SIU-ICUD: Germline Genetic Susceptibility to Prostate Cancer: Utility and Clinical Implementation
Abstract
1. Introduction
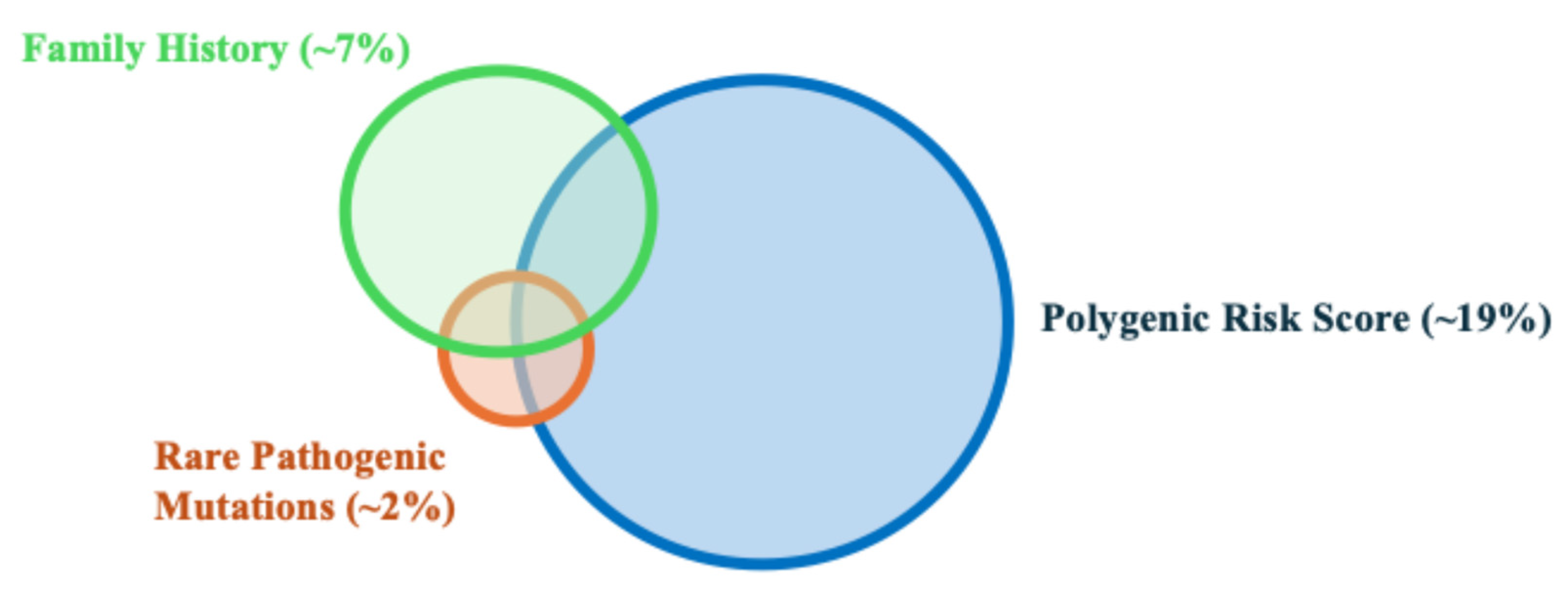
1.1. Genetic Assessment: Three Required Components
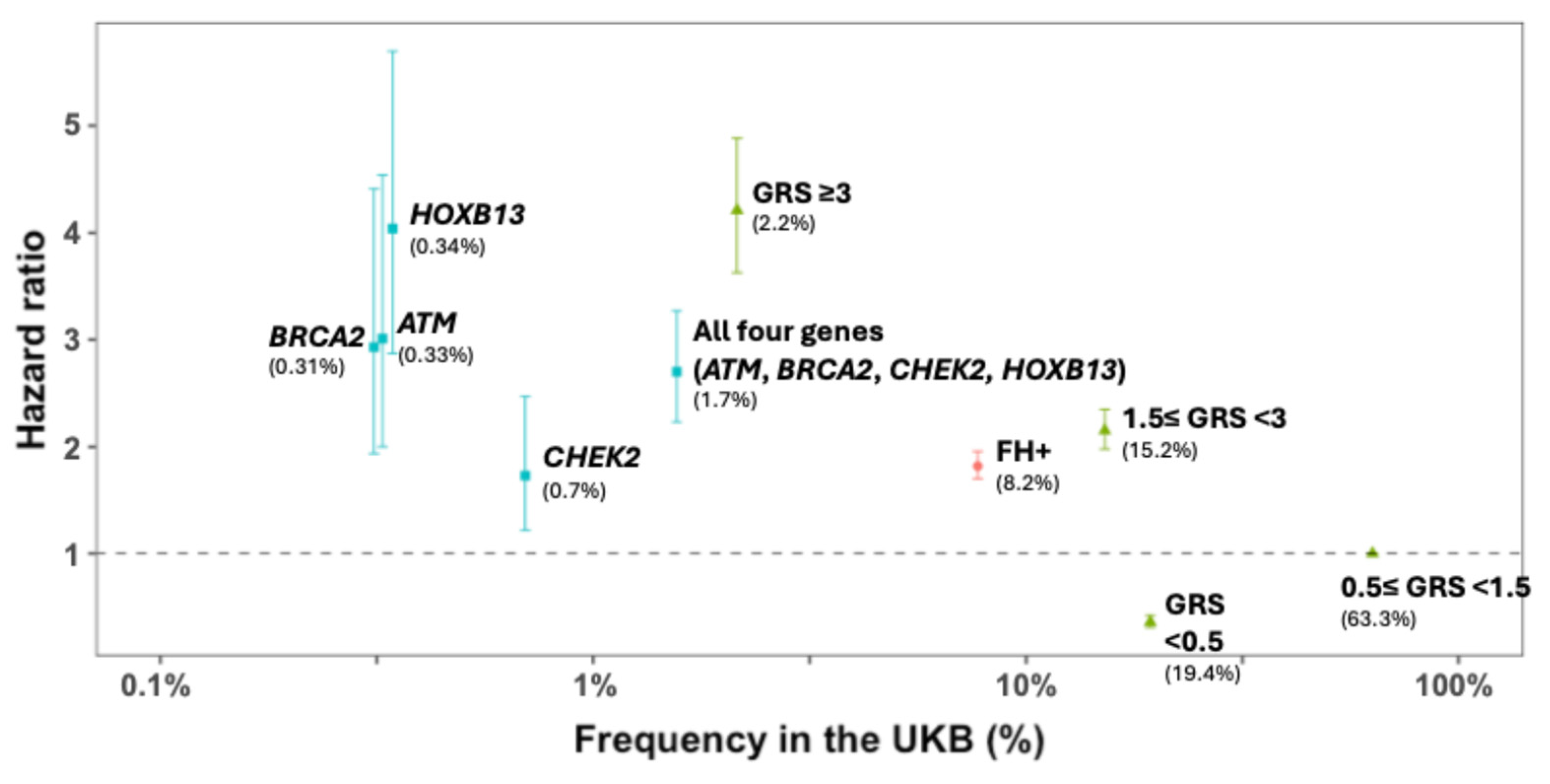
1.2. Rare Pathogenic Mutations and Prostate Cancer Susceptibility
1.3. Single Nucleotide Polymorphisms, Polygenic Risk Scores, and Prostate Cancer Susceptibility
1.4. Key Characteristics of PRS for Prostate Cancer Risk Assessment
1.5. Inability to Differentiate Risk Between Indolent and Aggressive Prostate Cancer
1.6. Challenges and Opportunities for PRS Adoption in the Clinic
1.7. Genetic Variation Among Different Racial Groups
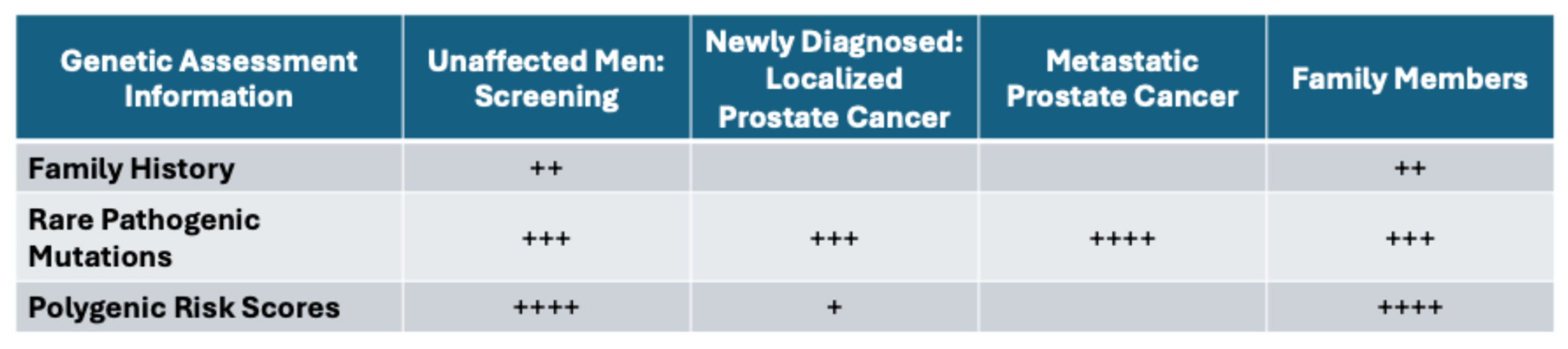
1.8. Clinical Implementation of Genetic Assessment: Utility for Unaffected Individuals
1.9. Clinical Implementation of Genetic Assessment: Utility for Patients on Active Surveillance
1.10. Clinical Implementation of Genetic Assessment: Responsiveness to Treatment for Metastatic Cancer
1.11. Targeted Prostate Cancer Screening in Individuals with Alterations in Rare Variants
1.12. Targeted Prostate Cancer Screening in Individuals with Alterations in Common Variants
1.13. Future of Genetic Information in Clinical Practice
1.14. Implementation Strategies for Genetic Counseling and Germline Testing
