Abstract
Background and Clinical Significance: Acute esophageal necrosis (AEN), or black esophagus, is an extraordinary rare source of acute upper gastrointestinal bleeding. Its pathogenesis is still poorly understood, whereas etiology seems to be multifactorial, mainly involving esophageal ischemia, increased acid reflux, and reduced mucosal defenses. Although alcohol abuse has been reported to be a common trigger factor, only one case of AEN due to severe alcoholic lactic acidosis has been described up to date. Case Presentation: Herein, we describe a case of a non-cirrhotic 61-year-old lady with a history of chronic alcohol abuse, who was admitted to the Emergency Room due to upper gastrointestinal (GI) bleeding. AEN caused by severe alcoholic lactic acidosis was promptly diagnosed by subsequent investigations, including blood test, urinalysis, computed tomography, and upper GI endoscopy. The treatment involved a multidisciplinary, aggressive medical approach, which included one hemodialysis session. Conclusions: This is the second documented case of AEN secondary to alcoholic lactic acidosis, successfully treated with a previously unreported aggressive multidisciplinary approach, involving one hemodialysis session. It highlights the value of a multidisciplinary approach in managing such complex and rare conditions.
1. Introduction and Clinical Significance
First reported in 1990 by Goldenberg and colleagues [1], acute esophageal necrosis (AEN), also defined as black esophagus, is a rare and potentially life-threatening condition, characterized endoscopically by black-colored esophageal mucosa abruptly ending at the gastro-esophageal junction, and histologically by extensive mucosal necrosis [2,3,4]. Upper gastrointestinal bleeding is the most common clinical presentation of AEN [2,5,6].
The exact pathogenesis is still unknown, but its etiology seems to be multifactorial, encompassing esophageal ischemia, increased acid reflux, and reduced mucosal defenses [2,3,4]. Various conditions have been associated with the development of AEN, such as hemodynamic compromise, some medications, diabetic ketoacidosis, inflammatory states, malignancy, surgery, gastric outlet obstruction, and chronic alcohol abuse [2,3,4]. Although the latter has been shown to be the predisposing factor in up to 25% of patients with AEN [7,8], until now only one case of AEN secondary to alcoholic lactic acidosis has been reported [9].
To date, there is no specific treatment for AEN. Hydration, acid suppression, bowel rest, antibiotics in case of infection, and proper treatment of the underlying illness currently represent the mainstay of AEN management [4,10,11].
However, given the rarity of the disease, optimal management is still unclear.
The reported mortality of AEN is high, ranging from 30% to 50%, mainly reflecting the severity of the underlying illness [5,11,12].
Herein, we describe a case of AEN caused by severe alcoholic lactic acidosis, successfully treated by means of a previously unreported multidisciplinary, aggressive medical approach, involving one hemodialysis session.
2. Case Presentation
A 61-year-old lady with a history of chronic alcohol abuse was admitted to the Emergency Room due to a 24 h severe epigastric pain associated with episodes of vomiting and recent onset of active coffee-ground emesis with signs of hemodynamic instability. Her past medical history included alcoholic liver disease in the absence of cirrhosis. She declared alcohol binging during the previous days. Conversely, the ingestion of any caustic agents, methanol, and drugs was denied.
2.1. Diagnostic Evaluation
At the time of the admission, she was pale, afebrile, eupneic in room air, with a regular pulse of 110 bpm, and a blood pressure of 100/70 mmHg. Mild conscious impairment was present. Her physical examination was negative for any evidence of portal hypertension or other stigmata of chronic liver disease. Abdominal examination revealed a distended abdomen and a moderate epigastric tenderness. The rectal examination did not exhibit melena or blood. A Foley catheter was inserted into the bladder, and normochromic urine was returned. A naso-gastric tube was placed and about 500 mL of coffee-ground material with blood traces and clots was removed.
