Lymphoepithelial Carcinoma in the Lateral Tongue: The Case Report
Abstract
1. Introduction
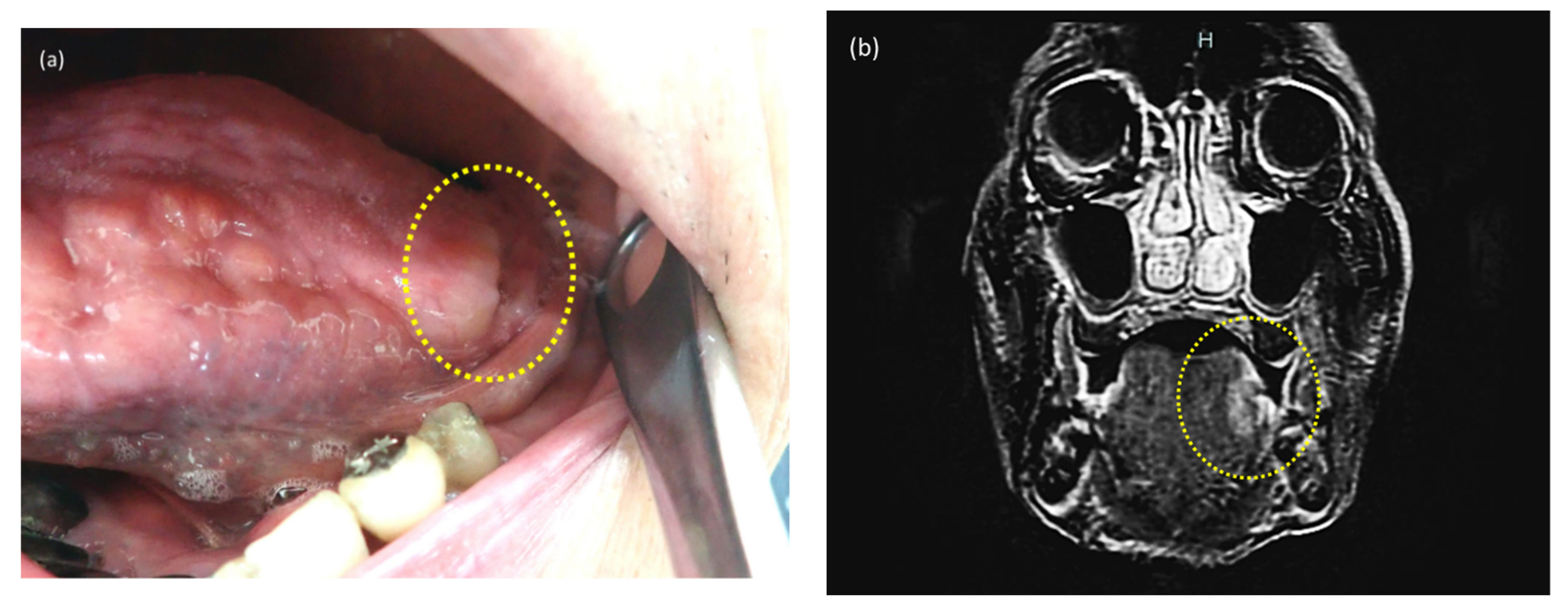
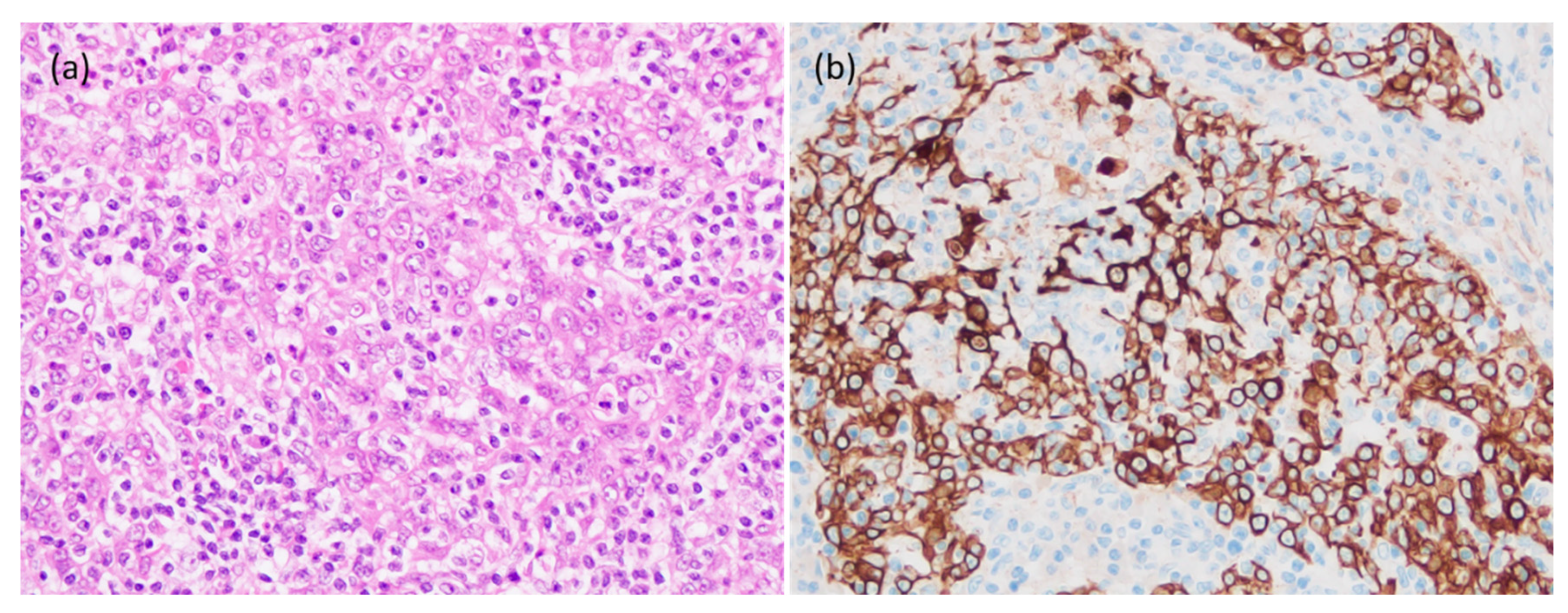
2. Case Report
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Rytkönen, A.E.; Hirvikoski, P.P.; Salo, T.A. Lymphoepithelial Carcinoma: Two Case Reports and a Systematic Review of Oral and Sinonasal Cases. Head Neck Pathol. 2011, 5, 327–334. [Google Scholar] [CrossRef]
- Schminke, A. Über lymphoepitheliale Geschwü. Beitr. Pathol. Anat. 1921, 68, 161–170. [Google Scholar]
- Ahuja, A.T.; Teo, P.M.; To, K.F.; King, A.D.; Metreweli, C. Palatal Lymphoepitheliomas and a review of head and neck lymphoepitheliomas. Clin. Radiol. 1999, 54, 289–293. [Google Scholar] [CrossRef]
- Chow, T.L.; Chow, T.K.; Lui, Y.H.; Sze, W.M.; Yuen, N.W.F.; Kwok, S.P.Y. Lymphoepithelioma-like carcinoma of oral cavity: Report of three cases and literature review. Int. J. Oral. Maxillofac. Surg. 2002, 31, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.Y.; Huang, C.C.; Hsiung, C.Y.; Eng, H.L.; Huang, H.Y. Primary lymphoepithelioma-like carcinoma of minor salivary gland: A case report with immunohistochemical and in situ hybridization studies. Head Neck. 2006, 28, 182–186. [Google Scholar] [CrossRef] [PubMed]
- Tanuja, S.; Brijesh, A.; Siddhartha, L.; Rajan, B.; Shubhada, K.; Purna, K. Epstein-Barr virus-associated lymphoepithelioma-like carcinoma of mandible. Pediatr. Dev. Pathol. 2009, 12, 152–155. [Google Scholar]
- Hsieh, M.Y.; Chen, Y.K.; Lin, L.M. Primary buccal lymphoepithelial carcinoma: Report of a case. Cases J. Taomfr. 2010, 2, 4–11. [Google Scholar]
- Zeng, M.; Li, S.; Fu, J.; Wu, H.; Gao, Y. Primary lymphoepithelial carcinoma of the intraoral minor salivary gland: A case report. Oncol. Lett. 2015, 9, 790–792. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Weiss, L.M.; Movahed, L.A.; Butler, A.E.; Swanson, S.A.; Frierson, H.F., Jr.; Cooper, P.H.; Colby, T.V.; Mills, S.E. Analysis of lymphoepithelioma and lymphoepithelioma-like carcinomas for Epstein-Barr viral genomes by in situ hybridization. Am. J. Surg. Pathol. 1989, 13, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Worley, N.K.; Daroca, P.J., Jr. Lymphoepithelial carcinoma of the minor salivary gland. Arch. Otolaryngol. Head Neck Surg. 1997, 123, 638–640. [Google Scholar] [CrossRef] [PubMed]