1.15. Incorporating Germline Genetics into Healthcare Systems
1.16. Satisfaction with Genetic Testing
2. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Siegel, R.L.; Giaquinto, A.N.; Jemal, A. Cancer statistics, 2024. CA Cancer J. Clin. 2024, 74, 12–49. [Google Scholar] [CrossRef] [PubMed]
- Carter, B.S.; Bova, G.S.; Beaty, T.H.; Steinberg, G.D.; Childs, B.; Isaacs, W.B.; Walsh, P.C. Hereditary prostate cancer: Epidemiologic and clinical features. J. Urol. 1993, 150, 797–802. [Google Scholar] [CrossRef] [PubMed]
- Hampel, H.; Bennett, R.L.; Buchanan, A.; Pearlman, R.; Wiesner, G.L. Guideline Development Group, American College of Medical Genetics and Genomics Professional Practice and Guidelines Committee and National Society of Genetic Counselors Practice Guidelines Committee. A practice guideline from the American College of Medical Genetics and Genomics and the National Society of Genetic Counselors: Referral indications for cancer predisposition assessment. Genet. Med. 2015, 17, 70–87. [Google Scholar] [PubMed]
- Giri, V.N.; Hegarty, S.E.; Hyatt, C.; O’Leary, E.; Garcia, J.; Knudsen, K.E.; Kelly, W.K.; Gomella, L.G. Germline genetic testing for inherited prostate cancer in practice: Implications for genetic testing, precision therapy, and cascade testing. Prostate 2018, 79, 333–339. [Google Scholar] [CrossRef]
