Quality of Life Measured with the WHO-5 Wellness Index during Wildfire Season in Two Canadian Provinces—Cross-Sectional Study
Abstract
1. Introduction
2. Methodology
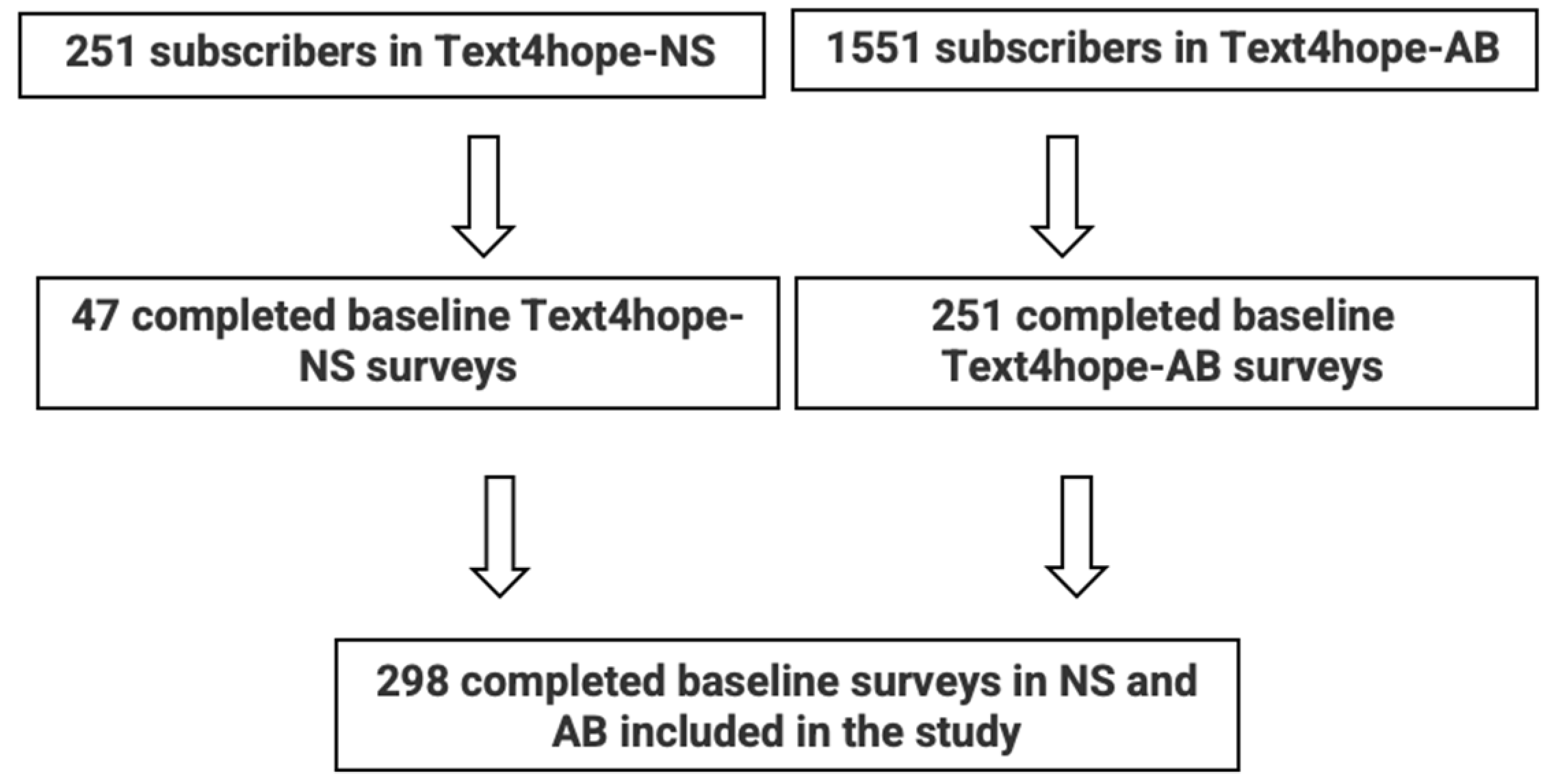
2.1. Study Setting and Design
2.2. Ethical Approval
2.3. Data Collection
2.4. Outcome Measure
2.5. Sample Size Estimation
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Morganstein, J.C.; Ursano, R.J. Ecological Disasters and Mental Health: Causes, Consequences, and Interventions. Front. Psychiatry 2020, 11, 1. [Google Scholar] [CrossRef]
- Ebi, K.L.; Vanos, J.; Baldwin, J.W.; Bell, J.E.; Hondula, D.M.; Errett, N.A.; Hayes, K.; Reid, C.E.; Saha, S.; Spector, J.; et al. Extreme Weather and Climate Change: Population Health and Health System Implications. Annu. Rev. Public Health 2021, 42, 293–315. [Google Scholar] [CrossRef]
- Masson-Delmotte, V. Global Warming of 1.5 °C: An IPCC Special Report on Impacts of Global Warming of 1.5 °C above Pre-Industrial Levels and Related Global Greenhouse Gas Emission Pathways, in the Contex of Strengthening the Global Response to the Thereat of Blimate Change, Sustainable Development, and Efforts to Eradicate Poverty; Cambridge University Press: Cambridge, UK, 2022. [Google Scholar]
- To, P.; Eboreime, E.; Agyapong, V.I.O. The Impact of Wildfires on Mental Health: A Scoping Review. Behav. Sci. 2021, 11, 126. [Google Scholar] [CrossRef] [PubMed]
