Intradural Lumbar Disc Herniation: Updated Report of a Case with Literature Review
Abstract
:1. Introduction
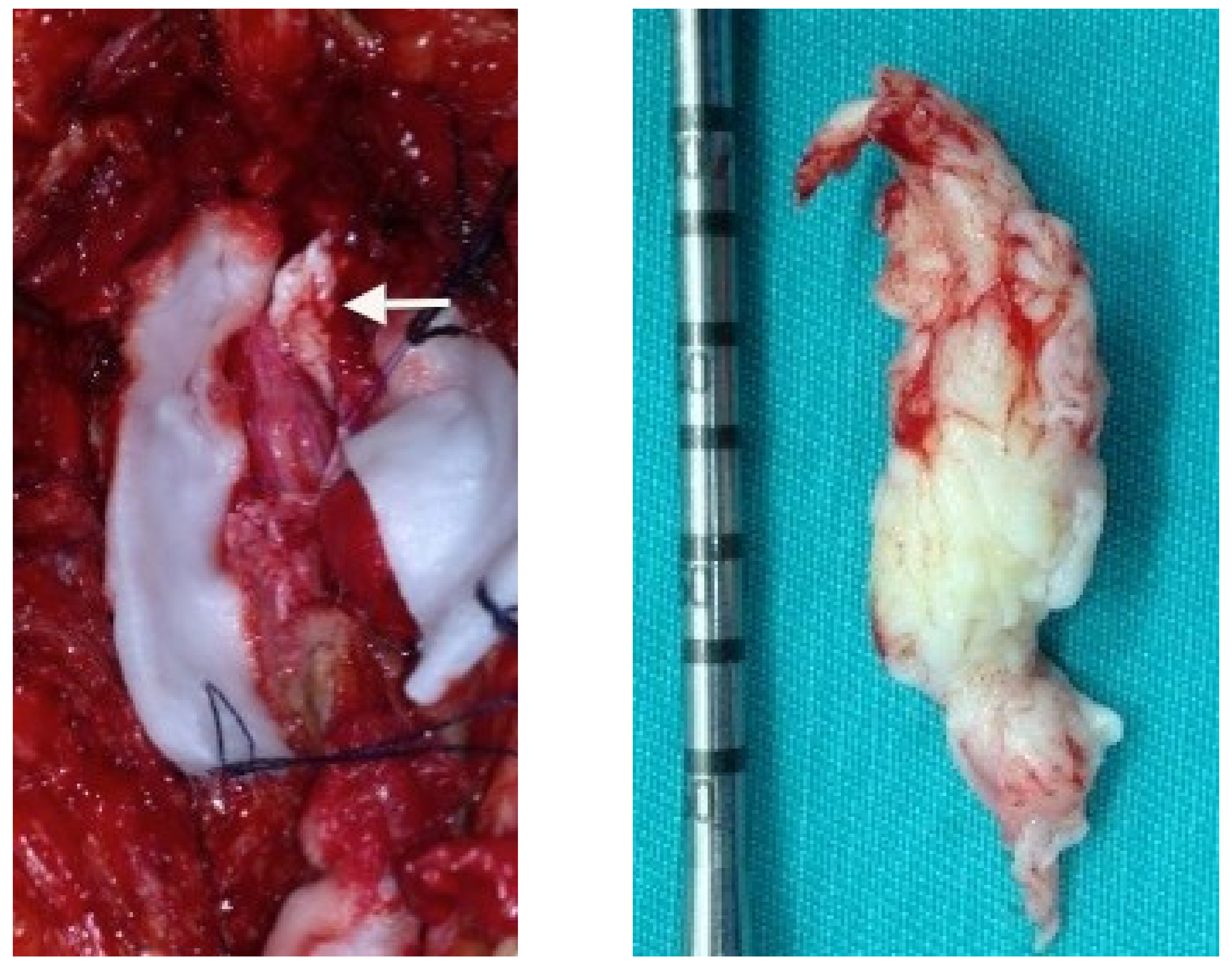
2. Case Presentation Section
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ihejirika, R.C.; Tong, Y.; Patel, K.; Protopsaltis, T. Intradural lumbar disc herniation: Illustrative case. J. Neurosurg. Case Lessons 2021, 2, CASE21336. [Google Scholar] [CrossRef]
- D’Andrea, G.; Trillò, G.; Roperto, R.; Celli, P.; Orlando, E.R.; Ferrante, L. Intradural lumbar disc herniations: The role of MRI in preoperative diagnosis and review of the literature. Neurosurg. Rev. 2004, 27, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Ducati, L.G.; Silva, M.V.; Brandão, M.M.; Romero, F.R.; Zanini, M.A. Intradural lumbar disc herniation: Report of five cases with literature review. Eur. Spine J. 2013, 22, 404–408. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tamaki, Y.; Sakai, T.; Miyagi, R.; Nakagawa, T.; Shimakawa, T.; Sairyo, K.; Chikawa, T. Intradural lumbar disc herniation after percutaneous endoscopic lumbar discectomy: Case report. J. Neurosurg. Spine 2015, 23, 336–339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J.; Ni, H.-J.; Xue, F.; Fan, Y.-S.; Li, X.-F.; Chen, X.-Z.; He, S.-S. Upper Lumbar Intradural Disc Herniation: A Rare Case Report and Etiologic Analysis. J. Pain Res. 2021, 14, 1475–1481. [Google Scholar] [CrossRef] [PubMed]
- Dandy, W.E. Serious Complications of Ruptured Intervertebral Disks. JAMA J. Am. Med. Assoc. 1942, 119, 474–477. [Google Scholar] [CrossRef]
- Hidalgo-Ovejero, Á.M.; García-Mata, S.; Gozzi-Vallejo, S.; Izco-Cabezón, T.; Martínez-Morentín, J.; Martínez-Grande, M. Intradural Disc Herniation and Epidural Gas: Something More Than a Casual Association? Spine 2004, 29, E463–E467. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.-C.; Huang, C.-T.; Lin, C.-M.; Liu, K.-N. Intradural disc herniation at L5 level mimicking an intradural spinal tumor. Eur. Spine J. 2011, 20, 326–329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sakai, T.; Tsuji, T.; Asazuma, T.; Yato, Y.; Matsubara, O.; Nemoto, K. Spontaneous resorption in recurrent intradural lumbar disc herniation: Case report. J. Neurosurg. Spine 2007, 6, 574–578. [Google Scholar] [CrossRef] [PubMed]
