1. Introduction
Glass-ceramics, polycrystalline ceramics, and resin-matrix ceramics are the most frequently used materials for prosthodontic restorations [
1]. Glass-ceramics are widely used in dentistry as restorative materials for different applications such as crowns, inlays, onlays, and veneers. The success of glass-ceramic dental restorations is in part due to their excellent mechanical and biocompatibility properties [
2,
3,
4]. One of the subcategories of glass-ceramics is synthetic ceramics which include lithium silicate and its derivatives: lithium disilicate, lithium alumina-silicate, and zirconia reinforced lithium silicates. The first generation of LSGC introduced to the dental market was IPS Empress II (Ivoclar-Vivadent, Liechtenstein, Schaan, Liechtenstein) in 1998. The development of computer-aided design and computer-aided manufacturing (CAD/CAM) technology led to the introduction of another generation of CAD-CAM LSGC called IPS e.max CAD in 2006. IPS e.max CAD is popular for use in both single- and multiple-unit indirect restorations due to its high mechanical strength (~360 MPa), excellent esthetic properties, and good clinical success [
5]. In addition, CAD/CAM technology allows the dentist to prepare and deliver an indirect restoration in one appointment [
6]. Recently, two new CAD/CAM glass-ceramic materials were introduced to the dental market: (1) zirconia reinforced lithium silicate glass ceramics: Vita Suprinity
®, and Celtra Duo
® (from Vita Zahnfabrick, Bad Säckingen, Germany and Dentsply DeTrey Hanau-Wolfgang, Germany respectively); and (2) lithium alumina silicate reinforced with lithium disilicate: n!ce (from Strauman, Basel, Switzerland). Both Vita Suprinity and Celtra Duo ceramics are enriched with zirconia (≈10% by weight). They claim to be the first zirconia reinforced LSDC [
3]. Like e.max CAD, Vita Suprinity is supplied in a precrystalline stage suitable for milling procedures and is crystallized following the milling procedure. Celtra Duo and n!ce are provided as fully sintered blocks. Celtra Duo may be heat treated to improve its mechanical properties [
7,
8]. According to the manufacturers, both Celtra Duo and n!ce can be immediately seated and cemented after fabrication with a CAD/CAM system.
The quality of the ceramic–resin bonding is a key factor for clinical success. The ceramic-resin interface is subjected to the moist oral environment and functional forces present in the oral cavity. The adhesion at the ceramic–resin interface is the result of a physicochemical interaction across the interface involving the adhesive and the ceramic surface [
9,
10]. A durable bond between the resin cement and glass-ceramic restoration is obtained by two mechanisms: micromechanical retention provided by different surface treatments, such as acid etching or sand-blasting with Al
2O
3 or a combination of any two of these methods [
9,
11]. The second mechanism is the chemical bonding provided by a silane coupling agent [
12].
The LSDG microstructure has two phases, a glassy matrix phase (silica) and a crystals phase. The glassy matrix phase contributes to micromechanical bonding as certain surface treatments can affect the glassy matrix. Specifically, hydrofluoric acid etching and aluminum-oxide particle sand-blasting of the ceramic surface produces microporosities that contribute to micromechanical bonding [
11]. These microporosities increase the surface area and expose and generate hydroxyl groups on the ceramic surface that are responsible for chemical bonding via silane coupling agents [
13]. The crystals phase (lithium disilicate oxide, Li
2Si
2O
5) is responsible for its mechanical properties and ceramic strength [
14].
Scanning electron microscopy (SEM) is a valuable tool to investigate the morphology and microstructural changes of glass-ceramic surfaces [
15]. Atomic force microscopy (AFM) is used in biomaterial science to provide a quantitative measurement of surface roughness and it describes the topography of the biomaterial surface with less effort of sample preparation [
16,
17]. Although surface treatments of lithium disilicate-based glass-ceramic of the pressed technique have been studied previously, the CAD/CAM LSGC such as IPS e.max CAD, Vita Suprinity
®, Celtra Duo
®, and n!ce have not been fully investigated.
