prehabilitation on the outcomes of colorectal cancer surgery: Controlled before and after study. BJS Open 2022, 6, zrac029. [Google Scholar] [CrossRef]
- Pak, H.; Maghsoudi, L.H.; Soltanian, A.; Gholami, F. Surgical complications in colorectal cancer patients. Ann. Med. Surg. 2020, 55, 13–18. [Google Scholar] [CrossRef]
- Waterland, J.L.; McCourt, O.; Edbrooke, L.; Granger, C.L.; Ismail, H.; Riedel, B.; Denehy, L. Efficacy of Prehabilitation Including Exercise on Postoperative Outcomes Following Abdominal Cancer Surgery: A Systematic Review and Meta-Analysis. Front. Surg. 2021, 8, 628848. [Google Scholar] [CrossRef]
- Stout, N.L.; Mina, D.S.; Lyons, K.D.; Robb, K.; Silver, J.K. A systematic review of rehabilitation and exercise recommendations in oncology guidelines. CA A Cancer J. Clin. 2021, 71, 149–175. [Google Scholar] [CrossRef]
- Clinical Practice Guidelines for the Prevention, Early Detection and Management of Colorectal Cancer||References n.d. Available online: https://app.magicapp.org/#/guideline/noPKwE (accessed on 30 March 2025).
- Molenaar, C.J.L.; Minnella, E.M.; Coca-Martinez, M.; Cate, D.W.G.T.; Regis, M.; Awasthi, R.; Martínez-Palli, G.; López-Baamonde, M.; Sebio-Garcia, R.; Feo, C.V.; et al. Effect of Multimodal Prehabilitation on Reducing Postoperative Complications and Enhancing Functional Capacity Following Colorectal Cancer Surgery: The PREHAB Randomized Clinical Trial. JAMA Surg. 2023, 158, 572–581. [Google Scholar] [CrossRef] [PubMed]
- Carli, F.; Bousquet-Dion, G.; Awasthi, R.; Elsherbini, N.; Liberman, S.; Boutros, M.; Stein, B.; Charlebois, P.; Ghitulescu, G.; Morin, N.; et al. Effect of Multimodal Prehabilitation vs. Postoperative Rehabilitation on 30-Day Postoperative Complications for Frail Patients Undergoing Resection of Colorectal Cancer: A Randomized Clinical Trial. JAMA Surg. 2020, 155, 233–242. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Amatya, B.; Malik, S.; Song, K.; Marcella, S.; Voutier, C.; Khan, F. Effectiveness of rehabilitation interventions in patients with colorectal cancer: An overview of systematic reviews. J. Rehabil. Med. 2025, 57, jrm40021. [Google Scholar] [CrossRef] [PubMed]
- Beyer, M.; Bischoff, C.; Lässing, J.; Gockel, I.; Falz, R. Effects of postoperative physical exercise rehabilitation on cardiorespiratory fitness, functional capacity and quality of life in patients with colorectal, breast, and prostate cancer—A systematic review and meta-analysis. J. Cancer Res. Clin. Oncol. 2025, 151, 13. [Google Scholar] [CrossRef]
- Trépanier, M.; Minnella, E.M.; Paradis, T.; Awasthi, R.; Kaneva, P.; Schwartzman, K.; Carli, F.; Fried, G.M.; Feldman, L.S.; Lee, L. Improved Disease-free Survival after Prehabilitation for Colorectal Cancer Surgery. Ann. Surg. 2019, 270, 493–501. [Google Scholar] [CrossRef]