- Carbon Credits. Wildfires Cost Over $148B and 30% of Emissions. 2023. Available online: https://carboncredits.com/wildfires-cost-emissions/#:~:text=According%20to%20the%20World%20Health,from%20suffocation%2C%20injuries%20and%20burns (accessed on 6 August 2023).
- Government of Canada. Cost of Wildland Fire Protection. 2021. Available online: https://natural-resources.canada.ca/climate-change/impacts-adaptations/climate-change-impacts-forests/forest-change-indicators/cost-fire-protection/17783 (accessed on 6 August 2023).
- NC State University. College of Natural Resources News. Why Canada’s Wildfires Are So Bad This Year. 2023. Available online: https://cnr.ncsu.edu/news/2023/07/why-canadas-wildfires-are-so-bad/#:~:text=While%20the%20Canadian%20wildfire%20season,the%20country’s%20National%20Forestry%20Database (accessed on 7 August 2023).
- Livewire Calgary. Wildfires Lead to Alberta Declaring State of Emergency. 2023. Available online: https://livewirecalgary.com/2023/05/06/wildfires-lead-to-alberta-declaring-state-of-emergency/#:~:text=Premier%20Danielle%20Smith%20declared%20the,of%20Albertans%2C%E2%80%9D%20she%20said (accessed on 7 August 2023).
- Nova Scotia. State of Emergency: Wildfires. 2023. Available online: https://beta.novascotia.ca/state-emergency-wildfires#:~:text=The%20Government%20of%20Nova%20Scotia,2023%20and%20can%20be%20renewed (accessed on 7 August 2023).