- Mahomed, F.; Grayson, W. A rare case of lymphoepithelial carcinoma of the lip. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2008, 105, e49–e52. [Google Scholar] [CrossRef] [PubMed]
- Dardo, M.; Luigi, L.; Massimiliano, M.; Cristian, C.; Mariarosaria, B.; Alfredo, D.; Alfonso, B. Intraoral lymphoepithelial carcinoma of the minor salivary glands. In Vivo 2012, 26, 1087–1089. [Google Scholar]
- Gultekin, M.; Sari, S.Y.; Gunhan, O.; Hosal, S.; Cengiz, M.; Gurkaynak, M. Lymphoepithelial carcinoma of the lower lip: Report of a case. Int. J. Hematol. Oncol. 2014, 24, 70–72. [Google Scholar] [CrossRef]
- Almeida, L.Y.; Silveira, H.A.; Silva, E.V.; Barbeiro, C.O.; Paula, J.A.; Bufalino, A.; Ribeiro-Silva, A.; León, J.E. EBV-negative lymphoepithelial-like carcinoma of the lower lip. Autops. Case Rep. 2019, 13, e2020138. [Google Scholar] [CrossRef] [PubMed]
- Takeda, D.; Shigeoka, M.; Sugano, T.; Yatagai, N.; Hasegawa, T.; Akashi, M. A Case Report of Tongue Lymphoepithelial Carcinoma with a Histological Diagnostic Dilemma. Diagnostics 2021, 11, 1039. [Google Scholar] [CrossRef] [PubMed]
- Hsiung, C.Y.; Huang, C.C.; Wang, C.J.; Huang, E.Y.; Huang, H.Y. Lymphoepithelioma-like carcinoma of salivary glands: Treatment results and failure patterns. Br. J. Radiol. 2006, 79, 52–55. [Google Scholar] [CrossRef] [PubMed]



| Study | Age (Years) | Gender | Country | EBV | Site | Size | Metastasis | Treatment | Follow-Up (Month) | Residual, Metastasis |
|---|---|---|---|---|---|---|---|---|---|---|
| Ahuja (1999) [3] | 63 | M | China | + | Roof of oral cavity | 2.5 cm | NM | NM | NM | NM |
| 47 | F | + | Palatinum | NM | cervical LN | NM | NM | NM | ||
| Chow (2002) [4] | 58 | M | China | + | Palatinum | 2.0 cm | cervical LN | R | 30 | No |
| 56 | F | + | Palatinum | 1.5 cm | No | R | 12 | No | ||
| 80 | F | + | Retromolar region | NM | cervical LN | patient refused | 34 | Died | ||
| Lu (2005) [5] | 50 | F | Taiwan | + | Minor salivary gland, cheek | 2 × 1.6 × 1 cm3 | No | S+R | 120 | No |
| Tanuja (2008) [6] | 11 | M | India | + | Mandible | NM | cervical LN | C + R | 36 | No |
| Hsieh (2010) [7] | 50 | M | Taiwan | + | Buccal mucosa | 2 cm | No | C + R | NM | residual tumor |