- Bojesen, R.D.; Dalton, S.O.; Skou, S.T.; Jørgensen, L.B.; Walker, L.R.; Eriksen, J.R.; Grube, C.; Justesen, T.F.; Johansen, C.; Slooter, G.; et al. Preoperative multimodal prehabilitation before elective colorectal cancer surgery in patients with WHO performance status I or II: Randomized clinical trial. BJS Open 2023, 7, zrad134. [Google Scholar] [CrossRef]
- Choi, B.Y.; Bae, J.H.; Lee, C.S.; Han, S.R.; Lee, Y.S.; Lee, I.K. Implementation and improvement of Enhanced Recovery after Surgery protocols for colorectal cancer surgery. Ann. Surg. Treat. Res. 2022, 102, 223–233. [Google Scholar] [CrossRef]
- Peretti, A.; Amenta, F.; Tayebati, S.K.; Nittari, G.; Mahdi, S.S. Telerehabilitation: Review of the state-of-the-art and areas of application. JMIR Rehabil. Assist. Technol. 2017, 4, e7. [Google Scholar] [CrossRef]
- Winters, J.M. Telerehabilitation research: Emerging opportunities. Annu. Rev. Biomed. Eng. 2002, 4, 287–320. [Google Scholar] [CrossRef]
- Van Blarigan, E.L.; Chan, H.; Van Loon, K.; Kenfield, S.A.; Chan, J.M.; Mitchell, E.; Zhang, L.; Paciorek, A.; Joseph, G.; Laffan, A.; et al. Self-monitoring and reminder text messages to increase physical activity in colorectal cancer survivors (Smart Pace): A pilot randomized controlled trial. BMC Cancer 2019, 19, 218. [Google Scholar] [CrossRef]
- Dennett, A.; Harding, K.E.; Reimert, J.; Morris, R.; Parente, P.; Taylor, N.F. Telerehabilitation’s Safety, Feasibility, and Exercise Uptake in Cancer Survivors: Process Evaluation. JMIR Cancer 2021, 7, e33130. [Google Scholar] [CrossRef] [PubMed]
- Larson, J.L.; Rosen, A.B.; Wilson, F.A. The effect of telehealth interventions on quality of life of cancer survivors: A systematic review and meta-analysis. Health Inform. J. 2020, 26, 1060–1078. [Google Scholar] [CrossRef]
- Reese, C.; Weis, J.; Schmucker, D.; Mittag, O. Development of practice guidelines for psychological interventions in the rehabilitation of patients with oncological disease (breast, prostate, or colorectal cancer): Methods and results. Psycho-Oncology 2017, 26, 1513–1518. [Google Scholar] [CrossRef] [PubMed]
- Holland, A.E.; Spruit, M.A.; Troosters, T.; Puhan, M.A.; Pepin, V.; Saey, D.; McCormack, M.C.; Carlin, B.W.; Sciurba, F.C.; Pitta, F.; et al. An official european respiratory society/american thoracic society technical standard: Field walking tests in chronic respiratory disease. Eur. Respir. J. 2014, 44, 1428–1446. [Google Scholar] [CrossRef]
- Crapo, R.O.; Casaburi, R.; Coates, A.L.; Enright, P.L.; MacIntyre, N.R.; McKay, R.T.; Johnson, D.; Wanger, J.S.; Zeballos, R.J.; Bittner, V.; et al. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar]
- Schmidt, K.; Vogt, L.; Thiel, C.; Jäger, E.; Banzer, W. Validity of the six-minute walk test in cancer patients. Int. J. Sport Med. 2013, 34, 631–636. [Google Scholar] [CrossRef]