- Fergusson, D.M.; Horwood, L.J.; Boden, J.M.; Mulder, R.T. Impact of a Major Disaster on the Mental Health of a Well-Studied Cohort. JAMA Psychiatry 2014, 71, 1025–1031. [Google Scholar] [CrossRef] [PubMed]
- Agyapong, B.; Shalaby, R.; Eboreime, E.; Obuobi-Donkor, G.; Owusu, E.; Adu, M.; Mao, W.; Oluwasina, F.; Agyapong, V. Effects of cumulative trauma from multiple natural disasters. Eur. Psychiatry 2023, 66, S949. [Google Scholar] [CrossRef]
- Mao, W.; Eboreime, E.; Shalaby, R.; Nkire, N.; Agyapong, B.; Pazderka, H.; Obuobi-Donkor, G.; Adu, M.; Owusu, E.; Oluwasina, F.; et al. Post-Traumatic Stress Disorder in Fort McMurray: Prevalence and Correlates One Year After the Flood. Eur. Psychiatry 2023, 66, S477. [Google Scholar] [CrossRef]
- Neelam, K.; Duddu, V.; Anyim, N.; Neelam, J.; Lewis, S. Pandemics and pre-existing mental illness: A systematic review and meta-analysis. Brain Behav. Immun. Health 2021, 10, 100177. [Google Scholar] [CrossRef] [PubMed]
- Eisenman, D.P.; Galway, L.P. The mental health and well-being effects of wildfire smoke: A scoping review. BMC Public Health 2022, 22, 2274. [Google Scholar] [CrossRef]
- Teoli, D.; Bhardwaj, A. Quality Of Life. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK536962/ (accessed on 20 August 2023).
- World Health Organization. WHOQOL: Measuring Quality of Life. Available online: https://www.who.int/tools/whoqol (accessed on 20 August 2023).
- Hayes, K.; Berry, P.; Ebi, K.L. Factors Influencing the Mental Health Consequences of Climate Change in Canada. Int. J. Environ. Res. Public Health 2019, 16, 1583. [Google Scholar] [CrossRef]
- Johnston, D.W.; Önder, Y.K.; Rahman, M.H.; Ulubaşoğlu, M.A. Evaluating wildfire exposure: Using wellbeing data to estimate and value the impacts of wildfire. J. Econ. Behav. Organ. 2021, 192, 782–798. [Google Scholar] [CrossRef]
- Christianson, A.C.; McGee, T.K.; Whitefish Lake First Nation 459. Wildfire evacuation experiences of band members of Whitefish Lake First Nation 459, Alberta, Canada. Nat. Hazards 2019, 98, 9–29. [Google Scholar] [CrossRef]
- Agyapong, V.I.O.; Hrabok, M.; Juhas, M.; Omeje, J.; Denga, E.; Nwaka, B.; Akinjise, I.; Corbett, S.E.; Moosavi, S.; Brown, M.; et al. Prevalence Rates and Predictors of Generalized Anxiety Disorder Symptoms in Residents of Fort McMurray Six Months After a Wildfire. Front. Psychiatry 2018, 9, 345. [Google Scholar] [CrossRef] [PubMed]
- Mao, W.; Adu, M.; Eboreime, E.; Shalaby, R.; Nkire, N.; Agyapong, B.; Pazderka, H.; Obuobi-Donkor, G.; Owusu, E.; Oluwasina, F.; et al. Post-Traumatic Stress Disorder, Major Depressive Disorder, and Wildfires: A Fifth-Year Postdisaster Evaluation among Residents of Fort McMurray. Int. J. Environ. Res. Public Health 2022, 19, 9759. [Google Scholar] [CrossRef]
- Papanikolaou, V.; Adamis, D.; Kyriopoulos, J. Long term quality of life after a wildfire disaster in a rural part of Greece. Open J. Psychiatry 2012, 2, 164–170. [Google Scholar] [CrossRef]
- De Pretto, L.; Acreman, S.; Ashfold, M.J.; Mohankumar, S.K.; Campos-Arceiz, A. The Link between Knowledge, Attitudes and Practices in Relation to Atmospheric Haze Pollution in Peninsular Malaysia. PLoS ONE 2015, 10, e0143655. [Google Scholar] [CrossRef] [PubMed]
- Felix, E.D.; Afifi, W. The Role of Social Support on Mental Health after Multiple Wildfire Disasters. J. Community Psychol. 2015, 43, 156–170. [Google Scholar] [CrossRef]
- World Health Organization. Mental Health in Emergencies. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-health-in-emergencies (accessed on 29 October 2023).