An optimal glass-ceramic surface treatment has not been confirmed as yet. This study aims to evaluate the effect of sand-blasting with aluminum oxide (Al2O3), etching with 5% hydrofluoric acid, and the use of a combination of sand-blasting and hydrofluoric acid treatment on the surface roughness of IPS e. max® CAD, Vita Suprinity®, Celtra Duo®, and n!ce. The null hypothesis is that different surface treatments would not affect the surface roughness and micromorphology of four CAD/CAM lithium silicate glass-ceramics.
2. Materials and Methods
Eighty specimens of four different types of lithium disilicate-based glass-ceramics (see
Table 1) were selected for this study, 20 specimens of each of the four materials (
n = 5).
CAD/CAM ceramic blocks were sectioned into rectangular slices with a 2 mm height, using a low-speed saw diamond (Isomet1000, Buehler Ltd., Lake Bluff, IL, USA). IPS—e.max CAD and Vita Suprinity specimens were cleaned with ethanol for 2 min and then ultrasonically cleaned in distilled water for 15 min. Thereafter it was sintered in a furnace according to the firing program recommended by the manufacturer. Celtra Duo and n!ce specimens are fabricated from fully crystallized lithium disilicate-based glass-ceramic blocks and they do not need additional sinterization. To obtain a smooth flat surface, all specimens were polished on wet 400, 600 and 1200 grit size silicon carbide paper (Buehler Ltd., Lake Bluff, IL, USA) and then polished with a 3 µm and 1 µm polycrystalline diamond suspension liquid (Buehler Ltd., Lake Bluff, IL, USA) on a grinding device. The samples were then cleaned with ethanol for 2 min and placed in an ultrasonic machine (Branson cleaning equipment company, Shelton, CT, USA) for 15 min. The ceramic specimens were labeled on the treated surfaces and then randomly assigned to four treatment groups.
Group C. No treatment applied to the ceramic surfaces. This group served as a control.
Group SB. Sandblasted: labeled surfaces of ceramic specimens were sandblasted (Al2O3; Perlablast® Micro; Bego, Bremen, Germany) with 50 µm Al2O3 at 70 psi for 10s. Specimens were held at a distance of 20 mm between the surface of the specimen and the blasting tip to ensure an equal distance for each specimen. Following sand-blasting, the specimens were rinsed under running water for the 20s and then dried for 20s with oil-free compressed air.
Group HF. Hydrofluoric acid-etched: labeled surfaces of ceramic specimens etched with 5% hydrofluoric acid for 20s (e.max CAD, Vita Suprinity, and n!ce) and 30s (Celtra Duo) based on manufacturer recommendations for each type. The etching gel was removed under running water for 20s then dried for 20s with oil-free compressed air.
Group S + E. Sandblasted and hydrofluoric acid-etched: in this group, the specimens were first sandblasted with 50 um Al2O3 at 70 psi for 10s. After cleaning, the specimens were etched with 5% hydrofluoric acid for 20s and then cleaned under running water for 20s followed by drying.
All specimens were then cleaned with ethanol and subjected to ultrasonic treatment in distilled water to remove any surface residues and then dried with free compressed oil.