- Mut, M.; Berker, M.; Palaoğlu, S. Intraradicular disc herniations in the lumbar spine and a new classification of intradural disc herniations. Spinal Cord 2001, 39, 545–548. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rong, Y.; Wang, J.; Sui, T.; Liu, W.; Luo, Y.; Cai, W. Cervical intradural disc herniation with Brown-Séquard syndrome: Case report and literature review. J. Pain Res. 2019, 12, 2403–2410. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nam, K.H.; Han, I.H.; Cho, W.H.; Choi, B.K. A pure fluid-filled intradural cyst associated with intradural disc herniation and possible pathogenesis: A case report. Spine J. 2013, 13, e11–e15. [Google Scholar] [CrossRef] [PubMed]
- Guan, Q.; Xing, F.; Long, Y.; Xiang, Z. Cervical intradural disc herniation: A systematic review. J. Clin. Neurosci. 2018, 48, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Yildizhan, A.; Paşaoglu, A.; Ökten, T.; Ekinci, N.; Aycan, K.; Aral, O. Intradural disc herniations pathogenesis, clinical picture, diagnosis and treatment. Acta Neurochir. 1991, 110, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Blikra, G. Intradural Herniated Lumbar Disc. J. Neurosurg. 1969, 31, 676–679. [Google Scholar] [CrossRef] [PubMed]
- Mailleux, R.; Redant, C.; Milbouw, G. MR diagnosis of transdural disc herniation causing cauda equine syndrome. J. Belg. Radiol. 2006, 89, 303. [Google Scholar]
- Hida, K.; Iwasaki, Y.; Abe, H.; Shimazaki, M.; Matsuzaki, T. Magnetic resonance imaging of intradural lumbar disc herniation. J. Clin. Neurosci. 1999, 6, 345–347. [Google Scholar] [CrossRef]
- Han, I.-H.; Kim, K.S.; Jin, B.-H. Intradural Lumbar Disc Herniations Associated with Epidural Adhesion: Report of Two Cases. J. Korean Neurosurg. Soc. 2009, 46, 168–171. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.K.; Shrivastava, S.; Dulani, R.; Banode, P.; Gupta, S. Dorsal Herniation of Cauda Equina Due to Sequestrated Intradural Disc. Asian Spine J. 2012, 6, 145–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, H.-L.; Do, M.-H.; Vo, H.-L.; Nguyen, B.-T.L. Intradural Lumbar Disc Herniation: Updated Report of a Case with Literature Review. Reports 2022, 5, 9. https://doi.org/10.3390/reports5010009
Nguyen H-L, Do M-H, Vo H-L, Nguyen B-TL. Intradural Lumbar Disc Herniation: Updated Report of a Case with Literature Review. Reports. 2022; 5(1):9. https://doi.org/10.3390/reports5010009
Chicago/Turabian StyleNguyen, Hoang-Long, Manh-Hung Do, Hoang-Long Vo, and Bao-Tien L. Nguyen. 2022. "Intradural Lumbar Disc Herniation: Updated Report of a Case with Literature Review" Reports 5, no. 1: 9. https://doi.org/10.3390/reports5010009
APA StyleNguyen, H.-L., Do, M.-H., Vo, H.-L., & Nguyen, B.-T. L. (2022). Intradural Lumbar Disc Herniation: Updated Report of a Case with Literature Review. Reports, 5(1), 9. https://doi.org/10.3390/reports5010009