- De Bono, J.; Mateo, J.; Fizazi, K.; Saad, F.; Shore, N.; Sandhu, S.; Chi, K.N.; Sartor, O.; Agarwal, N.; Olmos, D.; et al. Olaparib for Metastatic Castration-Resistant Prostate Cancer. N. Engl. J. Med. 2020, 382, 2091–2102. [Google Scholar] [CrossRef]
- Abida, W.; Patnaik, A.; Campbell, D.; Shapiro, J.; Bryce, A.H.; McDermott, R.; Sautois, B.; Vogelzang, N.J.; Bambury, R.M.; Voog, E.; et al. Rucaparib in Men With Metastatic Castration-Resistant Prostate Cancer Harboring a BRCA1 or BRCA2 Gene Alteration. J. Clin. Oncol. 2020, 38, 3763–3772. [Google Scholar] [CrossRef]
- Agarwal, N.; A Azad, A.; Carles, J.; Fay, A.P.; Matsubara, N.; Heinrich, D.; Szczylik, C.; De Giorgi, U.; Joung, J.Y.; Fong, P.C.C.; et al. Talazoparib plus enzalutamide in men with first-line metastatic castration-resistant prostate cancer (TALAPRO-2): A randomised, placebo-controlled, phase 3 trial. Lancet 2023, 402, 291–303. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network Clinical Pracice Guidelines in Oncology (NCCN Guidelines®): Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic (Version 3.2024). Available online: https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1545 (accessed on 3 March 2024).