Topographic Analyses
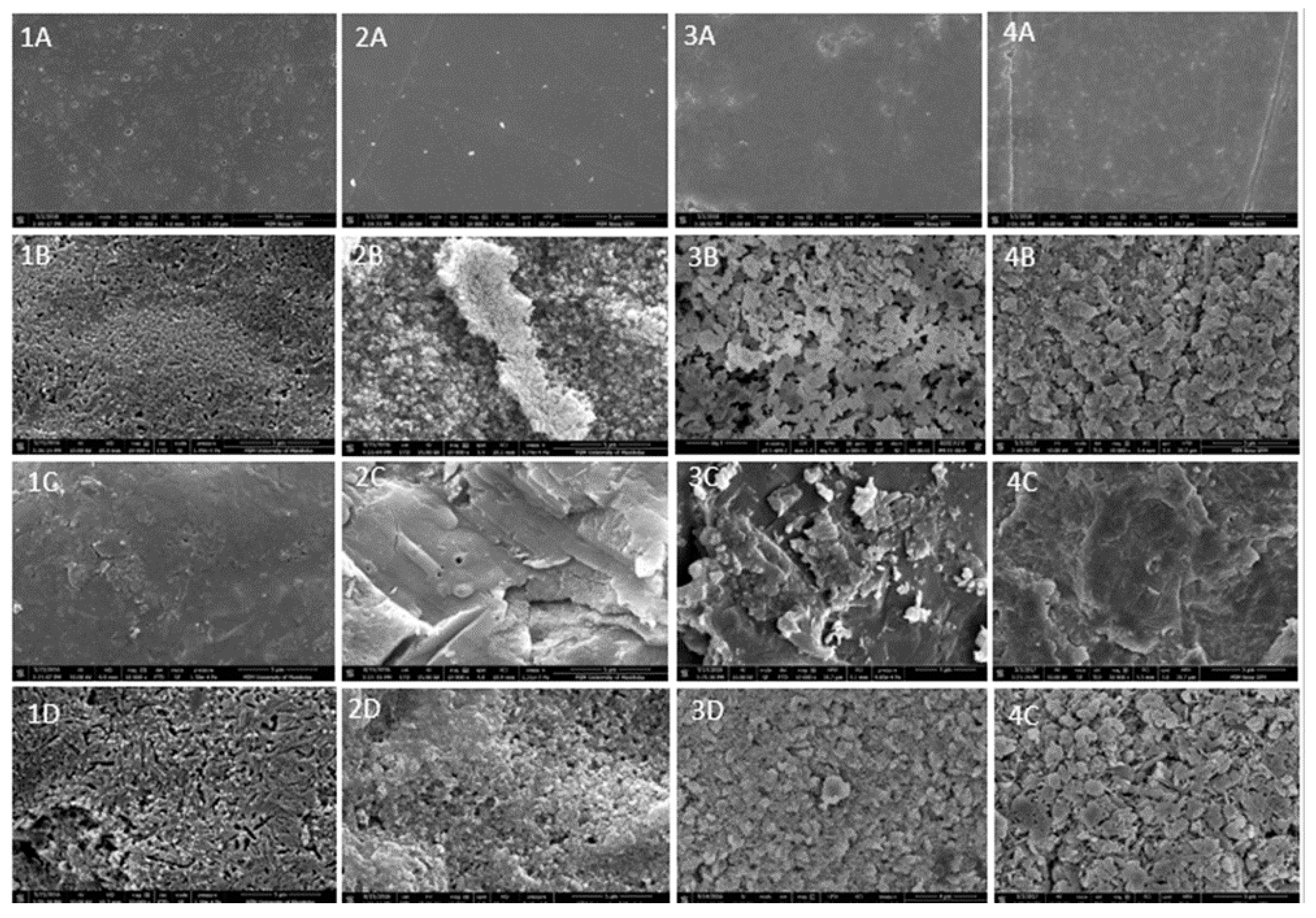
Scanning electron microscopy: All ceramic specimens were coated with gold and loaded in an SEM unit (ThermoFisher, OR, USA). All SEM images were captured at 10,000× magnification.
Atomic force microscopy: All ceramic specimens were evaluated under AFM Multimode nanoscope IIIa, Digital Instruments (Veeco metrology group, Santa Barbara, CA, USA). Images were taken in tapping mode at 50 µm × 50 µm scan size with a slow scan rate (0.1 Hz). The average surface roughness (Ra) of the ceramic after different surface treatments was recorded as a numeric value (in nanometer) using appropriate software (Nanoscope v613R1).
Statistical Analysis: Data were analyzed using a two-way ANOVA with α = 0.05. The means were analyzed for contrast using Tukey’s post hoc test.
3. Results
Figure 1 displays the SEM images of the effect of the surface treatments on the four LDGC. SEM images for HF specimens had a honeycomb shape for Celta and n!ce (
Figure 1(3B,4B)), and a needle shape for e.max CAD (
Figure 1(1B)) and Vita Suprinity (
Figure 1(2B)). Means and standard deviations for the roughness Ra (nm) of four CAD/CAM LDGC were extrapolated from the AFM digital images and are displayed in
Table 2. Sand-blasting created significantly higher mean roughness values (
p < 0.05) compared to other surface treatments for Vita Suprinity and Celtra Duo (867.8 nm) and (609.6 nm) respectively. However, sand-blasting and S + E had no significant difference for e.max CAD and n!ce. Although hydrofluoric acid demonstrated less roughness than other surface treatments, it changed the micromorphology and produces microporosities on the surface of all four ceramic types.