- Luz Alejandra Lorca, P.; Ribeiro, I.L.; Mónica Martínez, M.; Jorge Plasser, T.; Jessica Vivallos, G.; Roberto Salas, O. Functional results of a prehabilitation program in elective colorectal cancer surgery. Rev. Cir. 2022, 74, 276–282. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Crouch, R. Minimal clinically important difference for change in 6-minute walk test distance of adults with pathology: A systematic review. J. Eval. Clin. Pract. 2017, 23, 377–381. [Google Scholar] [CrossRef]
- Ræder, H.; Kværner, A.S.; Henriksen, C.; Florholmen, G.; Henriksen, H.B.; Bøhn, S.K.; Paur, I.; Smeland, S.; Blomhoff, R. Validity of bioelectrical impedance analysis in estimation of fat-free mass in colorectal cancer patients. Clin. Nutr. 2018, 37, 292–300. [Google Scholar] [CrossRef]
- Branco, M.G.; Mateus, C.; Capelas, M.L.; Pimenta, N.; Santos, T.; Mäkitie, A.; Ganhão-Arranhado, S.; Trabulo, C.; Ravasco, P. Bioelectrical Impedance Analysis (BIA) for the Assessment of Body Composition in Oncology: A Scoping Review. Nutrients 2023, 15, 4792. [Google Scholar] [CrossRef]
- Wang, N.; Khankari, N.K.; Cai, H.; Li, H.; Yang, G.; Gao, Y.; Xiang, Y.; Shu, X.; Zheng, W. Prediagnosis body mass index and waist–hip circumference ratio in association with colorectal cancer survival. Int. J. Cancer 2017, 140, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Godinho, L.; Ribeiro, G.; Lopez, E.; Deminice, R. Handgrip strength test vs. chair stand test: Divergent diagnosis of sarcopenia and its clinical implications in colorectal cancer. Clin. Nutr. ESPEN 2024, 63, 1068. [Google Scholar] [CrossRef]
- Bohannon, R.W. Minimal clinically important difference for grip strength: A systematic review. J. Phys. Ther. Sci. 2019, 31, 75–78. [Google Scholar] [CrossRef]
- Muñoz-Bermejo, L.; Adsuar, J.C.; Mendoza-Muñoz, M.; Barrios-Fernández, S.; Garcia-Gordillo, M.A.; Pérez-Gómez, J.; Carlos-Vivas, J. Test-retest reliability of five times sit to stand test (ftsst) in adults: A systematic review and meta-analysis. Biology 2021, 10, 510. [Google Scholar] [CrossRef] [PubMed]
- Cayrou, S.; Dickès, P.; Gauvain-Piquard, A.; Rogé, B. The Mental Adjustment to Cancer (MAC) Scale: French replication and assessment of positive and negative adjustment dimensions. Psycho-Oncology J. Psychol. Soc. Behav. Dimens. Cancer 2003, 12, 8–23. [Google Scholar] [CrossRef]
- Watson, M.; Homewood, J. Mental Adjustment to Cancer Scale©: Psychometric properties in a large cancer cohort. Psycho-Oncology 2008, 17, 1146–1151. [Google Scholar] [CrossRef]
- Smith, A.B.; Selby, P.J.; Velikova, G.; Stark, D.; Wright, E.P.; Gould, A.; Cull, A. Factor analysis of the hospital anxiety and depression scale from a large cancer population. Psychol. Psychother. Theory Res. Pract. 2002, 75, 165–176. [Google Scholar] [CrossRef]
- Aminisani, N.; Nikbakht, H.; Jafarabadi, M.A.; Shamshirgaran, S.M. Depression, anxiety, and health related quality of life among colorectal cancer survivors. J. Gastrointest. Oncol. 2017, 8, 81–88. [Google Scholar] [CrossRef]