- National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology. Prostate Cancer Early Detection Version 1. 2024. Available online: https://www.nccn.org/professionals/physician_gls/pdf/prostate_detection.pdf (accessed on 3 March 2024).
- National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology. Prostate Cancer Version 1. 2024. Available online: https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf (accessed on 3 March 2024).
- Schaeffer, E.M.; Srinivas, S.; Adra, N.; An, Y.; Barocas, D.; Bitting, R.; Bryce, A.; Chapin, B.; Cheng, H.H.; D’Amico, A.V.; et al. Prostate Cancer, Version 4.2023, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2023, 21, 1067–1096. [Google Scholar] [CrossRef]
- Zheng, S.L.; Sun, J.; Wiklund, F.; Smith, S.; Stattin, P.; Li, G.; Adami, H.-O.; Hsu, F.-C.; Zhu, Y.; Bälter, K.; et al. Cumulative association of five genetic variants with prostate cancer. N. Engl. J. Med. 2008, 358, 910–919. [Google Scholar] [CrossRef]
- Xu, J.; Resurreccion, W.K.; Shi, Z.; Wei, J.; Wang, C.-H.; Zheng, S.L.; Hulick, P.J.; Ross, A.E.; Pavlovich, C.P.; Helfand, B.T.; et al. Inherited risk assessment and its clinical utility for predicting prostate cancer from diagnostic prostate biopsies. Prostate Cancer Prostatic. Dis. 2022, 25, 422–430. [Google Scholar] [CrossRef]
- Shi, Z.; Platz, E.A.; Wei, J.; Na, R.; Fantus, R.J.; Wang, C.-H.; Eggener, S.E.; Hulick, P.J.; Duggan, D.; Zheng, S.L.; et al. Performance of Three Inherited Risk Measures for Predicting Prostate Cancer Incidence and Mortality: A Population-based Prospective Analysis. Eur. Urol. 2021, 79, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Na, R.; Labbate, C.; Yu, H.; Shi, Z.; Fantus, R.J.; Wang, C.-H.; Andriole, G.L.; Isaacs, W.B.; Zheng, S.L.; Helfand, B.T.; et al. Single-Nucleotide Polymorphism–Based Genetic Risk Score and Patient Age at Prostate Cancer Diagnosis. JAMA Netw. Open 2019, 2, e1918145. [Google Scholar] [CrossRef] [PubMed]
- Conti, D.V.; Darst, B.F.; Moss, L.C.; Saunders, E.J.; Sheng, X.; Chou, A.; Schumacher, F.R.; Al Olama, A.A.; Benlloch, S.; Dadaev, T.; et al. Trans-ancestry genome-wide association meta-analysis of prostate cancer identifies new susceptibility loci and informs genetic risk prediction. Nat. Genet. 2021, 53, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Na, R.; Packiam, V.T.; Conran, C.A.; Jiang, D.; Tao, S.; Yu, H.; Lin, X.; Meng, W.; Zheng, S.L.; et al. Reclassification of prostate cancer risk using sequentially identified SNPs: Results from the REDUCE trial. Prostate 2017, 77, 1179–1186. [Google Scholar] [CrossRef]