Figure 2 displays the AFM images of the surface at the nanolevel. Our results showed that hydrofluoric acid reduced the surface roughness by more than 50% when applied after sand-blasting (
Figure 3). This was true for both Vita Suprinity and Celtra Duo. However, there was a slight increase in the roughness after sand-blasting for e.max CAD and n!ce.
4. Discussion
A reliable bond between resin cement and glass-ceramic restorations contributes to the longevity of glass-ceramic restorations and their overall clinical success [
18]. Several studies focused on cement selection and the use of silane coupling agents to improve the bonding between resin cement and glass-ceramic [
19,
20,
21,
22]. However, there are many LSGC used for the fabrication of indirect dental restorations and still lacking supportive evidence for its functionality. The ideal clinical protocol for predictable bonding between resin cement and lithium disilicate-based glass-ceramic restoration remains undetermined. The surface treatment of glass-ceramic restorations before cementation is an essential step to improve the clinical performance of LSGC restorations. Increasing the surface roughness of the intaglio surface of restorations increases the bonding area and improves mechanical retention. It also decreases the surface tension to create the desired interlocking retention with resin cement. This laboratory study investigated the effect of different surface treatments on the micromorphology and roughness of four CAM/CAM LSGC. The null hypothesis of the present study was rejected, since, different surface treatments significantly increased the roughness and changed the micromorphology.
The application of hydrofluoric acid increased roughness and changed the micromorphology of all four types of LSGC. This occurred due to the chemical interaction between hydrofluoric acid and silica which represents the glass phase in lithium-disilicate-based glass-ceramic materials formed of the hexafluorosilicates [
23]. Following HF etching, these silicates were removed under running water and resulted in small porosities creating an irregular roughness on the surface [
13,
24]. SEM images of etched surfaces (
Figure 1) of Celtra Duo and n!ce appear like a honeycomb surface. However, e.max CAD and Vita Suprinity were different and showed needlelike shapes. This could be related to the amount of glass phase, crystal size, and shape exposed on the surface of each material. Hydrofluoric acid in this study increased the roughness of all four types of LSGC. These results are in agreement with Kara et al. and Ramakrishnaiah et al. who reported that hydrofluoric acid increases the roughness and changes the surface structure as well as the wettability [
17,
25]. In addition, hydrofluoric acid produced less roughness compared to other surface treatments. Even though both Celtra Duo and Vita Suprinity are zirconia reinforced with lithium silicate glass-ceramic, hydrofluoric acid produced higher roughness on Celtra Duo than Vita Suprinity (
Table 2). This could be attributed to its glass phase content. According to other authors, surface treatment with hydrofluoric acid provides the best bond strength between resin cement and LSGC [
18,
26,
27]. However, another study reported that HF is not the best surface treatment choice to provide reliable bond strength [
28].
In this study, sand-blasting produced higher surface roughness compared to other surface treatments for Vita Suprinity and Celtra Duo. These observations are in agreement with some previous studies [
17,
29]. Most of the studies for e.max CAD report that sand-blasting is an insufficient method to improve the bond strength with resin cement [
18,
28]. However, Al-Thagafi et al. reported that zirconia-reinforced lithium silicate ceramic (Vita Suprinity) and lithium disilicate glass-ceramic (IPS e-max CAD) had higher repair bond strength value when treated by sand-blasting with Co Jet sand than treated with hydrofluoric acid [
30]. In addition, another study on the effect of different surface treatments on bond strength of lithium disilicate glass-ceramic (IPS e.max Press) in vitro found that sand-blasting with Co-Jet-silica-coated Al
2O
3 powder provided the best shear bond strength compared to HF and SB with aluminum oxide [
28]. In this study sand-blasting with aluminum oxide did not change the micromorphology of the surface, but it created small cracks around the crystal phase which could cause propagation and restoration failure in the future.