- Roudijk, B.; Ludwig, K.; Devlin, N. EQ-5D-5L value set summaries. In Value Sets for EQ-5D-5L: A Compendium, Comparative Review & User Guide; Springer International Publishing: Berlin/Heidelberg, Germany, 2022; pp. 55–212. [Google Scholar] [CrossRef]
- Flyum, I.R.; Mahic, S.; Grov, E.K.; Joranger, P. Health-related quality of life in patients with colorectal cancer in the palliative phase: A systematic review and meta-analysis. BMC Palliat. Care 2021, 20, 144. [Google Scholar] [CrossRef]
- Pesce, A.; Fabbri, N.; Colombari, S.; Uccellatori, L.; Grazzi, G.; Lordi, R.; Anania, G.; Feo, C.V. A randomized controlled clinical trial on multimodal prehabilitation in colorectal cancer patients to improve functional capacity: Preliminary results. Surg. Endosc. 2024, 38, 7440–7450. [Google Scholar] [CrossRef]
- Piraux, E.; Caty, G.; Reychler, G. Effects of preoperative combined aerobic and resistance exercise training in cancer patients undergoing tumour resection surgery: A systematic review of randomised trials. Surg. Oncol. 2018, 27, 584–594. [Google Scholar] [CrossRef] [PubMed]
- Suen, M.; Liew, A.; Turner, J.D.; Khatri, S.; Lin, Y.; Raso, K.L.; Vardy, J.L. Short-term multimodal prehabilitation improves functional capacity for colorectal cancer patients prior to surgery. Asia-Pacific J. Clin. Oncol. 2022, 18, E103–E110. [Google Scholar] [CrossRef]
- Minnella, E.M.; Carli, F. Prehabilitation and functional recovery for colorectal cancer patients. Eur. J. Surg. Oncol. (EJSO) 2018, 44, 919–926. [Google Scholar] [CrossRef] [PubMed]
- Carli, F.; Charlebois, P.; Stein, B.; Feldman, L.; Zavorsky, G.; Kim, D.J.; Scott, S.; Mayo, N.E. Randomized clinical trial of prehabilitation in colorectal surgery. Br. J. Surg. 2010, 97, 1187–1197. [Google Scholar] [CrossRef]
- van Rooijen, S.; Carli, F.; Dalton, S.; Thomas, G.; Bojesen, R.; Le Guen, M.; Barizien, N.; Awasthi, R.; Minnella, E.; Beijer, S.; et al. Multimodal prehabilitation in colorectal cancer patients to improve functional capacity and reduce postoperative complications: The first international randomized controlled trial for multimodal prehabilitation. BMC Cancer 2019, 19, 98. [Google Scholar] [CrossRef]
- Wu, F.; Rotimi, O.; Laza-Cagigas, R.; Rampal, T. The feasibility and effects of a telehealth-delivered home-based prehabilitation program for cancer patients during the pandemic. Curr. Oncol. 2021, 28, 2248–2259. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, J.; Zhu, H.; Zhang, X.; Jiang, Y.; Zhang, J. Effect of Psychological Intervention on Quality of Life and Psychological Outcomes of Colorectal Cancer Patients. Psychiatry 2020, 83, 58–69. [Google Scholar] [CrossRef]