- Plym, A.; Zhang, Y.; Stopsack, K.H.; Jee, Y.H.; Wiklund, F.; Kibel, A.S.; Kraft, P.; Giovannucci, E.; Penney, K.L.; Mucci, L.A. Family History of Prostate and Breast Cancer Integrated with a Polygenic Risk Score Identifies Men at Highest Risk of Dying from Prostate Cancer before Age 75 Years. Clin. Cancer Res. 2022, 28, 4926–4933. [Google Scholar] [CrossRef]
- Huynh-Le, M.-P.; Fan, C.C.; Karunamuni, R.; Thompson, W.K.; Martinez, M.E.; Eeles, R.A.; Kote-Jarai, Z.; Muir, K.; Schleutker, J.; Pashayan, N.; et al. Polygenic hazard score is associated with prostate cancer in multi-ethnic populations. Nat. Commun. 2021, 12, 1236. [Google Scholar] [CrossRef]
- Pagadala, M.S.; Lynch, J.; Karunamuni, R.; Alba, P.R.; Lee, K.M.; Agiri, F.Y.; Anglin, T.; Carter, H.; Gaziano, J.M.; Jasuja, G.K.; et al. Polygenic risk of any, metastatic, and fatal prostate cancer in the Million Veteran Program. J. Natl. Cancer Inst. 2023, 115, 190–199. [Google Scholar] [CrossRef]
- Darst, B.F.; Sheng, X.; Eeles, R.A.; Kote-Jarai, Z.; Conti, D.V.; Haiman, C.A. Combined Effect of a Polygenic Risk Score and Rare Genetic Variants on Prostate Cancer Risk. Eur. Urol. 2021, 80, 134–138. [Google Scholar] [CrossRef]
- Teo, Y.Y.; Small, K.S.; Kwiatkowski, D.P. Methodological challenges of genome-wide association analysis in Africa. Nat. Rev. Genet. 2010, 11, 149–160. [Google Scholar] [CrossRef]
- Lachance, J.; Berens, A.J.; Hansen, M.E.B.; Teng, A.K.; Tishkoff, S.A.; Rebbeck, T.R. Genetic Hitchhiking and Population Bottlenecks Contribute to Prostate Cancer Disparities in Men of African Descent. Cancer Res. 2018, 78, 2432–2443. [Google Scholar] [CrossRef]
- Kim, M.S.; Patel, K.P.; Teng, A.K.; Berens, A.J.; Lachance, J. Genetic disease risks can be misestimated across global populations. Genome. Biol. 2018, 19, 179. [Google Scholar] [CrossRef] [PubMed]
- Manrai, A.K.; Funke, B.H.; Rehm, H.L.; Olesen, M.S.; Maron, B.A.; Szolovits, P.; Margulies, D.M.; Loscalzo, J.; Kohane, I.S. Genetic Misdiagnoses and the Potential for Health Disparities. N. Engl. J. Med. 2016, 375, 655–665. [Google Scholar] [CrossRef]
- Xu, J.; Isaacs, W.B.; Mamawala, M.; Shi, Z.; Landis, P.; Petkewicz, J.; Wei, J.; Wang, C.; Resurreccion, W.K.; Na, R.; et al. Association of prostate cancer polygenic risk score with number and laterality of tumor cores in active surveillance patients. Prostate 2021, 81, 703–709. [Google Scholar] [CrossRef]
- Kearns, J.T.; Helfand, B.T.; Xu, J. Moving Prostate Cancer Polygenic Risk Scores from Research Towards Clinical Practice. Eur. Urol. Focus 2022, 8, 913–915. [Google Scholar] [CrossRef]