Arterial blood gas measurements showed the following: pH 7.22, PaCO2 16.2 mmHg, PaO2 107.7 mmHg, AG 26.3 mmol/L, HCO3− 6.7 mmol/L, lactate > 20.0 mmol/L, glucose 62 mg/dL.
Laboratory examinations were remarkable for moderate anemia (hemoglobin 8.5 g/dL) and mild hepatic cytolysis (AST 68 UI/L, ALT 70 UI/L). All remaining laboratory examinations, including liver and renal function tests, were within normal values. Blood tests for ethanol, isopropanol, methanol, and ethylene glycol screening were all negative. Urinalysis revealed neither ketones nor oxalate crystals. Urine drug screen was negative.
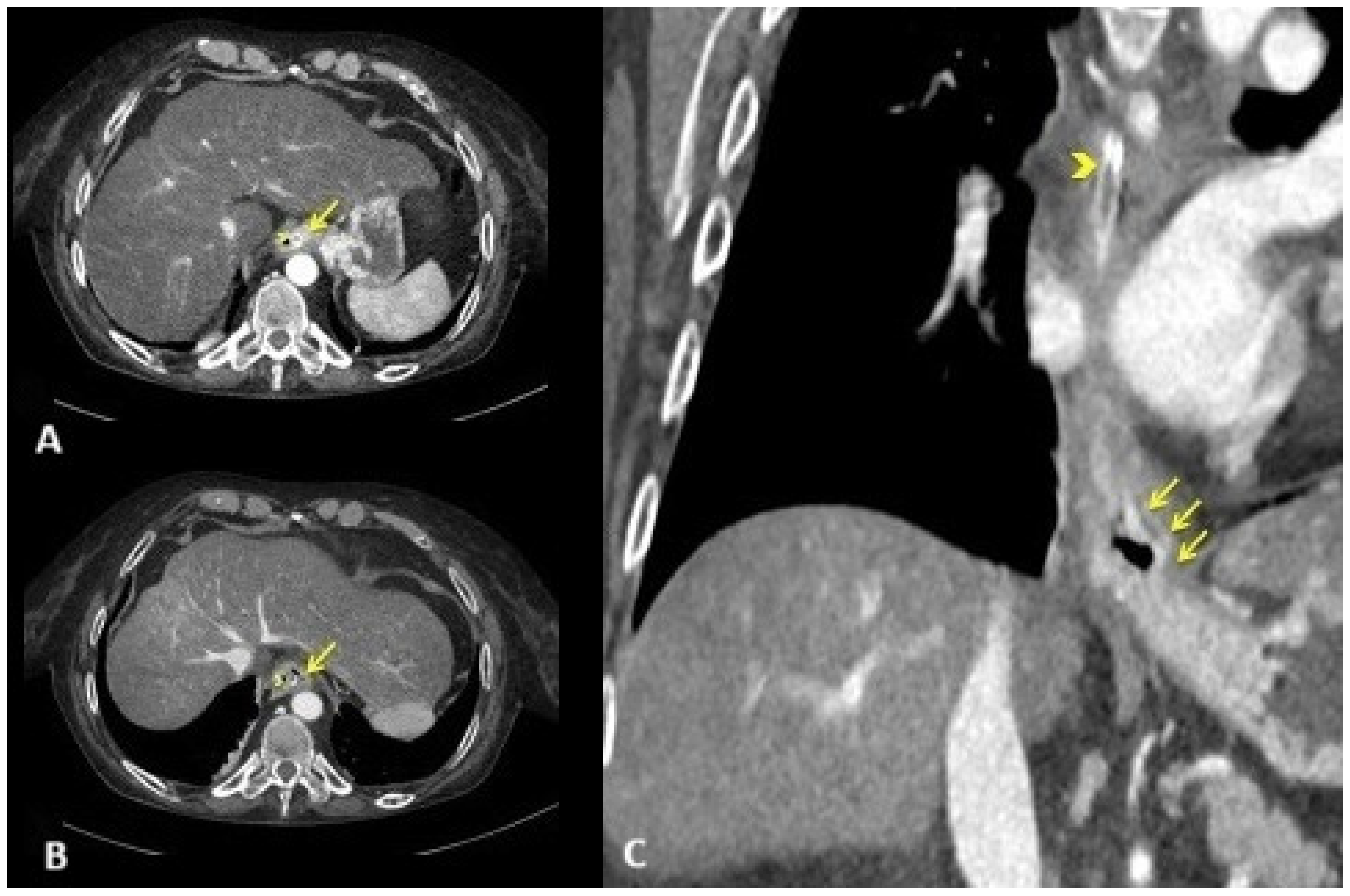
Fluids with 80 mL of 7% sodium bicarbonate, thiamine, and high-dose pantoprazole were administered intravenously. Then, an emergent computed tomography angiography was performed, demonstrating a grossly dilated gastric cavity alongside a thickened distal esophagus with evidence of transmural inflammation, in the absence of free air or active bleeding (Figure 1).