- Downing, A.; Morris, E.J.; Richards, M.; Corner, J.; Wright, P.; Sebag-Montefiore, D.; Finan, P.; Kind, P.; Wood, C.; Lawton, S.; et al. Health-related quality of life after colorectal cancer in England: A patient-reported outcomes study of individuals 12 to 36 months after diagnosis. J. Clin. Oncol. 2015, 33, 616–624. [Google Scholar] [CrossRef]
- Mishra, S.I.; Scherer, R.W.; Snyder, C.; Geigle, P.M.; Berlanstein, D.R.; Topaloglu, O. Exercise interventions on health-related quality of life for people with cancer during active treatment. Cochrane Database Syst. Rev. 2012, 2012, CD008465. [Google Scholar] [CrossRef]
- Carpallo-Porcar, B.; Romo-Calvo, L.; Pérez-Palomares, S.; Jiménez-Sánchez, C.; Herrero, P.; la Cruz, N.B.-D.; Calvo, S. Efficacy of an asynchronous telerehabilitation program in post-COVID-19 patients: A protocol for a pilot randomized controlled trial. PLoS ONE 2022, 17, e0270766. [Google Scholar] [CrossRef]

| Age | Gender | Weight (kg) | Height (cm) | BMI (kg/cm) | Marital Status | Education Level | Employment Status | |
|---|---|---|---|---|---|---|---|---|
| Participant 1 | 36 | Male | 92.8 | 191 | 25.7 | Single | Secondary | Employed |
| Participant 2 | 62 | Female | 56.9 | 166 | 20.6 | Divorced | Primary | Employed |
| Participant 3 | 52 | Female | 53.4 | 164 | 20.8 | Divorced | University | Employed |
| Participant 4 | 56 | Male | 95.6 | 179 | 29.8 | Married | Secondary | Employed |
| Participant 5 | 62 | Male | 92.5 | 179 | 28.9 | Married | University | Employed |
| Variable | Participant | Assessment | Change Score | |||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T4 | T2–T1 | T3–T1 | T4–T1 | ||
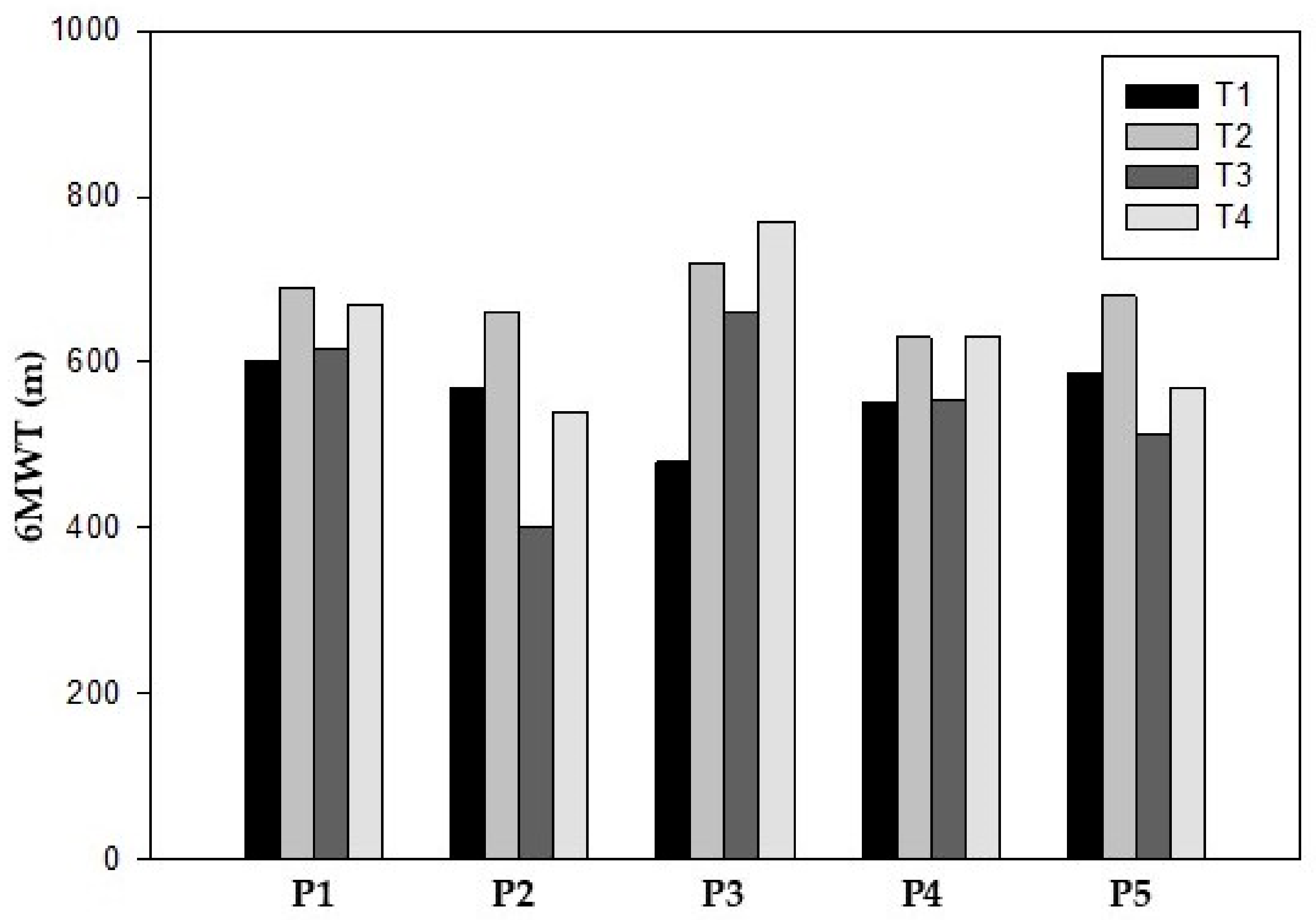
| 6MWT (meters) | P1 | 600 | 690 | 615 | 670 | 90 | 15 | 70 |
| P2 | 570 | 660 | 400 | 540 | 90 | −170 | −30 | |
| P3 | 480 | 720 | 660 | 770 | 240 | 180 | 290 | |
| P4 | 550 | 630 | 554 | 630 | 80 | 4 | 80 | |
| P5 | 586 | 680 | 514 | 570 | 94 | −72 | −16 | |
| Mean ± SD | 557.0 ± 47 | 676.0 ± 33.6 | 548.6 ± 100.2 | 652.5 ± 90.4 | 67.9 ± 118.8 | 130.9 ± 26.6 | 128.0 ± 78.8 | |
| Variable | Participant | Assessment | Change Score | |||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T4 | T2–T1 | T3–T1 | T4–T1 | ||
| Waist Circumference (cm) | P1 | 94 | 92 | 90 | 92 | −2 | −4 | −2 |
| P2 | 72 | 72 | 72 | 74 | 0 | 0 | 2 | |
| P3 | 75 | 71 | 70 | 73 | −4 | −5 | −2 | |
| P4 | 109 | 105.5 | 103 | 105 | −3.5 | −6 | −4 | |
| P5 | 102 | 100 | 98 | 99 | −2 | −4 | −3 | |
| Mean ± SD | 90.4 ± 16.3 | 83.8 ± 16.3 | 86.6 ± 15 | 88.6 ± 14.5 | (−) 2.3 ± 1.6 | (−) 3.8 ± 2.3 | (−) 1.8 ± 2.3 | |
| Hip Circumference (cm) | P1 | 106 | 106 | 106 | 106 | 0 | 0 | 0 |
| P2 | 99 | 91 | 92.5 | 94 | −8 | −6.5 | −5 | |
| P3 | 93 | 89 | 92.5 | 93 | −4 | −0.5 | 0 | |
| P4 | 105 | 104.5 | 104 | 104 | −0.5 | −1 | −1 | |
| P5 | 106 | 105 | 104 | 106 | −1 | −2 | 0 | |
| Mean ± SD | 101.8 ± 5.7 | 97.8 ± 9 | 104.7 ± 1.2 | 100.6 ± 6.5 | (−) 2.7 ± 3.3 | (−) 2.0 ± 2.6 | (−) 1.2 ± 2.2 | |
