Transhepatic Vascular Access for Implantation of a Watchman Left Atrial Appendage Closure Device
Abstract
1. Introduction
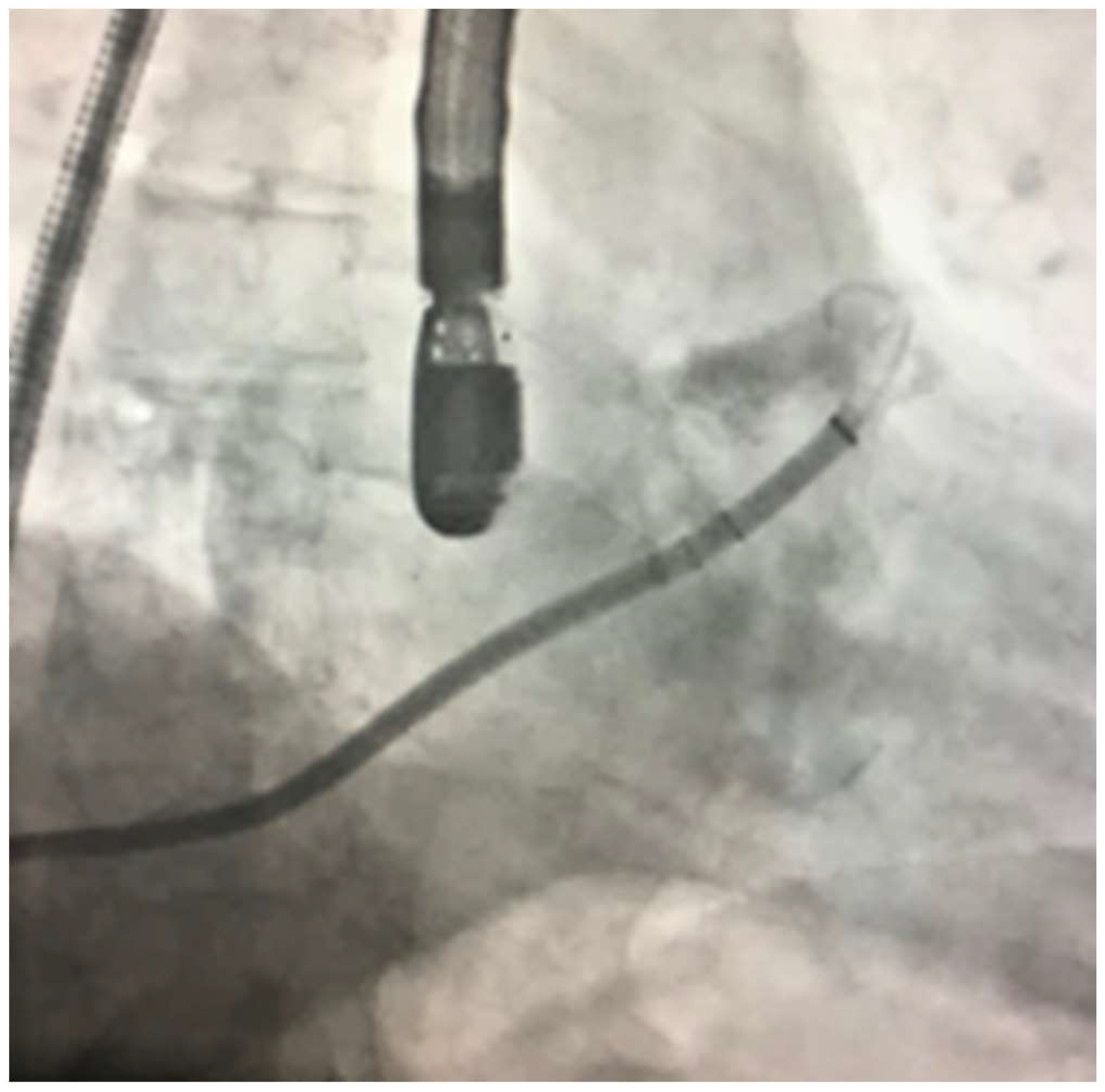
2. Case Report
3. Discussion
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| LAA | left atrial appendage |
| AF | atrial fibrillation |
| DVT | deep vein thrombosis |
| SVC | superior vena cava |
| RF | radiofrequency |
References
- Wunderlich, N.C.; Beigel, R.; Swaans, M.J.; Ho, S.Y.; Siegel, R.J. Percutaneous interventions for left atrial appendage exclusion: Options, assessment, and imaging using 2D and 3D echocardiography. JACC Cardiovasc. Imaging 2015, 8, 472–488. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.M.; Neuzil, P.; Skoka, J.; Kriz, R.; Popelova, J.; Love, B.A.; Mittnacht, A.J.; Reddy, V.Y. Percutaneous transhepatic venous access for catheter ablation procedures in patients with interruption of the inferior vena cava. Circ. Arrhythm. Electrophysiol. 2011, 4, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.T.; Gupta, R.; Kay, J.; Fagan, T.; Lowery, C.; Collins, K.K.; Sauer, W.H. Percutaneous transhepatic access for catheter ablation of cardiac arrhythmias. Europace 2013, 15, 494–500. [Google Scholar] [CrossRef] [PubMed]
- Ebeid, M.R. Transhepatic vascular access for diagnostic and interventional procedures: Techniques, outcome, and complications. Catheter. Cardiovasc. Interv. 2007, 69, 594–606. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.L.; Fellows, K.E.; Murphy, J.D. Transhepatic central venous access for cardiac catheterization and radiologic intervention. Cathet. Cardiovasc. Diagn. 1995, 35, 168–171. [Google Scholar] [CrossRef] [PubMed]
- Wallace, M.J.; Hovsepian, D.M.; Balzer, D.T. Transhepatic venous access for diagnostic and interventional cardiovascular procedures. J. Vasc. Interv. Radiol. 1996, 7, 579–582. [Google Scholar] [CrossRef]
- Stavropoulos, S.W.; Pan, J.J.; Clark, T.W.; Soulen, M.C.; Shlansky-Goldberg, R.D.; Itkin, M.; Trerotola, S.O. Percutaneous transhepatic venous access for hemodialysis. J. Vasc. Interv. Radiol. 2003, 14, 1187–1190. [Google Scholar] [CrossRef] [PubMed]
- Crummy, A.B.; Carlson, P.; McDermott, J.C.; Andrews, D. Percutaneous transhepatic placement of a Hickman catheter. AJR Am. J. Roentgenol. 1989, 153, 1317–1318. [Google Scholar] [CrossRef] [PubMed]
- Rajappan, K.; Sporton, S.C.; Schilling, R.J. Left atrial tachycardia and inferior vena cava thrombotic occlusion complicating atrial fibrillation ablation successfully treated from the right subclavian vein. Heart 2007, 93, 28. [Google Scholar] [CrossRef] [PubMed]