Figure 1.
Emergent computed tomography angiography. Axial arterial (A) CT scan at the level of the gastro-esophageal junction and venous (B) CT scan at the level of lower thoracic esophagus showing circumferential thickening of the esophageal wall. Note the mucosal enhancement ((A); yellow arrow) with wall hypoattenuation, producing the target sign ((B); yellow arrow). Coronal venous CT reconstruction showing extension of esophagitis predominantly to the distal third of the esophagus, including the gastro-esophageal junction ((C); yellow arrows). Nasogastric tube ((A–C); yellow arrowhead).
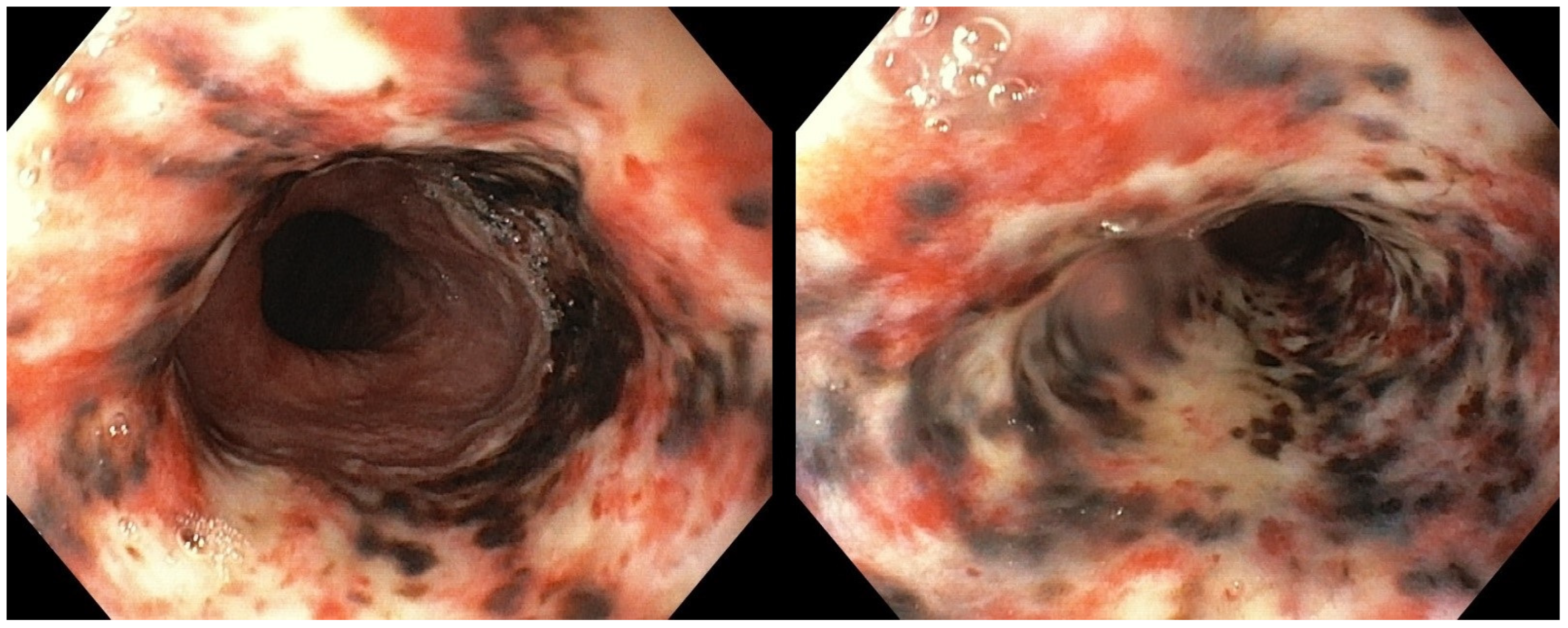
The patient was admitted to our Bleeding Unit. After the hemodynamic stabilization, an urgent esophagogastroduodenoscopy (EGD) under monitored anesthesia care was carried out. The endoscopic examination showed diffuse, circumferential, black-colored, friable mucosa at the middle and the distal esophagus, in the absence of signs of active bleeding. Gastric mucosa was spared (Figure 2). Esophageal biopsies were not taken at this time due to concern about a possible perforation.
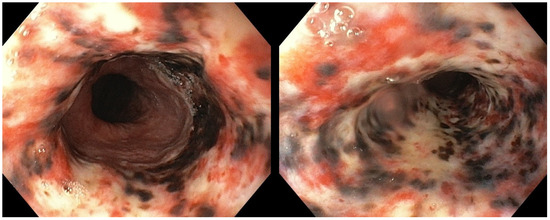
Figure 2.
Urgent esophagogastroduodenoscopy showing diffusely black-colored mucosa at the level of the middle and the distal esophagus, abruptly ending at the gastro-esophageal junction.
2.2. Treatment and Outcome