- Statistics Canada. Population Estimates, Quarterly. 2023. Available online: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000901 (accessed on 20 August 2023).
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Bech, P. Health-related quality of life measurements in the assessment of pain clinic results. Acta Anaesthesiol. Scand. 1999, 43, 893–896. [Google Scholar] [CrossRef]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A Systematic Review of the Literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef]
- Psychiatric Research Unit. WHO Collaborating Centre in Mental Health. WHO (Five) Well-Being Index (1998 version). Available online: https://www.psykiatri-regionh.dk/who-5/Documents/WHO-5%20questionaire%20-%20English.pdf (accessed on 14 July 2023).
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 2020, 15, e0231924. [Google Scholar]
- Statistics Canada. Population and Dwelling Counts: Canada, Provinces and Territories. 2022. Available online: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=9810000101 (accessed on 8 July 2023).
- IBM Corp. IBM SPSS Statistics for Macintosh, version 28.0; IBM Corp.: Armonk, NY, USA, 2021. [Google Scholar]
- Diener, E.; Oishi, S.; Lucas, R.E. Personality, culture, and subjective well-being: Emotional and cognitive evaluations of life. Annu. Rev. Psychol. 2003, 54, 403–425. [Google Scholar] [CrossRef] [PubMed]
- Ngamaba, K.H.; Panagioti, M.; Armitage, C.J. How strongly related are health status and subjective well-being? Systematic review and meta-analysis. Eur. J. Public Health 2017, 27, 879–885. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.R.G.; Agyapong, V.; Greenshaw, A.J.; Cribben, I.; Brett-MacLean, P.; Drolet, J.; McDonald-Harker, C.; Omeje, J.; Mankowsi, M.; Noble, S.; et al. After the Fort McMurray wildfire there are significant increases in mental health symptoms in grade 7-12 students compared to controls. BMC Psychiatry 2019, 19, 18. [Google Scholar]
- SCIAM. Wildfires and Smoke Are Harming People’s Mental Health. Here’s How to Cope. Available online: https://www.scientificamerican.com/article/wildfires-and-smoke-are-harming-peoples-mental-health-heres-how-to-cope/ (accessed on 20 January 2024).
- British Columbia. Wildfire Season Summary. Available online: https://www2.gov.bc.ca/gov/content/safety/wildfire-status/about-bcws/wildfire-history/wildfire-season-summary (accessed on 20 January 2024).
- Humphreys, A.; Walker, E.G.; Bratman, G.N.; Errett, N.A. What can we do when the smoke rolls in? An exploratory qualitative analysis of the impacts of rural wildfire smoke on mental health and wellbeing, and opportunities for adaptation. BMC Public Health 2022, 22, 41. [Google Scholar] [CrossRef] [PubMed]
- Simpson, D.M. Non-institutional sources of assistance following a disaster: Potential triage and treatment capabilities of neighborhood-based preparedness organizations. Prehosp. Disaster Med. 2000, 15, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Committee on Post-Disaster Recovery of a Community’s Public Health, Medical, and Social Services. Healthy, Resilient, and Sustainable Communities After Disasters: Strategies, Opportunities, and Planning for Recovery; National Academies Press (US): Washington, DC, USA, 2015. [Google Scholar]
- ResilienceNHope Suite of Supportive Text Messaging Programs Reduce Stress, Anxiety and Depression. Available online: https://www.youtube.com/watch?v=KmaPyjCNtio (accessed on 4 November 2023).
