First Case of Chryseobacterium gleum Post-COVID-19 in a Child with Recurrent Fever
Abstract
1. Introduction and Clinical Significance
2. Case Description
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Holmes, B.; Owen, R.J.; Steigerwalt, A.G.; Brenner, D.J. Flavobacterium gleum, a new species found in human clinical specimens. Int. J. Syst. Bacteriol. 1984, 34, 21–25. [Google Scholar] [CrossRef]
- Lo, H.H.; Chang, S.M. Identification, characterization, and biofilm formation of clinical Chryseobacterium gleum isolates. Diagn. Microbiol. Infect. Dis. 2014, 79, 298–302. [Google Scholar] [CrossRef] [PubMed]
- Chiu, C.W.; Li, M.C.; Ko, W.C.; Li, C.W.; Chen, P.L.; Chang, C.M.; Lee, N.Y.; Lee, C.C. Clinical impact of Gram-negative nonfermenters on adults with community-onset bacteremia in the emergency department. J. Microbiol. Immunol. Infect. 2015, 48, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.; Alsoub, H. Chryseobacterium gleum bacteraemia: First reported cases from Qatar. New Microbes New Infect. 2021, 41, 100869. [Google Scholar] [CrossRef] [PubMed]
- Virok, D.P.; Abrok, M.; Szel, B.; Tajti, Z.; Mader, K.; Urban, E. Chryseobacterium gleum—A novel bacterium species detected in neonatal respiratory tract infections. J. Matern. Fetal Neonatal Med. 2014, 27, 1926–1929. [Google Scholar] [CrossRef]
- Abdul Wahab, A.; Taj-Aldeen, S.J.; Ibrahim, E.B.; Talaq, E.; Abu-Madi, M.; Fotedar, R. Discrepancy in MALDI-TOF MS identification of uncommon Gram-negative bacteria from lower respiratory secretions in patients with cystic fibrosis. Infect. Drug Resist. 2015, 8, 83–88. [Google Scholar] [CrossRef]
- Brkic, D.V.; Zlopasa, O.; Bedenic, B.; Plecko, V. Chryseobacterium gleum infection in patient with extreme malnutrition and hepatic lesion—Case report. Signa Vitae 2015, 10, 50–52. [Google Scholar]
- Ramya, T.G.; Baby, S.; Das, P.; Geetha, R.K. Chryseobacterium gleum urinary tract infection. Genes. Rev. 2015, 1, 1–5. [Google Scholar]
- Abdalhamid, B.; Elhadi, N.; Alsamman, K.; Aljindan, R. Chryseobacterium gleum pneumonia in an infant with nephrotic syndrome. IDCases 2016, 5, 34–36. [Google Scholar] [CrossRef]
- Lambiase, A.; Del Pezzo, M.; Raia, V.; Sepe, A.; Ferri, P.; Rossano, F. Chryseobacterium respiratory tract infections in patients with cystic fibrosis. J. Infect. 2007, 55, 518–523. [Google Scholar] [CrossRef]
- Jain, V.; Hussain, N.A.; Siddiqui, T.; Sahu, C.; Ghar, M.; Prasad, K.N. Simultaneous isolation of Chryseobacterium gleum from bloodstream and respiratory tract: First case report from India. JMM Case Rep. 2017, 4, e005122. [Google Scholar] [CrossRef] [PubMed]
- Arouna, O.; Deluca, F.I.; Camara, M.; Fall, B.; Fall, B.; Ba Diallo, A.; Docquier, J.D.; Mboup, S. Chryseobacterium gleum in a man with prostatectomy in Senegal: A case report and review of the literature. J. Med. Case Rep. 2017, 11, 118. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Singhal, L.; Gupta, V.; Mehta, V.; Singla, N.; Janmeja, A.K.; Chander, J. Sepsis due to Chryseobacterium gleum in a diabetic patient with chronic obstructive pulmonary disease: A case report and mini review. JPN J. Infect. Dis. 2017, 70, 687–688. [Google Scholar] [CrossRef]