Treatment with total parenteral nutrition and a high dose of pantoprazole continuous infusion was started. However, despite aggressive intravenous hydration, repeated arterial blood gas analysis at 2, 3, and 5 h after the patient’s admission, showed the persistence of severe lactic acidosis (pH 7.28, anion gap 26.0 mmol/L, lactate 19.9 mmol/L, HCO3− 8.1 mmol/L). Thus, following a multidisciplinary evaluation which involved the nephrologist and the emergency physician, an urgent dialysis was planned. A single 3 h and 30 min hemodialysis session was carried out, resulting in nearly normalization of the severe lactic acidosis (pH 7.46, anion gap 11 mmol/L, lactates 7.4 mmol/L, HCO3− 23.5 mmol/L).
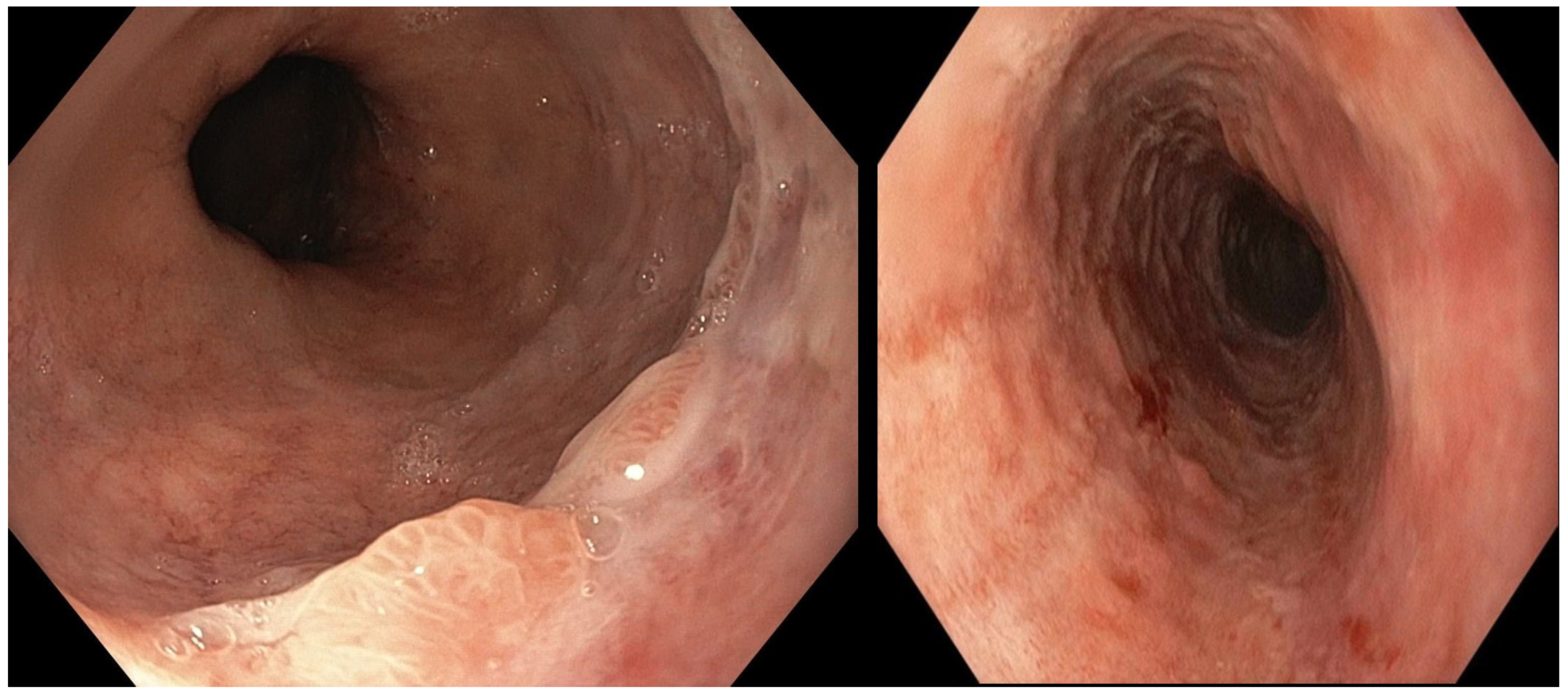
Post-operative stay was uneventful. Following the normal intestinal canalization and a clinical and laboratory improvement, on day 5, oral diet was gradually resumed. On day 7, EGD was repeated, showing nearly complete healing of the AEN, with only mild hyperemia and congestion at the medial and the distal esophagus, in the absence of strictures or other complications (Figure 3). Esophageal biopsies were taken, evidencing mild epithelial non-specific inflammation only. The patient was discharged home on day 8, and no complications were observed up to the 6-month follow-up.
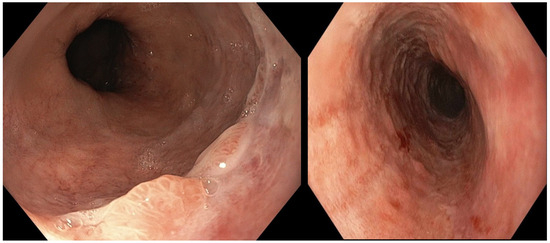
Figure 3.
Follow-up esophagogastroduodenoscopy showing a nearly complete resolution of the esophageal necrosis, with mild hyperemia and congestion at the level of the middle and the distal esophagus.
3. Discussion
AEN is an extremely rare disease, with a reported incidence ranging from 0.0125% to 0.2% [12,13,14], which mainly presents with upper gastrointestinal bleeding [2,5,6]. It is associated with poor prognosis. Indeed, the overall mortality is approximately 30–50% [5,11,12], mainly related to underlying critical illness. Conversely, the mortality directly related to AEN is relatively low, at about 6% [11]. The main complications of AEN include esophageal perforation and stenosis. The first one is the most severe and has a reported incidence of approximately 5–7%, whereas the last one is a late complication encountered in about 10% of patients on follow-up endoscopy [15]. Although the exact pathogenesis of AEN is still unknown, its etiology seems to be multifactorial, mainly involving esophageal ischemia, increased acid reflux, and reduced mucosal defenses [4]. Several conditions have been reported to be associated with the development of AEN, including alcohol abuse, which has been identified as the triggering factor in up to 25% of patients [7,8]. However, to date, only one case of AEN secondary to alcoholic lactic acidosis has been reported [9].