This study showed that the roughness from the surface treatment is fully dependent on the material composition. A recent study using X-ray photoelectron spectroscopy has shown an increase in the concentration of lithium after HF etching, and also a decrease of reinforced particles as ZrO
2 (for Celtra Duo and Vita Suprinity) and alumina (for n!ce) [
3]. These findings indicate that not only the glassy phase but also the fillers were removed by the acid etching. The detachment of larger fillers can generate more roughness when the surrounded glassy matrix is dissolved. Furthermore, the shape of the crystal can play an important role in the roughness. LSGC like e.max CAD and n!ce display the same needlelike crystal pattern [
3] which could explain the similar results on roughness analyses. Zirconia-reinforced LSGC showed a high roughness under sand-blasting treatment; however, several studies have demonstrated that it produced a weak bond strength [
18,
29,
31,
32,
33]. Among the possible reasons for that is the fact that the high elastic modulus and consequently low resilience of the ZnO
2 fillers could generate microcracks decreasing the mechanical properties of the LSGC [
32,
33,
34,
35].
The combination of SB and HF showed that the surface roughness created first by sand-blasting could be decreased to more than a half with subsequent treatment with hydrofluoric acid for Vita Suprinity and Celtra Duo. In contrast, the surface roughness was minimally increased for e.max CAD and n!ce. A sand-blasting + hydrofluoric surface treatment method could be an option to control the roughness value on ceramic and avoid the hazard of increasing the HF concentration or application time to provide reliable bond strengths. This study has the limitation of not assessing the bond strength of the experimental conditions. However, the literature has already demonstrated the lack of correlation between the surface roughness and good adhesion results [
10,
34,
36]. There are several areas at the material-science level to be explored before achieving the optimal adhesive joint (ceramic/resin-cement system/tooth structure), which will improve the clinical behavior of LSGC restorations.
5. Conclusions
Within the limitations of this in vitro study, the following conclusions are drawn.
Roughness is material-dependent. All surface treatments produced higher surface roughness compared to the untreated surface of all ceramic products in this study. Sand-blasting produced a higher surface roughness for Vita Suprinity and Celtra Duo. However, there is no significant difference between sand-blasting and sand-blasting + etching treatments for surface roughness for e.max CAD and n!ce. Hydrofluoric acid produced less surface roughness compared to other surface treatments.
Author Contributions
Conceptualization, R.F. and M.B.; methodology, R.F. and M.B.; formal analysis, M.B.; investigation, M.B., A.H. and R.F.; writing—original draft preparation, M.B., A.H. and R.F.; supervision, M.B., A.H. and R.F.; funding, A.H. and R.F.; acquisition, M.B., A.H. and R.F. All authors have read and agreed to the published version of the manuscript.
Funding
We thank the Tripoli University, Libya for the scholarship and the College of Dentistry Research Grant for supporting this study.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- França, R. Lithium Disilicate-Based Glass-Ceramics; Sacher, E., França, R., Eds.; Dental Biomaterials, World Scientific: Singapore, 2018; pp. 173–209. [Google Scholar]
- El-Meliegy, E.; Noort, R. Glasses and Glass Ceramics for Medical Applications; Springer: New York, NY, USA, 2012. [Google Scholar]