| Visceral Fat Level | P1 | 5 | 5 | 5 | 5 | 0 | 0 | 0 |
| P2 | 6 | 6 | 5 | 6 | 0 | −1 | 0 | |
| P3 | 4 | 4 | 3 | 4 | 0 | −1 | 0 | |
| P4 | 12 | 13 | 12 | 10 | 1 | 0 | −2 | |
| P5 | 13 | 14 | 12 | 16 | 1 | −1 | 2 | |
| Mean ± SD | 8 ± 4.2 | 8.4 ± 4.7 | 7.4 ± 4.3 | 8.2 ± 4.9 | 0.4 ± 0.5 | (−) 0.6 ± 0.5 | 0 ± 1.4 | |
| Weight (kg) | P1 | 92.8 | 89.2 | 86.8 | 90.6 | −3.6 | −6 | −2.2 |
| P2 | 56.9 | 56.1 | 54.2 | 55.7 | −0.8 | −2.7 | −1.2 | |
| P3 | 53.4 | 52.5 | 50.9 | 51.4 | −0.9 | −2.5 | −3 | |
| P4 | 95.6 | 94.5 | 89.1 | 90.5 | −1.1 | −6.5 | −5.1 | |
| P5 | 92.5 | 90.3 | 87.4 | 90.3 | −2.2 | −5.1 | −2.2 | |
| Mean ± SD | 78.2 ± 22.6 | 76.5 ± 21.8 | 73.7 ± 20.5 | 875.7 ± 21.4 | (−) 1.7 ± 1.2 | (−) 4.6 ± 1.9 | (−) 2.7 ± 1.5 | |
| Body Fat (Percentage) | P1 | 14.7 | 15.1 | 15 | 14.8 | 0.4 | 0.3 | 0.1 |
| P2 | 26.1 | 26.3 | 26.5 | 26.4 | 0.2 | 0.4 | 0.3 | |
| P3 | 23.5 | 20.5 | 20.4 | 23.1 | −3 | −3.1 | −0.4 | |
| P4 | 23.2 | 24.2 | 24.1 | 18.8 | 1 | 0.9 | −4.4 | |
| P5 | 24.2 | 25.3 | 22.9 | 26 | 1.1 | −1.3 | 1.8 | |
| Mean ± SD | 24.5 ± 1.5 | 22.3 ± 4.6 | 21.8 ± 4.4 | 21.8 ± 5 | (−) 0.1 ± 1.7 | (−) 0.6 ± 1.6 | (−) 0.5 ± 2.3 | |
| Muscle Mass (Percentage) | P1 | 75.3 | 72 | 70.2 | 73.4 | −3.3 | −5.1 | −1.9 |
| P2 | 39.9 | 39.0 | 39.4 | 38.9 | −0.9 | −0.5 | −1 | |
| P3 | 38.7 | 39.2 | 38.5 | 37.6 | 0.5 | −0.2 | −1.1 | |
| P4 | 69.9 | 68.1 | 64.2 | 69.8 | −1.8 | −5.7 | −0.1 | |
| P5 | 66.7 | 64.1 | 64.1 | 63.5 | −2.6 | −2.6 | −3.2 | |
| Mean ± SD | 58.1 ± 17.4 | 60.9 ± 14.8 | 55.3 ± 15.1 | 56.6 ± 17.2 | (−) 1.6 ± 1.5 | (−) 2.8 ± 2.5 | (−) 1.5 ± 1.2 | |
| BMI (Body Mass Index) | P1 | 25.7 | 24.7 | 24.3 | 24.8 | −1 | −1.4 | −0.9 |
| P2 | 20.6 | 20.4 | 19.9 | 20.2 | −0.2 | −0.7 | −0.4 | |
| P3 | 20.8 | 20.5 | 19.9 | 20.1 | −0.3 | −0.9 | −0.7 | |
| P4 | 29.8 | 29.5 | 27.8 | 28.2 | −0.3 | −2.3 | −1.6 | |
| P5 | 28.9 | 28.5 | 27.3 | 27.8 | −0.4 | −1.6 | −1.1 | |
| Mean ± SD | 25.2 ± 4.3 | 24.7 ± 4.3 | 23.8 ± 3.8 | 24.2 ± 3.9 | (−) 0.4 ± 0.3 | (−) 1.4 ± 0.6 | (−) 0.9 ± 0.5 | |
| Variable | Participant | Assessment | Change Score | |||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T4 | T2–T1 | T3–T1 | T4–T1 | ||
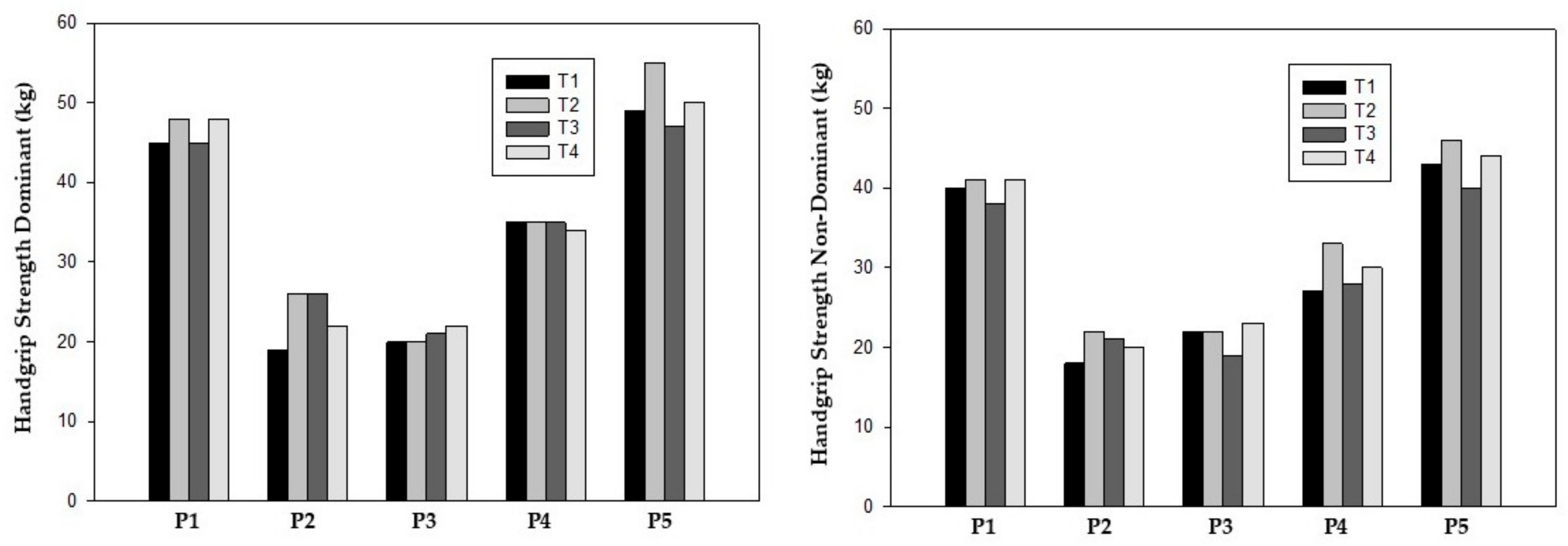
| Handgrip Strength Dominant (kg) | P1 | 45 | 48 | 45 | 48 | 3 | 0 | 3 |
| P2 | 19 | 26 | 26 | 22 | 7 | 7 | 3 | |
| P3 | 20 | 20 | 21 | 22 | 0 | 1 | 2 | |
| P4 | 35 | 35 | 35 | 34 | 0 | 0 | −1 | |
| P5 | 49 | 55 | 47 | 50 | 6 | −2 | 1 | |
| Mean ± SD | 33.6 ± 13.8 | 36.8 ± 14.7 | 34.8 ± 11.4 | 35.2 ± 13.5 | 3.2 ± 3.3 | 1.2 ± 3.4 | 1.6 ± 1.7 | |
| Handgrip Strength Non-dominant (kg) | P1 | 40 | 41 | 38 | 41 | 1 | −2 | 1 |
| P2 | 18 | 22 | 21 | 20 | 4 | 3 | 2 | |
| P3 | 22 | 22 | 19 | 23 | 0 | −3 | 1 | |
| P4 | 27 | 33 | 28 | 30 | 5 | 1 | 3 | |
| P5 | 43 | 46 | 40 | 44 | 3 | −3 | 1 | |
| Mean ± SD | 30.0 ± 11 | 32.8 ± 10.9 | 29.2 ± 9.6 | 31.6 ± 10.6 | 2.6 ± 2.1 | (−) 0.8 ± 2.7 | 1.6 ± 0.9 | |