- Bhattacharjee, A.; Pang, J.; Liu, A.; Mariakakis, A.; Williams, J.J. Design Implications for One-Way Text Messaging Services that Support Psychological Wellbeing. ACM Trans. Comput.-Hum. Interact. 2023, 30, 1–29. [Google Scholar] [CrossRef]
- Shalaby, R.; Spurvey, P.; Knox, M.; Rathwell, R.; Vuong, W.; Surood, S.; Urichuk, L.; Snaterse, M.; Greenshaw, A.J.; Li, X.-M.; et al. Clinical Outcomes in Routine Evaluation Measures for Patients Discharged from Acute Psychiatric Care: Four-Arm Peer and Text Messaging Support Controlled Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 3798. [Google Scholar] [CrossRef]
- Agyapong, V.I.O.; Hrabok, M.; Vuong, W.; Shalaby, R.; Noble, J.M.; Gusnowski, A.; Mrklas, K.J.; Li, D.; Urichuk, L.; Snaterse, M.; et al. Changes in Stress, Anxiety, and Depression Levels of Subscribers to a Daily Supportive Text Message Program (Text4Hope) During the COVID-19 Pandemic: Cross-Sectional Survey Study. JMIR Ment. Health 2020, 7, e22423. [Google Scholar] [CrossRef]
- Agyapong, V.I.O.; Shalaby, R.; Hrabok, M.; Vuong, W.; Noble, J.M.; Gusnowski, A.; Mrklas, K.; Li, D.; Snaterse, M.; Surood, S.; et al. Mental Health Outreach via Supportive Text Messages during the COVID-19 Pandemic: Improved Mental Health and Reduced Suicidal Ideation after Six Weeks in Subscribers of Text4Hope Compared to a Control Population. Int. J. Environ. Res. Public Health 2021, 18, 2157. [Google Scholar] [CrossRef]
- Obuobi-Donkor, G.; Shalaby, R.; Vuong, W.; Agyapong, B.; Hrabok, M.; Gusnowski, A.; Surood, S.; Greenshaw, A.J.; Agyapong, V.I. Effects of Text4Hope-Addiction Support Program on Cravings and Mental Health Symptoms: Results of a Longitudinal Cross-sectional Study. JMIR Form. Res. 2023, 7, e40440. [Google Scholar] [CrossRef]
- Shalaby, R.; Adu, M.K.; El Gindi, H.M.; Agyapong, V.I.O. Text Messages in the Field of Mental Health: Rapid Review of the Reviews. Front. Psychiatry 2022, 13, 921982. [Google Scholar] [CrossRef] [PubMed]
- Shalaby, R.; Vuong, W.; Hrabok, M.; Gusnowski, A.; Mrklas, K.; Li, D.; Snaterse, M.; Surood, S.; Cao, B.; Li, X.-M.; et al. Gender Differences in Satisfaction With a Text Messaging Program (Text4Hope) and Anticipated Receptivity to Technology-Based Health Support During the COVID-19 Pandemic: Cross-sectional Survey Study. JMIR Mhealth Uhealth 2021, 9, e24184. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. Fire Incidents Increase During the Pandemic. 2023. Available online: https://www150.statcan.gc.ca/n1/daily-quotidien/230608/dq230608a-eng.htm (accessed on 7 August 2023).