- França, R.; Bebsh, M.; Haimeur, A.; Fernandes, A.C.; Sacher, E. Physicochemical surface characterizations of four dental CAD/CAM lithium disilicate-based glass-ceramics on HF etching: An XPS study. Ceram. Int. 2021, 46, 1411–1418. [Google Scholar] [CrossRef]
- Serbena, F.C.; Mathias, I.; Foerster, C.E.; Zanotto, E.D. Crystallization toughening of a model glass-ceramic. Acta Mater. 2015, 86, 216–228. [Google Scholar] [CrossRef]
- Fasbinder, D.J.; Dennison, J.B.; Heys, D.; Neiva, G. A clinical evaluation of chairside lithium disilicate CAD/CAM crowns A two-year report. J. Am. Dent. Assoc. 2010, 141, 10s–14s. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, T.; Hotta, Y. CAD/CAM systems available for the fabrication of crown and bridge restorations. Aust. Dent. J. 2011, 56, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Kalavacharla, V.K.; Lawson, N.C.; Ramp, L.C.; Burgess, J.O. Influence of Etching Protocol and Silane Treatment with a Universal Adhesive on Lithium Disilicate Bond Strength. Oper. Dent. 2015, 40, 372–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Arcangelo, C.; Vanini, L.; Rondoni, G.D.; De Angelis, F. Wear properties of dental ceramics and porcelains compared with human enamel. J. Prosthet. Dent. 2016, 115, 350–355. [Google Scholar] [CrossRef] [PubMed]
- Della Bona, A.; Shen, C.Y.; Anusavice, K.J. Work of adhesion of resin on treated lithia disilicate-based ceramic. Dent. Mater. 2004, 20, 338–344. [Google Scholar] [CrossRef]
- Özcan, M.; Vallittu, P.K. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent. Mater. 2003, 19, 725–731. [Google Scholar] [CrossRef] [Green Version]
- Borges, G.A.; Sophr, A.M.; de Goes, M.F.; Sobrinho, L.C.; Chan, D.C.N. Effect of etching and airborne particle abrasion on the microstructure of different dental ceramics. J. Prosthet. Dent. 2003, 89, 479–488. [Google Scholar] [CrossRef]
- Lacy, A.M.; LaLuz, J.; Watanabe, L.G.; Dellinges, M. Effect of porcelain surface treatment on the bond to composite. J. Prosthet. Dent. 1988, 60, 288–291. [Google Scholar] [CrossRef]
- Lung, C.Y.; Matinlinna, J.P. Aspects of silane coupling agents and surface conditioning in dentistry: An overview. Dent. Mater. 2012, 28, 467–477. [Google Scholar] [CrossRef]
- Chen, J.H.; Matsumura, H.; Atsuta, M. Effect of different etching periods on the bond strength of a composite resin to a machinable porcelain. J. Dent. 1998, 26, 53–58. [Google Scholar] [CrossRef]
- Della Bona, A.; Van Noort, R. Ceramic surface preparations for resin bonding. Am. J. Dent. 1998, 11, 276–280. [Google Scholar]
- Dilber, E.; Yavuz, T.; Kara, H.B.; Ozturk, A.N. Comparison of the Effects of Surface Treatments on Roughness of Two Ceramic Systems. Photomed. Laser Surg. 2012, 30, 308–314. [Google Scholar] [CrossRef]
- Kara, H.B.; Kara, O.; Sayin, G.; Cakan, U.; Ozturk, A.N. Atomic force microscopy investigation of lithium disilicate glass ceramic after various surface treatments. Adv. Appl. Ceram. 2014, 113, 301–306. [Google Scholar] [CrossRef]
- Frankenberger, R.; Hartmann, E.; Krech, M.; Kramer, N.; Reich, S.; Braun, A.; Oggendorf, M. Adhesive luting of new CAD/CAM materials. Int. J. Comput. Dent. 2015, 18, 9–20. [Google Scholar]
- Gre, C.P.; de Re Silveira, R.C.; Shibata, S.; Lago, C.T.; Vieira, L.C. Effect of Silanization on Microtensile Bond Strength of Different Resin Cements to a Lithium Disilicate Glass Ceramic. J. Contemp. Dent. Pract. 2016, 17, 149–153. [Google Scholar] [CrossRef] [Green Version]
- Nagai, T.; Kawamoto, Y.; Kakehashi, Y.; Matsumura, H. Adhesive bonding of a lithium disilicate ceramic material with resin-based luting agents. J. Oral Rehabil. 2005, 32, 598–605. [Google Scholar] [CrossRef]
- Maruo, Y.; Nishigawa, G.; Yoshihara, K.; Minagi, S.; Matsumoto, T.; Irie, M. Does 8-methacryloxyoctyl trimethoxy silane (8-MOTS) improve initial bond strength on lithium disilicate glass ceramic? Dent. Mater. 2017, 33, e95–e100. [Google Scholar] [CrossRef] [PubMed]