| Sit-to-stand 5R-STS (s) | P1 | 13.09 | 10.84 | 11.5 | 9.84 | −2.25 | −1.59 | −3.25 |
| P2 | 10.72 | 10.63 | 14.94 | 9.78 | −0.09 | 4.22 | −0.94 | |
| P3 | 8.37 | 6.8 | 7.25 | 5.85 | −1.57 | −1.12 | −2.52 | |
| P4 | 11.46 | 7.46 | 10.1 | 10.46 | −4 | −1.36 | −1 | |
| P5 | 7.69 | 6.28 | 8.69 | 6.34 | −1.41 | 1 | −1.35 | |
| Mean ± SD | 10.3 ± 2.2 | 7.8 ± 2 | 10.5 ± 2.9 | 8.5 ± 2.2 | 1.9 ± 1.4 | 0.2 ± 2.5 | (−) 1.8 ± 1 | |
| Variable | Participant | Assessment | Change Score | |||
|---|---|---|---|---|---|---|
| T1 | T4 | T5 | T4–T1 | T5–T1 | ||
| Fighting Spirit (FS) | P1 | 30 | 31 | 31 | 1 | 1 |
| P2 | 34 | 28 | 28 | −6 | −6 | |
| P3 | 24 | 26 | 26 | −2 | −2 | |
| P4 | 29 | 31 | 29 | 2 | 0 | |
| P5 | 29 | 28 | 28 | −1 | −1 | |
| Mean ± SD | 29.2 ± 3.6 | 28.8 ± 2.2 | 28.4 ± 1.8 | (−) 1.0 ± 3.6 | (−) 1.5 ± 3.1 | |
| Anxious Preoccupation (AP) | P1 | 19 | 21 | 21 | 2 | 2 |
| P2 | 19 | 22 | 22 | 3 | 3 | |
| P3 | 19 | 23 | 23 | 4 | 4 | |
| P4 | 16 | 21 | 20 | 5 | 4 | |
| P5 | 19 | 26 | 26 | 7 | 7 | |
| Mean ± SD | 18.4 ± 1.3 | 22.6 ± 2.1 | 22.4 ± 2.3 | 4.2 ± 1.9 | 4.0 ± 1.9 | |
| Fatalism (FA) | P1 | 24 | 16 | 16 | −8 | −8 |
| P2 | 17 | 18 | 18 | 1 | 1 | |
| P3 | 11 | 13 | 13 | 2 | 2 | |
| P4 | 15 | 17 | 14 | 2 | −1 | |
| P5 | 19 | 15 | 15 | −4 | −4 | |
| Mean ± SD | 17.2 ± 4.8 | 15.8 ± 1.9 | 15.2 ± 1.9 | (−) 1.4 ± 4.4 | (−) 2.0 ± 4.1 | |
| Helplessness/Hopelessness (HH) | P1 | 22 | 25 | 25 | 3 | 3 |
| P2 | 22 | 24 | 24 | 2 | 2 | |
| P3 | 30 | 27 | 27 | −3 | −3 | |
| P4 | 23 | 27 | 23 | 4 | 0 | |
| P5 | 26 | 25 | 25 | −1 | −1 | |
| Mean ± SD | 24.6 ± 3.4 | 25.6 ± 1.3 | 24.8 ± 1.5 | 1.0 ± 2.9 | 0.2 ± 2.4 | |
| Cognitive Avoidance (CA) | P1 | 8 | 7 | 7 | −1 | −1 |
| P2 | 5 | 7 | 7 | 2 | 2 | |
| P3 | 5 | 7 | 7 | 2 | 2 | |
| P4 | 6 | 7 | 7 | 1 | 1 | |
| P5 | 6 | 7 | 7 | 1 | 1 | |
| Mean ± SD | 6.0 ± 1.2 | 7.0 ± 0 | 7.0 ± 0 | 1.0 ± 1.2 | 1.0 ± 1.2 | |
| Variable | Participant | Assessment | Change Score | |||
|---|---|---|---|---|---|---|
| T1 | T4 | T5 | T4–T1 | T5–T1 | ||
| HADS-A | P1 | 4 | 5 | 5 | 1 | 1 |
| P2 | 13 | 9 | 9 | −4 | −4 | |
| P3 | 14 | 13 | 13 | −1 | −1 | |
| P4 | 5 | 3 | 3 | −2 | −2 | |
| P5 | 15 | 6 | 6 | −9 | −9 | |
| Mean ± SD | 10.2 ± 5.3 | 7.2 ± 3.9 | 7.2 ± 3.9 | (−) 3.0 ± 3.8 | (−) 3.0 ± 3.8 | |
| HADS-D | P1 | 6 | 7 | 7 | 1 | 1 |
| P2 | 4 | 5 | 5 | 1 | 1 | |
| P3 | 12 | 7 | 7 | −5 | −5 | |
| P4 | 5 | 5 | 5 | 0 | 0 | |
| P5 | 10 | 6 | 6 | −4 | −4 | |
| Mean ± SD | 7.4 ± 3.4 | 6.0 ± 1 | 6.0 ± 1 | (−) 1.4 ± 2.9 | (−) 1.4 ± 2.9 | |
| T1 | |||||||
| Participant | Mobility | Self-Care | Usual Activities | Pain/Discomfort | Anxiety/Depression | EQ-5D Index | EQ-VAS |
| P1 | 1 | 1 | 1 | 1 | 1 | 1.000 | 60 |
| P2 | 1 | 1 | 1 | 1 | 1 | 1.000 | 80 |
| P3 | 1 | 1 | 1 | 1 | 2 | 0.932 | 70 |
| P4 | 1 | 1 | 1 | 1 | 1 | 1.000 | 80 |
| P5 | 1 | 1 | 1 | 1 | 2 | 0.932 | 95 |
| Mean ± SD | 0.973 ± 0.04 | 77.0 ± 13.04 | |||||