- Stone, P.W. Economic burden of healthcare-associated infections: An American perspective. Expert. Rev. Pharmacoecon. Outcomes Res. 2009, 9, 417–422. [Google Scholar] [CrossRef]
- Amisha, F.; Fugere, T.; Caceres, J.; Rico Crescencio, J.C.; Falls, N. Chryseobacterium gleum Causing Healthcare-Associated Pneumonia in an Adult Male with Diffuse Large B Cell Lymphoma. Cureus 2021, 13, e19297. [Google Scholar] [CrossRef] [PubMed]
- Aykac, K.; Ozsurekci, Y.; Tuncer, O.; Sancak, B.; Cengiz, A.B.; Kara, A.; Ceyhan, M. Six cases during 2012–2015 and literature review of Chryseobacterium indologenes infections in pediatric patients. Can J Microbiol. 2016, 62, 812–819. [Google Scholar] [CrossRef]
- Mirza, H.C.; Tuncer, Ö.; Ölmez, S.; Şener, B.; Tuğcu, G.D.; Özçelik, U.; Gürsoy, N.C.; Otlu, B.; Büyükçam, A.; Kara, A.; et al. Clinical Strains of Chryseobacterium and Elizabethkingia spp. Isolated from Pediatric Patients in a University Hospital: Performance of MALDI-TOF MS-Based Identification, Antimicrobial Susceptibilities, and Baseline Patient Characteristics. Microb. Drug Resist. 2018, 24, 816–821. [Google Scholar] [CrossRef]
- Tsouvalas, C.; Mousa, G.; Lee, A.H.; Philip, J.A.; Levine, D. Chryseobacterium gleum isolation from respiratory culture following community-acquired pneumonia. Am. J. Case Rep. 2020, 21, e921172-1–e921172-5. [Google Scholar] [CrossRef]
- Anson, D.; Chaucer, B.; Norton, J.; Bansal, S. Multiple drug-resistant clabsi from an extremely rare bacterium, chryseobacterium gleum. Case Rep. Infect. Dis. 2020, 2020, 2097813. [Google Scholar] [CrossRef]
- Angrup, A.; Sharma, B.; Sehgal, I.S.; Biswal, M.; Ray, P. Emerging Bacterial Pathogens in the COVID-19 Era: Chryseobacterium gleum—A Case in Point. J. Lab. Physicians 2022, 15, 97–105. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lin, J.; Lai, C.; Yang, C.; Huang, Y. Differences in clinical manifestations, antimicrobial susceptibility patterns, and mutations of fluoroquinolone target genes between chryseobacterium gleum and chryseobacterium indologenes. Antimicrob. Agents Chemother. 2019, 63, e02256-18. [Google Scholar] [CrossRef] [PubMed]

| Examination | Results |
|---|---|
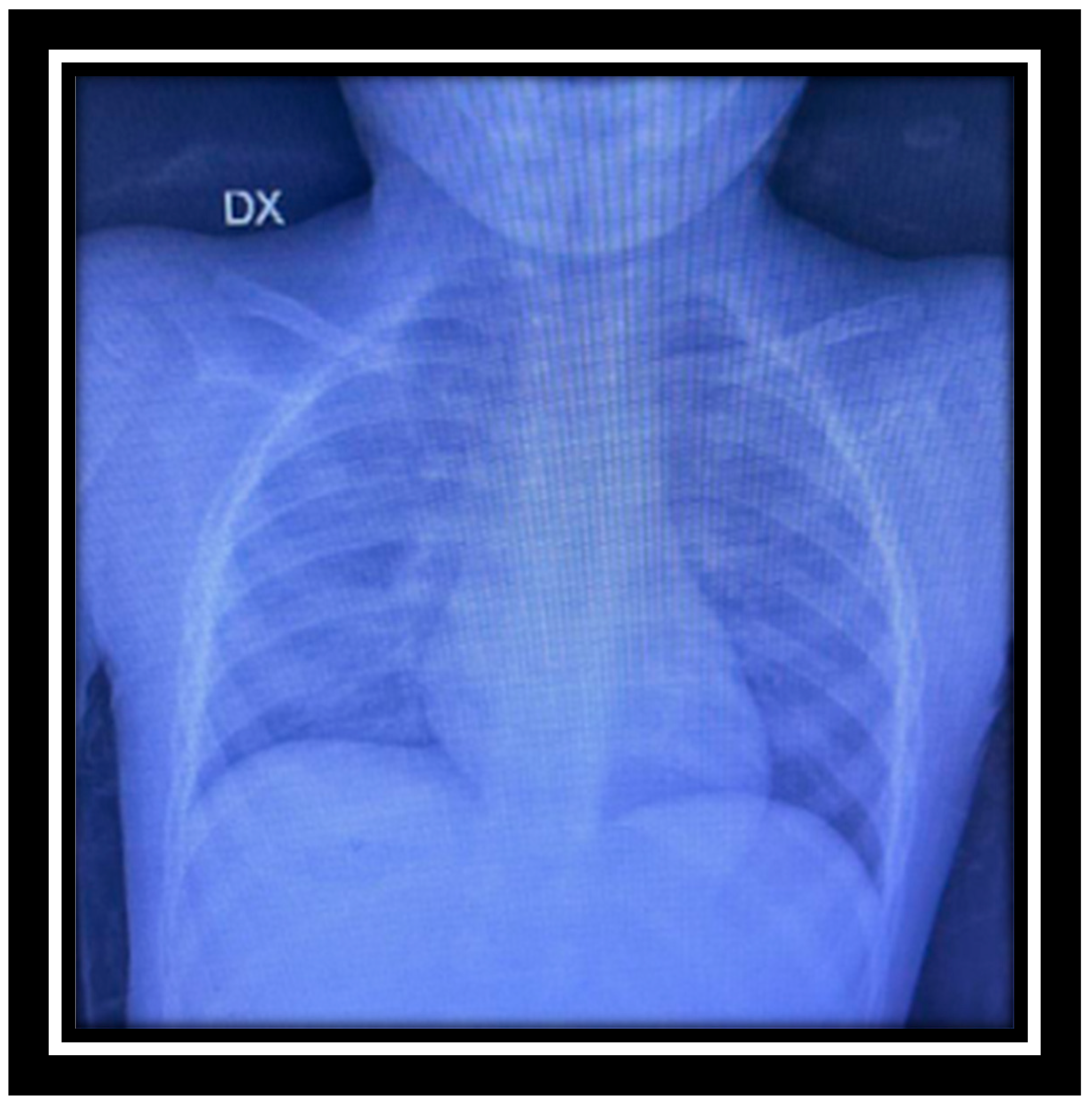
| Chest X-ray | mild accentuation of the bronchial structure |
| Lymph node echo | oval lymph nodes with thick, hypoechoic and thin cortex and hyperechoic central hilum |
| Peripheral blood smear | anisopoikilocytosis and elliptical red cells |
| Fine needle aspiration of the marrow | rich cellularity (C3, M1, MGK present) infiltrate |
| Microcytic Anemia Testing § | carrier of beta thalassemia trait, molecular analysis for triplication of the negative alpha gene |