- Shi, Z.; Lu, L.; Resurreccion, W.K.; Yang, W.; Wei, J.; Wang, Q.; Engelmann, V.; Zheng, S.L.; Cooney, K.A.; Isaacs, W.B.; et al. Association of germline rare pathogenic mutations in guideline-recommended genes with prostate cancer progression: A meta-analysis. Prostate 2022, 82, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Saunders, E.J.; Dadaev, T.; Brook, M.N.; Wakerell, S.; Govindasami, K.; Rageevakumar, R.; Hussain, N.; Osborne, A.; Keating, D.; Lophatananon, A.; et al. Identification of Genes with Rare Loss of Function Variants Associated with Aggressive Prostate Cancer and Survival. Eur. Urol. Oncol. 2024, 7, 248–257. [Google Scholar] [CrossRef] [PubMed]
- Abida, W.; Cheng, M.L.; Armenia, J.; Middha, S.; Autio, K.A.; Vargas, H.A.; Rathkopf, D.; Morris, M.J.; Danila, D.C.; Slovin, S.F.; et al. Analysis of the Prevalence of Microsatellite Instability in Prostate Cancer and Response to Immune Checkpoint Blockade. JAMA Oncol. 2019, 5, 471–478. [Google Scholar] [CrossRef]
- Kuzbari, Z.; Bandlamudi, C.; Loveday, C.; Garrett, A.; Mehine, M.; George, A.; Hanson, H.; Snape, K.; Kulkarni, A.; Allen, S.; et al. Germline-focused analysis of tumour-detected variants in 49,264 cancer patients: ESMO Precision Medicine Working Group recommendations. Ann. Oncol. 2023, 34, 215–227. [Google Scholar] [CrossRef]
- Ritch, E.; Fu, S.Y.; Herberts, C.; Wang, G.; Warner, E.W.; Schönlau, E.; Taavitsainen, S.; Murtha, A.J.; Vandekerkhove, G.; Beja, K.; et al. Identification of Hypermutation and Defective Mismatch Repair in ctDNA from Metastatic Prostate Cancer. Clin. Cancer Res. 2020, 26, 1114–1125. [Google Scholar] [CrossRef]
- Antonarakis, E.S.; Shaukat, F.; Velho, P.I.; Kaur, H.; Shenderov, E.; Pardoll, D.M.; Lotan, T.L. Clinical Features and Therapeutic Outcomes in Men with Advanced Prostate Cancer and DNA Mismatch Repair Gene Mutations. Eur. Urol. 2019, 75, 378–382. [Google Scholar] [CrossRef]
- Bancroft, E.K.; Page, E.C.; Brook, M.N.; Thomas, S.; Taylor, N.; Pope, J.; McHugh, J.; Jones, A.-B.; Karlsson, Q.; Merson, S.; et al. A prospective prostate cancer screening programme for men with pathogenic variants in mismatch repair genes (IMPACT): Initial results from an international prospective study. Lancet. Oncol. 2021, 22, 1618–1631. [Google Scholar] [CrossRef] [PubMed]
- van der Doelen, M.J.; Velho, P.I.; Slootbeek, P.H.; Naga, S.P.; Bormann, M.; van Helvert, S.; Kroeze, L.I.; van Oort, I.M.; Gerritsen, W.R.; Antonarakis, E.S.; et al. Impact of DNA damage repair defects on response to radium-223 and overall survival in metastatic castration-resistant prostate cancer. Eur. J. Cancer 2020, 136, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, D.N.; Rescigno, P.; Liu, D.; Yuan, W.; Carreira, S.; Lambros, M.B.; Seed, G.; Mateo, J.; Riisnaes, R.; Mullane, S.; et al. Immunogenomic analyses associate immunological alterations with mismatch repair defects in prostate cancer. J. Clin. Investig. 2018, 128, 5185. [Google Scholar] [CrossRef]