| T2 | |||||||
| Participant | Mobility | Self-Care | Usual Activities | Pain/Discomfort | Anxiety/Depression | EQ-5D Index | EQ-VAS |
| P1 | 1 | 1 | 1 | 2 | 1 | 0.924 | 65 |
| P2 | 1 | 1 | 1 | 1 | 1 | 1.000 | 80 |
| P3 | 1 | 1 | 1 | 1 | 2 | 0.932 | 75 |
| P4 | 1 | 1 | 1 | 1 | 1 | 1.000 | 80 |
| P5 | 1 | 1 | 1 | 1 | 2 | 0.932 | 95 |
| Mean ± SD | 0.958 ± 0.04 | 79.0 ± 10.84 | |||||
| T3 | |||||||
| Participant | Mobility | Self-Care | Usual Activities | Pain/Discomfort | Anxiety/Depression | EQ-5D Index | EQ-VAS |
| P1 | 1 | 1 | 1 | 2 | 1 | 0.924 | 60 |
| P2 | 1 | 1 | 2 | 2 | 1 | 0.849 | 50 |
| P3 | 1 | 1 | 1 | 1 | 2 | 0.932 | 50 |
| P4 | 1 | 1 | 1 | 2 | 2 | 0.857 | 70 |
| P5 | 1 | 1 | 1 | 1 | 1 | 1.000 | 60 |
| Mean ± SD | 0.912 ± 0.06 | 58.0 ± 8.37 | |||||
| T4 | |||||||
| Participant | Mobility | Self-Care | Usual Activities | Pain/Discomfort | Anxiety/Depression | EQ-5D Index | EQ-VAS |
| P1 | 1 | 1 | 1 | 1 | 1 | 1.000 | 40 |
| P2 | 1 | 1 | 1 | 1 | 2 | 0.932 | 50 |
| P3 | 1 | 1 | 1 | 1 | 2 | 0.932 | 40 |
| P4 | 1 | 1 | 1 | 2 | 2 | 0.857 | 90 |
| P5 | 1 | 1 | 1 | 1 | 1 | 1.000 | 95 |
| Mean ± SD | 0.944 ± 0.06 | 68.8 ± 27.80 | |||||
| T5 | |||||||
| Participant | Mobility | Self-Care | Usual Activities | Pain/Discomfort | Anxiety/Depression | EQ-5D Index | EQ-VAS |
| P1 | 1 | 1 | 1 | 1 | 1 | 1.000 | 50 |
| P2 | 1 | 1 | 1 | 1 | 2 | 0.932 | 70 |
| P3 | 1 | 1 | 1 | 1 | 2 | 0.932 | 50 |
| P4 | 1 | 1 | 1 | 2 | 2 | 0.857 | 70 |
| P5 | 1 | 1 | 1 | 1 | 1 | 1.000 | 95 |
| Mean ± SD | 0.944 ± 0.06 | 67.0 ± 18.57 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burgos-Bragado, J.M.; Brandín-de la Cruz, N.; Carpallo-Porcar, B.; Blas-Laina, J.L.; Calvo, S.; Jiménez-Sánchez, C. Integrating Telerehabilitation into the Prehabilitation and Rehabilitation Pathway in Colorectal Cancer: A Case Series. Reports 2025, 8, 60. https://doi.org/10.3390/reports8020060
Burgos-Bragado JM, Brandín-de la Cruz N, Carpallo-Porcar B, Blas-Laina JL, Calvo S, Jiménez-Sánchez C. Integrating Telerehabilitation into the Prehabilitation and Rehabilitation Pathway in Colorectal Cancer: A Case Series. Reports. 2025; 8(2):60. https://doi.org/10.3390/reports8020060
Chicago/Turabian StyleBurgos-Bragado, Jose Manuel, Natalia Brandín-de la Cruz, Beatriz Carpallo-Porcar, Juan Luis Blas-Laina, Sandra Calvo, and Carolina Jiménez-Sánchez. 2025. "Integrating Telerehabilitation into the Prehabilitation and Rehabilitation Pathway in Colorectal Cancer: A Case Series" Reports 8, no. 2: 60. https://doi.org/10.3390/reports8020060
APA StyleBurgos-Bragado, J. M., Brandín-de la Cruz, N., Carpallo-Porcar, B., Blas-Laina, J. L., Calvo, S., & Jiménez-Sánchez, C. (2025). Integrating Telerehabilitation into the Prehabilitation and Rehabilitation Pathway in Colorectal Cancer: A Case Series. Reports, 8(2), 60. https://doi.org/10.3390/reports8020060