| Zeng (2015) [8] | 38 | F | China | + | Hard palate | 2.6 × 2.4 × 1.7 cm3 | No | S | 12 | No |
| Weiss (1989) [9] | 64 | M | United States of America | − | Floor of mouth | NM | NM | NM | NM | NM |
| Worley (1997) [10] | 69 | F | United States of America | − | subepithelial mass | 0.5 cm | cervical LN | S + R | 12 | No |
| in the left buccal area | ||||||||||
| Mahomed (2008) [11] | 73 | M | South Africa | − | Lower lip | 1 × 1 cm2 | No | S | 20 | No |
| Rytkönen (2011) [1] | 30 | M | Finland | − | Maxilla | NM | No | S + R | 11 | No |
| Dardo (2012) [12] | 56 | M | Italy | − | Minor salivary gland | 2.5 cm | No | S | 24 | No |
| and upper lip | ||||||||||
| Gultekin (2014) [13] | 41 | M | Turkey | − | Lower lip | 1 cm | cervical LN | C + R | 36 | No |
| Almeida (2019) [14] | 82 | F | Brasil | − | Lower lip | NM | No | S | 24 | No |
| Takeda (2021) [15] | 72 | F | Japan | − | left tongue edge | 1.2 × 0.6 cm2 | No | S | 12 | No |
| Present case | 82 | M | Japan | − | left tongue edge | 1.7 × 1.0 × 1.2 cm3 | No | S | 7 | No |
| Hsiung (2005) [16] | 50 | F | Taiwan | NM | Minor salivary gland | NM | No | S + R | 116.5 | NM |
| in right buccal area |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ono, S.; Marunaka, H.; Yanai, H.; Kawai, H.; Takabatake, K.; Nishida, K.; Toji, T.; Nakano, K.; Nagatsuka, H.; Yoshino, T. Lymphoepithelial Carcinoma in the Lateral Tongue: The Case Report. Reports 2021, 4, 24. https://doi.org/10.3390/reports4030024
Ono S, Marunaka H, Yanai H, Kawai H, Takabatake K, Nishida K, Toji T, Nakano K, Nagatsuka H, Yoshino T. Lymphoepithelial Carcinoma in the Lateral Tongue: The Case Report. Reports. 2021; 4(3):24. https://doi.org/10.3390/reports4030024
Chicago/Turabian StyleOno, Sawako, Hidenori Marunaka, Hiroyuki Yanai, Hotaka Kawai, Kiyofumi Takabatake, Kenji Nishida, Tomohiro Toji, Keisuke Nakano, Hitoshi Nagatsuka, and Tadashi Yoshino. 2021. "Lymphoepithelial Carcinoma in the Lateral Tongue: The Case Report" Reports 4, no. 3: 24. https://doi.org/10.3390/reports4030024
APA StyleOno, S., Marunaka, H., Yanai, H., Kawai, H., Takabatake, K., Nishida, K., Toji, T., Nakano, K., Nagatsuka, H., & Yoshino, T. (2021). Lymphoepithelial Carcinoma in the Lateral Tongue: The Case Report. Reports, 4(3), 24. https://doi.org/10.3390/reports4030024