| Admission (8 March) | Follow-Up (19 March) | Normal Range | |
|---|---|---|---|
| White Blood Cells | 9.99 | 19.68 | 4.60–10.20 × 103/mm3 |
| Red Cells | 5.47 | 5.47 | 4.20–6.10 × 106/µL |
| Hemoglobin | 8.5 | 8.8 | 12–18 g/dL |
| Hematocrit Test | 29.6 | 29.6 | 37–52% of red blood cells |
| Mean Corpuscular Volume | 54.1 | 54.1 | 80–99 µm3 |
| Mean Corpuscular Hemoglobin | 16 | 16 | 27–32 pg/cell |
| Mean Corpuscular Hemoglobin Concentration | 29.6 | 29.6 | 32–37 g/dL |
| Platelets | 424 | 325 | 130–400 |
| Mean Platelet Volume | 7 | 7 | 7.2–11 |
| Neutrophils | 12.12 (61.6%) | 12.12 (61.6%) | 10.63–6.96 (39.3–73.7%) |
| Lymphocytes | 6.11 (31.1%) | 6.11 (31.1%) | 1.09–2.99 (18–48%) |
| Monocytes | 1.22 (6.19%) | 1.22 (6.19%) | 0.24–0.79 (4.4–12.7% of white blood cells) |
| Eosinophils | - | - | 0.03–0.44 (0.6–7.3% of white blood cells) |
| Basophils | 0.23 (1.2%) | 0.23 (1.2%) | 0.0–0.08 (0.0–1.7% of white blood cells) |
| Erythrocyte Sedimentation Rate | 107 | 107 | <20 mm/h |
| C-reactive Protein | 4.88 | 188 | 0.3–5 mg/L |
| Procalcitonin | 0.02 | 1.11 | once 0.05 ng/ml |
| EBV | |||
| VCA IgM | 19 | U/mL > 40 | |
| VCA IgG | >750 | U/mL > 40 | |
| Bartonella henselae | |||
| IgM | 0.156 | Index > 1.1 | |
| IgG | 0.785 | Index > 1.1 |
| Antibiotics | MIC | Sensitivity Pattern |
|---|---|---|
| Amikacin | 32 | Resistant |
| Amoxyclav | 64 | Resistant |
| Aztreonam | 32 | Resistant |
| Cefotaxime | 8 | Resistant |
| Ceftazidime | 2 | Susceptible |
| Ceftazidime/avibactam | <0.5 | Susceptible |
| Ceftalozane/tazobactam | <0.5 | Susceptible |
| Ciprofloxacin | 0.25 | Susceptible |
| Ertapenem | 2 | Resistant |
| Gentamicin | 8 | Resistant |
| Imipenem | 4 | Intermediate |
| Meropenem | 16 | Resistant |
| Piperacillin/tazobactam | 32 | Resistant |
| Tigecycline | 0.5 | Susceptible |
| Tobramycin | 8 | Resistant |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Colosimo, M.; Luciani, F.; Pullano, M.N.; Abrego-Guandique, D.M.; Gallelli, L. First Case of Chryseobacterium gleum Post-COVID-19 in a Child with Recurrent Fever. Reports 2024, 7, 90. https://doi.org/10.3390/reports7040090
Colosimo M, Luciani F, Pullano MN, Abrego-Guandique DM, Gallelli L. First Case of Chryseobacterium gleum Post-COVID-19 in a Child with Recurrent Fever. Reports. 2024; 7(4):90. https://doi.org/10.3390/reports7040090
Chicago/Turabian StyleColosimo, Manuela, Filippo Luciani, Maria Novella Pullano, Diana Marisol Abrego-Guandique, and Luca Gallelli. 2024. "First Case of Chryseobacterium gleum Post-COVID-19 in a Child with Recurrent Fever" Reports 7, no. 4: 90. https://doi.org/10.3390/reports7040090
APA StyleColosimo, M., Luciani, F., Pullano, M. N., Abrego-Guandique, D. M., & Gallelli, L. (2024). First Case of Chryseobacterium gleum Post-COVID-19 in a Child with Recurrent Fever. Reports, 7(4), 90. https://doi.org/10.3390/reports7040090