- Davenport, J.J.; Lam, L.; Whalen-Glass, R.; Nykanen, D.G.; Burke, R.P.; Hannan, R.; Zahn, E.M. The successful use of alternative routes of vascular access for performing pediatric interventional cardiac catheterization. Catheter. Cardiovasc. Interv. 2008, 72, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Emmel, M.; Sreeram, N.; Pillekamp, F.; Boehm, W.; Brockmeier, K. Transhepatic approach for catheter interventions in infants and children with congenital heart disease. Clin. Res. Cardiol. 2006, 95, 329–333. [Google Scholar] [PubMed]
- McLeod, K.A.; Houston, A.B.; Richens, T.; Wilson, N. Transhepatic approach for cardiac catheterisation in children: Initial experience. Heart 1999, 82, 694–696. [Google Scholar] [CrossRef] [PubMed]
- Book, W.M.; Raviele, A.A.; Vincent, R.N. Transhepatic vascular access in pediatric cardiology patients with occlusion of traditional central venous sites. J. Invasive Cardiol. 1999, 11, 341–344. [Google Scholar] [PubMed]
- Punamiya, K.; Beekman, R.H.; Shim, D.; Muller, D.W. Percutaneous transhepatic mitral commissurotomy. Cathet. Cardiovasc. Diagn. 1996, 39, 204–206. [Google Scholar] [CrossRef]
- Shim, D.; Lloyd, T.R.; Cho, K.J.; Moorehead, C.P.; Beekman, R.H., 3rd. Transhepatic cardiac catheterization in children. Evaluation of efficacy and safety. Circulation 1995, 92, 1526–1530. [Google Scholar] [CrossRef] [PubMed]
- Sommer, R.J.; Golinko, R.J.; Mitty, H.A. Initial experience with percutaneous transhepatic cardiac catheterization in infants and children. Am. J. Cardiol. 1995, 75, 1289–1291. [Google Scholar] [CrossRef]
- Erenberg, F.G.; Shim, D.; Beekman, R.H., 3rd. Intraperitoneal hemorrhage associated with transhepatic cardiac catheterization: A report of two cases. Cathet. Cardiovasc. Diagn. 1998, 43, 177–178. [Google Scholar] [CrossRef]


© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morcos, R.; Al Tahii, H.; Bansal, P.; Manam, R.; Maini, B. Transhepatic Vascular Access for Implantation of a Watchman Left Atrial Appendage Closure Device. Reports 2018, 1, 15. https://doi.org/10.3390/reports1020015
Morcos R, Al Tahii H, Bansal P, Manam R, Maini B. Transhepatic Vascular Access for Implantation of a Watchman Left Atrial Appendage Closure Device. Reports. 2018; 1(2):15. https://doi.org/10.3390/reports1020015
Chicago/Turabian StyleMorcos, Ramez, Haider Al Tahii, Priya Bansal, Rupesh Manam, and Brijeshwar Maini. 2018. "Transhepatic Vascular Access for Implantation of a Watchman Left Atrial Appendage Closure Device" Reports 1, no. 2: 15. https://doi.org/10.3390/reports1020015
APA StyleMorcos, R., Al Tahii, H., Bansal, P., Manam, R., & Maini, B. (2018). Transhepatic Vascular Access for Implantation of a Watchman Left Atrial Appendage Closure Device. Reports, 1(2), 15. https://doi.org/10.3390/reports1020015