- Pritchard, C.C.; Mateo, J.; Walsh, M.F.; De Sarkar, N.; Abida, W.; Beltran, H.; Garofalo, A.; Gulati, R.; Carreira, S.; Eeles, R.; et al. Inherited DNA-Repair Gene Mutations in Men with Metastatic Prostate Cancer. N. Engl. J. Med. 2016, 375, 443–453. [Google Scholar] [CrossRef]
- Carter, H.B.; Helfand, B.; Mamawala, M.; Wu, Y.; Landis, P.; Yu, H.; Wiley, K.; Na, R.; Shi, Z.; Petkewicz, J.; et al. Germline Mutations in ATM and BRCA1/2 Are Associated with Grade Reclassification in Men on Active Surveillance for Prostate Cancer. Eur. Urol. 2019, 75, 743–749. [Google Scholar] [CrossRef]
- Bancroft, E.K.; Page, E.C.; Castro, E.; Lilja, H.; Vickers, A.; Sjoberg, D.; Assel, M.; Foster, C.S.; Mitchell, G.; Drew, K.; et al. Targeted prostate cancer screening in BRCA1 and BRCA2 mutation carriers: Results from the initial screening round of the IMPACT study. Eur. Urol. 2014, 66, 489–499. [Google Scholar] [CrossRef]
- Page, E.C.; Bancroft, E.K.; Brook, M.N.; Assel, M.; Hassan Al Battat, M.; Thomas, S.; Taylor, N.; Chamberlain, A.; Pope, J.; Ni Raghallaigh, H.; et al. Interim Results from the IMPACT Study: Evidence for Prostate-specific Antigen Screening in BRCA2 Mutation Carriers. Eur. Urol. 2019, 76, 831–842. [Google Scholar] [CrossRef] [PubMed]
- Helfand, B.T.; Catalona, W.J.; Xu, J. A genetic-based approach to personalized prostate cancer screening and treatment. Curr. Opin. Urol. 2015, 25, 53–58. [Google Scholar] [CrossRef]
- Eeles, R.A.; Bancroft, E.K.; McHugh, J.K.; Saunders, E.; Brook, M.; McGrowder, E.; Wakerell, S.; James, D.; Page, E.; Osborne, A.; et al. Effect of polygenic risk score for clinically significant prostate cancer in a screening program: The BARCODE 1 study results. JCO 2024, 42 (Suppl. S16), 10500. [Google Scholar] [CrossRef]
- Morrow, A.; Chan, P.; Tucker, K.M.; Taylor, N. The design, implementation, and effectiveness of intervention strategies aimed at improving genetic referral practices: A systematic review of the literature. Genet. Med. 2021, 23, 2239–2249. [Google Scholar] [CrossRef]
- Loeb, S.; Byrne, N.; Walter, D.; Makarov, D.V.; Wise, D.R.; Becker, D.; Giri, V.N. Knowledge and practice regarding prostate cancer germline testing among urologists: Gaps to address for optimal implementation✰,✰✰. Cancer Treat. Res. Commun. 2020, 25, 100212. [Google Scholar] [CrossRef] [PubMed]
- Giri, V.N.; Walker, A.; Gross, L.; Trabulsi, E.J.; Lallas, C.D.; Kelly, W.K.; Gomella, L.G.; Fischer, C.; Loeb, S. Helix: A Digital Tool to Address Provider Needs for Prostate Cancer Genetic Testing in Clinical Practice. Clin. Genitourin. Cancer 2022, 20, e104–e113. [Google Scholar] [CrossRef]
- Welcome to ClinGen. Available online: https://clinicalgenome.org/ (accessed on 22 March 2024).
- ** ClinVar **. Available online: http://www.clinvar.com/ (accessed on 22 March 2024).