| Variables | High-School or Less Education n (%) | Post-Secondary Education n (%) | Total n (%) |
|---|---|---|---|
| Province | |||
| NS | 7 (13.7) | 40 (16.3) | 47 (15.8) |
| AB | 44 (86.3) | 206 (83.7) | 250 (84.2) |
| Age | |||
| Mean (SD) | 44.71 (18.83) | 49.15 (12.60) | 48.38 (13.93) |
| Age categories | |||
| ≥60 y | 13 (25.5) | 59 (24.0) | 72 (24.2) |
| 50–59 | 12 (23.5) | 68 (27.6) | 80 (26.9) |
| 40–49 | 8 (15.7) | 53 (21.5) | 61 (20.5) |
| ≤40 y | 18 (35.3) | 66 (26.8) | 84 (28.3) |
| Gender | |||
| Male | 14 (27.5) | 24 (9.8) | 38 (12.8) |
| Female | 37 (72.5) | 216 (87.8) | 253 (85.2) |
| Other | 0 (0.0) | 6 (2.4) | 6 (2.0) |
| Ethnicity | |||
| Caucasian | 36 (70.6) | 212 (86.2) | 248 (83.5) |
| Indigenous | 7 (13.7) | 11 (4.5) | 18 (6.1) |
| Asian | 3 (5.9) | 8 (3.3) | 11 (3.7) |
| Black/Hispanic | 1 (2.0) | 8 (3.3) | 9 (3.0) |
| Other | 4 (7.8) | 7 (2.8) | 11 (3.7) |
| Relationship status | |||
| In a relationship | 15 (29.4) | 152 (62.0) | 167 (56.4) |
| Not in a relationship | 36 (70.6) | 93 (38.0) | 129 (43.6) |
| Employment status | |||
| Employed | 27 (52.9) | 162 (65.9) | 189 (63.6) |
| Unemployed | 24 (47.1) | 84 (34.1) | 108 (36.4) |
| History of having mental health diagnosis from a health professional * | |||
| Depression | 30 (58.8) | 138 (56.1) | 168 (56.6) |
| Anxiety | 29 (56.9) | 128 (52.0) | 157 (52.9) |
| History of receiving psychotropic medications * | |||
| Antidepressants | 23 (45.1) | 93 (37.8) | 116 (39.1) |
| Benzodiazepines | 5 (9.8) | 11 (4.5) | 16 (5.4) |
| Living in a region of AB/NS that has recently been impacted by the wildfires | |||
| No | 34 (66.7) | 151 (61.4) | 185 (62.3) |
| Yes | 17 (33.3) | 95 (38.6) | 112 (37.7) |
| Having had to evacuate from home due to the recent wildfires in AB/NS | |||
| No | 11 (64.7) | 77 (81.1) | 88 (78.6) |
| Yes | 6 (35.3) | 18 (18.9) | 24 (21.4) |
| Having lost any property as a result of the wildfire | |||
| No | 15 (88.2) | 94 (98.9) | 109 (97.3) |
| Yes | 2 (11.8) | 1 (1.1) | 3 (2.7) |
| Having received support from family and friends in relation to the recent wildfires | |||
| Some-to-absolute support | 7 (41.2) | 44 (46.3) | 51 (45.5) |
| Limited-to-no support | 10 (58.8) | 51 (53.7) | 61 (54.5) |
| Having received support from the government of Alberta in relation to the recent wildfires | |||
| Some-to-absolute support | 2 (11.8) | 17 (17.9) | 19 (17.0) |
| Limited-to-no support | 15 (88.2) | 78 (82.1) | 93 (83.0) |
| Having received support from the Red Cross in relation to the recent wildfires | |||
| Some-to-absolute support | 2 (11.8) | 4 (4.3) | 6 (5.4) |
| Limited-to-no support | 15 (88.2) | 90 (95.7) | 105 (94.6) |
| Watching television images about the devastation caused by the recent wildfires in AB/NS | |||
| Less frequent (Maximum once/week) | 21 (42.0) | 112 (45.5) | 133 (44.9) |
| More frequent (At least every other day) | 29 (58.0) | 134 (54.5) | 163 (55.1) |
| WHO-5 | |||
| Mean (SD) | 38.70 (25.21) | 41.14 (19.86) | 40.79 (20.69) |
| Variables | Low QOL | |||
|---|---|---|---|---|
| Prevalence N (%) | Adjusted Odd’s Ratio (95% CI) | |||
| Overall | 171 (67.3) | |||
| Province |  | |||
| NS | 31 (70.5) | 1 (Ref) | ||