- Lambade, D.P.; Gundawar, S.M.; Radke, U.M. Evaluation of adhesive bonding of lithium disilicate ceramic material with duel cured resin luting agents. J. Clin. Diagn. Res. 2015, 9, ZC01-5. [Google Scholar] [CrossRef] [PubMed]
- Matinlinna, J.; Vallittu, P. Bonding of resin composites to etchable ceramic surfaces–an insight review of the chemical aspects on surface conditioning. J. Oral Rehabil. 2007, 34, 622–630. [Google Scholar] [CrossRef] [PubMed]
- Thurmond, J.W.; Barkmeier, W.W.; Wilwerding, T.M. Effect of Porcelain Surface Treatments on Bond Strengths of Composite Resin-Bonded to Porcelain. J. Prosthet. Dent. 1994, 72, 355–359. [Google Scholar] [CrossRef]
- Ramakrishnaiah, R.; Alkheraif, A.A.; Divakar, D.D.; Matinlinna, J.P.; Vallittu, P.K. The Effect of Hydrofluoric Acid Etching Duration on the Surface Micromorphology, Roughness, and Wettability of Dental Ceramics. Int. J. Mol. Sci. 2016, 17, E822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mokhtarpour, F.; Alaghehmand, H.; Khafri, S. Effect of hydrofluoric acid surface treatments on micro-shear bond strength of CAD/CAM ceramics. Electron. Physician 2017, 9, 5487. [Google Scholar] [CrossRef] [Green Version]
- Maruo, Y.; Nishigawa, G.; Irie, M.; Yoshihara, K.; Matsumoto, T.; Minagi, S. Does acid etching morphologically and chemically affect lithium disilicate glass ceramic surfaces? J. Appl. Biomater. Fundam. Mater. 2017, 15, e93–e100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Özdemir, H.; Aladag, L.I. Effect of different surface treatments on bond strength of different resin cements to lithium disilicate glass ceramic: An in vitro study. Biotechnol. Biotechnol. Equip. 2017, 31, 815–820. [Google Scholar] [CrossRef] [Green Version]
- Blatz, M.B.; Sadan, A.; Kern, M. Resin-ceramic bonding: A review of the literature. J. Prosthet. Dent. 2003, 89, 268–274. [Google Scholar] [CrossRef] [Green Version]
- Al-Thagafi, R.; Al-Zordk, W.; Saker, S. Influence of Surface Conditioning Protocols on Reparability of CAD/CAM Zirconia-reinforced Lithium Silicate Ceramic. J. Adhes. Dent. 2016, 18, 135–141. [Google Scholar]
- Spitznagel, F.A.; Horvath, S.D.; Guess, P.C.; Blatz, M.B. Resin bond to indirect composite and new ceramic/polymer materials: A review of the literature. J. Esthet. Restor. Dent. 2014, 26, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Moravej-Salehi, E.; Moravej-Salehi, E.; Valian, A. Surface topography and bond strengths of feldspathic porcelain prepared using various sandblasting pressures. J. Investig. Clin. Dent. 2016, 7, 347–354. [Google Scholar] [CrossRef]
- Strasser, T.; Preis, V.; Behr, M.; Rosentritt, M. Roughness, surface energy, and superficial damages of CAD/CAM materials after surface treatment. Clin. Oral Investig. 2018, 22, 2787–2797. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, V.L.B.; de Castro, E.F.; Bonvent, J.J.; de Andrade, O.S.; Nascimento, F.D.; Giannini, M.; Cavalli, V. Surface treatments on CAD/CAM glass-ceramics: Influence on roughness, topography, and bond strength. J. Esthet. Restor. Dent. 2021, 33, 739–749. [Google Scholar] [CrossRef]
- Ozcan, M.; Allahbeickaraghi, A.; Dundar, M. Possible hazardous effects of hydrofluoric acid and recommendations for treatment approach: A review. Clin. Oral Investig. 2012, 16, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Fabian Fonzar, R.; Goracci, C.; Carrabba, M.; Louca, C.; Ferrari, M.; Vichi, A. Influence of Acid Concentration and Etching Time on Composite Cement Adhesion to Lithium-silicate Glass Ceramics. J. Adhes. Dent. 2020, 22, 175–182. [Google Scholar] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).