Conservative supportive care, primarily including hydration, acid suppression, bowel rest, and antibiotics in case of infection, along with an adequate treatment of the underlying medical conditions, is currently suggested in almost all cases [4,10,11]. However, given the rarity of the disease, the optimal treatment strategy is still unknown.
As previously reported by Endo and colleagues [8], the leading pathogenesis of our case might be accounted for by the systemic hypoperfusion induced by severe alcoholic lactic acidosis. However, in our case, an early response of severe alcoholic lactic acidosis to vigorous intravenous hydration was not observed. Lactic acidosis is associated with sudden death in alcoholics and has profound effects on the circulation system and organ perfusion [16,17,18]. Thus, following a multidisciplinary evaluation, a single hemodialysis session was performed, aimed at improving the patient’s prognosis [19,20]. A prompt resolution of the lactic acidosis was subsequently observed. Moreover, the resolution of EAN was observed early at one week, and neither early nor late complications were encountered.
To the best of our knowledge, the presented case is the second report of AEN secondary to severe alcoholic lactic acidosis, which was effectively treated with a previously unreported aggressive multidisciplinary approach, involving one hemodialysis session.
4. Conclusions
Early recognition and aggressive multidisciplinary approach are crucial for the successful management of AEN secondary to severe alcoholic lactic acidosis and therefore to improving outcomes of this life-threatening disease.
Author Contributions
Conceptualization, L.O. and A.M.; methodology, A.M.; validation, O.P.; formal analysis, A.M; investigation, L.O. and A.M.; resources, L.O. and O.P.; data curation, A.M.; writing—original draft preparation, L.O. and A.M.; writing—review and editing, L.O., A.M., O.P., M.D.S., and G.L.; visualization, A.M.; supervision, M.D.S. and G.L.; project administration, G.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. In accordance with local standards, our Institution AORN "Antonio Cardarelli"does not require ethical approval or institutional review board approval for reporting individual case reports when informed consent is provided by the patient.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to privacy concerns.
Acknowledgments
We are grateful to Velia De Magistris for English editing.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Goldenberg, S.P.; Wain, S.L.; Marignani, P. Acute necrotizing esophagitis. Gastroenterology 1990, 98, 493–496. [Google Scholar] [CrossRef] [PubMed]
- Schizas, D.; Theochari, N.A.; Mylonas, K.S.; Kanavidis, P.; Spartalis, E.; Triantafyllou, S.; Economopoulos, K.P.; Theodorou, D.; Liakakos, T. Acute esophageal necrosis: A systematic review and pooled analysis. World J. Gastrointest. Surg. 2020, 27, 104–115. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gurvits, G.E. Black esophagus: Acute esophageal necrosis syndrome. World J. Gastroenterol. 2010, 14, 3219–3225. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sheikh, A.B.; Mirza, S.; Abbas, R.; Javed, N.; Nguyen, A.; Hanif, H.; Farooq, A. Acute Esophageal Necrosis: An In-depth Review of Pathogenesis, Diagnosis and Management. J Community Hosp. Intern. Med. Perspect. 2022, 31, 96–103. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Orlando, D.; Carabotti, M.; Ruggeri, M.; Esposito, G.; Corleto, V.D.; Di Giulio, E.; Annibale, B. Occurrence of Acute Oesophageal Necrosis (Black Oesophagus) in a Single Tertiary Centre. J. Clin. Med. 2019, 24, 1532. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lamers, C.R.; Mares, W.G.N.; Bac, D.J. Black esophagus: A case series and literature review of acute esophageal necrosis. Scand. J. Gastroenterol. 2018, 53, 1421–1424. [Google Scholar] [CrossRef] [PubMed]