- Lahiri, S.; Pirzadeh-Miller, S.; Moriarty, K.; Kubiliun, N. Implementation of a Population-Based Cancer Family History Screening Program for Lynch Syndrome. Cancer Control 2023, 30, 10732748231175011. [Google Scholar] [CrossRef]
- David, S.P.; Dunnenberger, H.M.; Choi, S.; DePersia, A.; Ilbawi, N.; Ward, C.; Wake, D.T.; Khandekar, J.D.; Shannon, Y.; Hughes, K.; et al. Personalized medicine in a community health system: The NorthShore experience. Front. Genet. 2023, 14, 1308738. [Google Scholar] [CrossRef] [PubMed]
- Pritchard, D.; Hulick, P.J.; Wells, C.J. The integration of personalized medicine into health systems: Progress and a path forward. Pers. Med. 2021, 18, 527–531. [Google Scholar] [CrossRef] [PubMed]
- Orlando, L.A.; Wu, R.R.; Myers, R.A.; Buchanan, A.H.; Henrich, V.C.; Hauser, E.R.; Ginsburg, G.S. Clinical utility of a Web-enabled risk-assessment and clinical decision support program. Genet. Med. 2016, 18, 1020–1028. [Google Scholar] [CrossRef]
- Webster, E.M.; Ahsan, M.D.; Perez, L.; Levi, S.R.; Thomas, C.; Christos, P.; Hickner, A.; Hamilton, J.G.; Babagbemi, K.; Cantillo, E.; et al. Chatbot Artificial Intelligence for Genetic Cancer Risk Assessment and Counseling: A Systematic Review and Meta-Analysis. JCO Clin. Cancer Inform. 2023, 7, e2300123. [Google Scholar] [CrossRef]
- Voils, C.I.; Coffman, C.J.; Wu, R.R.; Grubber, J.M.; Fisher, D.A.; Strawbridge, E.M.; Sperber, N.; Wang, V.; Scheuner, M.T.; Provenzale, D.; et al. A Cluster Randomized Trial of a Family Health History Platform to Identify and Manage Patients at Increased Risk for Colorectal Cancer. J. Gen. Intern. Med. 2023, 38, 1375–1383. [Google Scholar] [CrossRef]
- Wang, C.; Lu, H.; Bowen, D.J.; Xuan, Z. Implementing digital systems to facilitate genetic testing for hereditary cancer syndromes: An observational study of 4 clinical workflows. Genet. Med. 2023, 25, 100802. [Google Scholar] [CrossRef]
- Henderson, G.E.; Wolf, S.M.; Kuczynski, K.J.; Joffe, S.; Sharp, R.R.; Parsons, D.W.; Knoppers, B.M.; Yu, J.-H.; Appelbaum, P.S. The challenge of informed consent and return of results in translational genomics: Empirical analysis and recommendations. J. Law Med. Ethics 2014, 42, 344–355. [Google Scholar] [CrossRef]
- Russo, J.; Giri, V.N. Germline testing and genetic counselling in prostate cancer. Nat. Rev. Urol. 2022, 19, 331–343. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Société Internationale d’Urologie. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kearns, J.T.; Ashworth, A.; Castro, E.; Eeles, R.A.; FitzGerald, L.M.; Hulick, P.J.; Loeb, S.; Pavlovich, C.P.; Rebbeck, T.R.; Vadaparampil, S.T.; et al. SIU-ICUD: Germline Genetic Susceptibility to Prostate Cancer: Utility and Clinical Implementation. Soc. Int. Urol. J. 2025, 6, 45. https://doi.org/10.3390/siuj6030045
Kearns JT, Ashworth A, Castro E, Eeles RA, FitzGerald LM, Hulick PJ, Loeb S, Pavlovich CP, Rebbeck TR, Vadaparampil ST, et al. SIU-ICUD: Germline Genetic Susceptibility to Prostate Cancer: Utility and Clinical Implementation. Société Internationale d’Urologie Journal. 2025; 6(3):45. https://doi.org/10.3390/siuj6030045
Chicago/Turabian StyleKearns, James T., Annabelle Ashworth, Elena Castro, Rosalind A. Eeles, Liesel M. FitzGerald, Peter J. Hulick, Stacy Loeb, Christian P. Pavlovich, Timothy R. Rebbeck, Susan T. Vadaparampil, and et al. 2025. "SIU-ICUD: Germline Genetic Susceptibility to Prostate Cancer: Utility and Clinical Implementation" Société Internationale d’Urologie Journal 6, no. 3: 45. https://doi.org/10.3390/siuj6030045
APA StyleKearns, J. T., Ashworth, A., Castro, E., Eeles, R. A., FitzGerald, L. M., Hulick, P. J., Loeb, S., Pavlovich, C. P., Rebbeck, T. R., Vadaparampil, S. T., Shi, Z., Tran, H., Wei, J., Xu, J., & Helfand, B. T. (2025). SIU-ICUD: Germline Genetic Susceptibility to Prostate Cancer: Utility and Clinical Implementation. Société Internationale d’Urologie Journal, 6(3), 45. https://doi.org/10.3390/siuj6030045