| AB | 140 (66.7) | 0.66 (0.28–1.59) | ||
| Age categories |  | |||
| ≥60 y | 36 (59.0) | 1 (Ref) | ||
| 50–59 | 46 (70.8) | 1.78 (0.75–4.23) | ||
| 40–49 | 37 (67.3) | 1.63 (0.67–3.98) | ||
| ≤40 y | 52 (71.2) | 1.24 (0.53–2.91) | ||
| Gender |  | |||
| Male | 19 (63.3) | 1 (Ref) | ||
| Female | 147 (67.4) | 1.32 (0.53–3.25) | ||
| Other | 5 (83.3) | 1.92 (0.17–21.56) | ||
| Ethnicity |  | |||
| Caucasian | 141 (65.9) | 1 (Ref) | ||
| Indigenous | 11 (68.8) | 0.99 (0.30–3.30) | ||
| Asian | 7 (70.0) | 1.67 (0.37–7.55) | ||
| Black/Hispanic | 6 (85.7) | 2.55 (0.26–24.98) | ||
| Other | 6 (85.7) | 2.45 (0.24–24.85) | ||
| Education level |  | |||
| High School or Lower Education | 26 (70.3) | 1 (Ref) | ||
| Post-secondary Education | 145 (66.8) | 1.08 (0.45–2.59) | ||
| Relationship status |  | |||
| In a relationship | 91 (62.3) | 1 (Ref) | ||
| Not in a relationship | 80 (74.1) | 1.46 (0.79–2.70) | ||
| Employment status |  | |||
| Employed | 107 (64.1) | 1 (Ref) | ||
| Unemployed | 64 (73.6) | 1.71 (0.87–3.38) | ||
| History of having mental health diagnosis of depression from a health professional |  | |||
| No | 60 (57.7) | 1 (Ref) | ||
| Yes | 111 (74.0) | 1.93 (0.95–3.90) | ||
| History of having mental health diagnosis of anxiety from a health professional | ||||
| No | 64 (58.2) | 1 (Ref) | ||
| Yes | 107 (74.3) | 1.49 (0.79–2.81) | ||
| History of receiving Antidepressant medications * |  | |||
| No | 97 (64.2) | 1 (Ref) | ||
| Yes | 74 (71.8) | 0.97 (0.49–1.95) | ||
| History of receiving Benzodiazepines medications | ||||
| No | 157 (65.7) | 1 (Ref) | ||
| Yes | 14 (93.3) | 4.12 (0.49–34.54) | ||
| Living in a region of AB/NS that has recently been impacted by the wildfires |  | |||
| No | 97 (62.6) | 1 (Ref) | ||
| Yes | 74 (74.7) | 1.96 (1.05–3.65) | ||
| Watching television images about the devastation caused by the recent wildfires in AB/NS | ||||
| Maximum once/week | 85 (72.6) | 1 (Ref) | ||
| At least every other day | 86 (62.8) | 0.60 (0.32–1.10) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shalaby, R.; Agyapong, B.; Obuobi-Donkor, G.; da Luz Dias, R.; Agyapong, V.I.O. Quality of Life Measured with the WHO-5 Wellness Index during Wildfire Season in Two Canadian Provinces—Cross-Sectional Study. Fire 2024, 7, 39. https://doi.org/10.3390/fire7020039
Shalaby R, Agyapong B, Obuobi-Donkor G, da Luz Dias R, Agyapong VIO. Quality of Life Measured with the WHO-5 Wellness Index during Wildfire Season in Two Canadian Provinces—Cross-Sectional Study. Fire. 2024; 7(2):39. https://doi.org/10.3390/fire7020039
Chicago/Turabian StyleShalaby, Reham, Belinda Agyapong, Gloria Obuobi-Donkor, Raquel da Luz Dias, and Vincent I. O. Agyapong. 2024. "Quality of Life Measured with the WHO-5 Wellness Index during Wildfire Season in Two Canadian Provinces—Cross-Sectional Study" Fire 7, no. 2: 39. https://doi.org/10.3390/fire7020039
APA StyleShalaby, R., Agyapong, B., Obuobi-Donkor, G., da Luz Dias, R., & Agyapong, V. I. O. (2024). Quality of Life Measured with the WHO-5 Wellness Index during Wildfire Season in Two Canadian Provinces—Cross-Sectional Study. Fire, 7(2), 39. https://doi.org/10.3390/fire7020039