- Siddiqi, A.; Chaudhary, F.S.; Naqvi, H.A.; Saleh, N.; Farooqi, R.; Yousaf, M.N. Black esophagus: A syndrome of acute esophageal necrosis associated with active alcohol drinking. BMJ Open Gastroenterol. 2020, 7, e000466. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Abdullah, H.M.; Ullah, W.; Abdallah, M.; Khan, U.; Hurairah, A.; Atiq, M. Clinical presentations, management, and outcomes of acute esophageal necrosis: A systemic review. Expert Rev. Gastroenterol. Hepatol. 2019, 13, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Endo, T.; Sakamoto, J.; Sato, K.; Takimoto, M.; Shimaya, K.; Mikami, T.; Munakata, A.; Shimoyama, T.; Fukuda, S. Acute esophageal necrosis caused by alcohol abuse. World J. Gastroenterol. 2005, 21, 5568–5570. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rehman, O.; Jaferi, U.; Padda, I.; Khehra, N.; Atwal, H.; Parmar, M. Epidemiology, Pathogenesis, and Clinical Manifestations of Acute Esophageal Necrosis in Adults. Cureus 2021, 25, e16618. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gurvits, G.E.; Shapsis, A.; Lau, N.; Gualtieri, N.; Robilotti, J.G. Acute esophageal necrosis: A rare syndrome. J. Gastroenterol. 2007, 42, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Augusto, F.; Fernandes, V.; Cremers, M.I.; Oliveira, A.P.; Lobato, C.; Alves, A.L.; Pinho, C.; de Freitas, J. Acute necrotizing esophagitis: A large retrospective case series. Endoscopy 2004, 36, 411–415. [Google Scholar] [CrossRef] [PubMed]
- Gurvits, G.E.; Cherian, K.; Shami, M.N.; Korabathina, R.; El-Nader, E.M.; Rayapudi, K.; Gandolfo, F.J.; Alshumrany, M.; Patel, H.; Chowdhury, D.N.; et al. Black esophagus: New insights and multicenter international experience in 2014. Dig. Dis. Sci. 2015, 60, 444–453. [Google Scholar] [CrossRef] [PubMed]
- Ben Soussan, E.; Savoye, G.; Hochain, P.; Hervé, S.; Antonietti, M.; Lemoine, F.; Ducrotté, P. Acute esophageal necrosis: A 1-year prospective study. Gastrointest. Endosc. 2002, 56, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Dias, E.; Santos-Antunes, J.; Macedo, G. Diagnosis and management of acute esophageal necrosis. Ann. Gastroenterol. 2019, 32, 529–540. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Templeton, A.H.; Carter, K.L.; Sheron, N.; Gallagher, P.J.; Verrill, C. Sudden unexpected death in alcohol misuse--an unrecognized public health issue? Int. J. Environ. Res. Public Health 2009, 6, 3070–3081. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stacpoole, P.W.; Wright, E.C.; Baumgartner, T.G.; Bersin, R.M.; Buchalter, S.; Curry, S.H.; Duncan, C.; Harman, E.M.; Henderson, G.N.; Jenkinson, S.; et al. Natural history course of acquired lactic acidosis in adults DCA-Lactic Acidosis Study Group. Am. J. Med. 1994, 97, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.C.; Chan, K.S.; Tseng, K.L.; Weng, S.F. Prognosis of alcohol-associated lactic acidosis in critically ill patients: An 8-year study. Sci. Rep. 2016, 6, 35368. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kraut, J.A.; Madias, N.E. Lactic Acidosis: Current Treatments and Future Directions. Am. J. Kidney Dis. 2016, 68, 473–482. [Google Scholar] [CrossRef] [PubMed]
- Karthiraj, N.; Ramakrishnan, N.; Mani, A.K. Hemodialysis for Lactic Acidosis. Indian J. Crit. Care Med. 2017, 21, 537–538. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).