A female in her mid-40s presented to the emergency department with acute onset umbilical pain associated with vomiting. There was no flank pain, hematuria, dysuria, or fever. An ultrasound of the abdomen and pelvis was performed, which showed an empty right renal fossa and fused, conglomerated reniform-shaped structure in the midline at the umbilical region with vascularity noted on Doppler imaging. The patient was further advised on a cross-sectional study for better characterization. A contrast-enhanced computed tomography (CT) study of the abdomen with CT urography was performed, which showed empty right renal fossa and ectopic right kidney in the midline, which was fused with another kidney unit, which was further fused with the lower pole of the left kidney. In contrast sequences, the supernumerary kidney was receiving blood supply from the right common iliac artery and draining through the right common iliac vein, and both right and left kidneys had a normal vascular supply from the aorta and inferior vena cava (
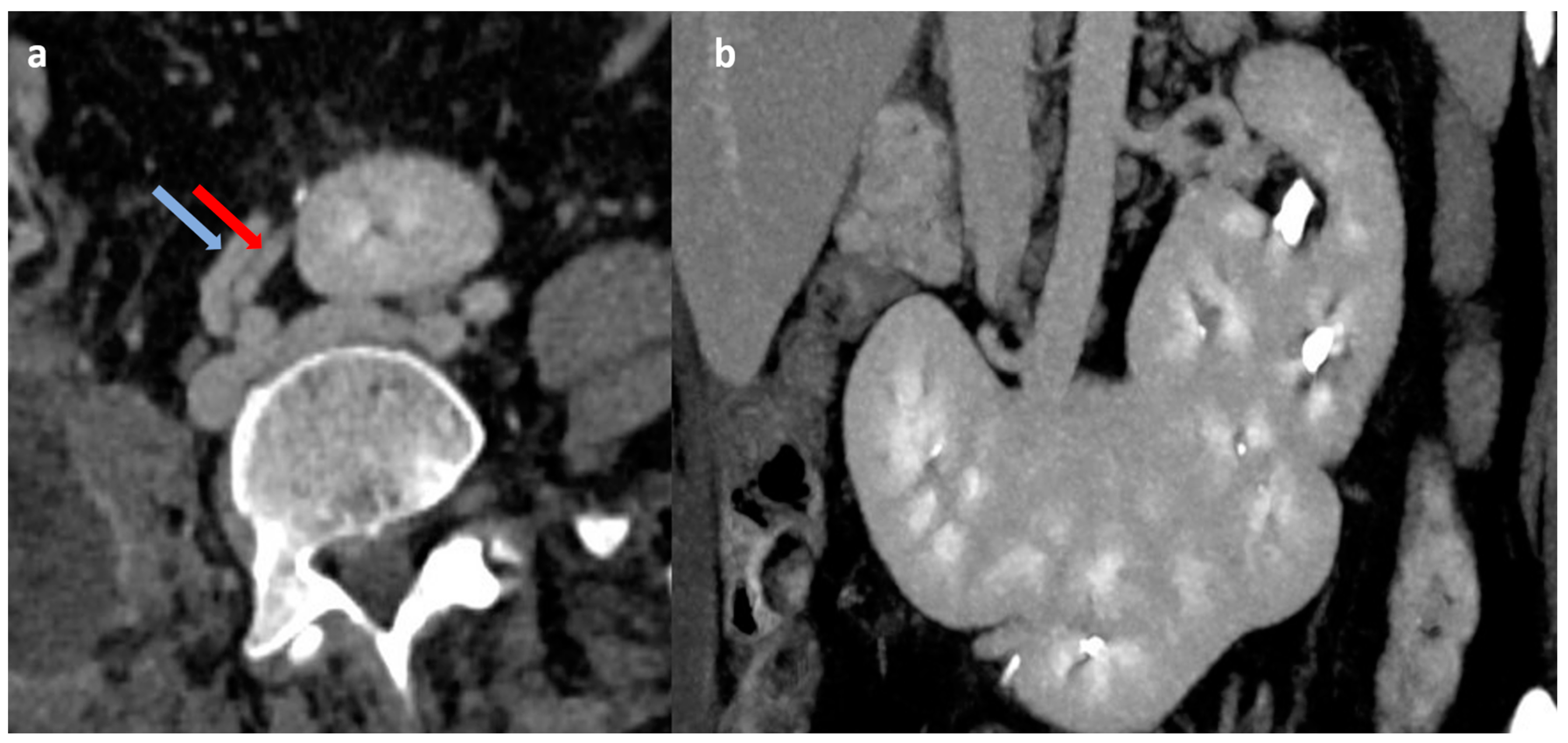
Figure 1). On delayed images, both the right ectopic kidney and left kidney showed a bifid pelvicalyceal system, and the supernumerary kidney showed a single pelvicalyceal system, with a total of five pelvicalyceal systems present in our patient (
Figure 2). The patient was managed conservatively and became asymptomatic after 2 days.
A supernumerary kidney is a rare congenital anomaly of renal number with more than two kidneys present in an individual with their own collecting system, vascular supply, and well-defined encapsulated parenchyma. The embryological origin is speculated to be an abnormally divided nephrogenic cord into two metanephric blastemas. It was first described 350 years ago, and the true incidence is not confirmed, with approximately 100 cases reported in the literature [
1]. It is usually smaller and caudal to the native kidney. It can either be attached to the native kidney or can be a separate moiety. The fusion of the supernumerary kidney with the ipsilateral native kidney is an extremely rare association [
2]. The fusion of all the renal moieties in the case of supernumerary kidneys is still rarer and has been reported sparsely in the literature [
3]. The supernumerary kidney is caudal to the ipsilateral kidney and is associated with the partial or complete duplex collecting system [
4,
5]. In our patient, all three kidneys were fused with the ectopic right kidney in the midline, which was fused with another kidney unit, which was further fused with the lower pole of the left kidney and took the shape of a partial horseshoe kidney with both the longitudinal axis kidneys having duplex collecting system and the transversely oriented kidney having its separate collecting system. The usual presentation of supernumerary kidneys is incidental, with diagnosis done on imaging for a different reason, as described in our case. However, it may present primarily with renal stones, infection, or tumor. The management of supernumerary kidneys depends on symptoms and underlying pathology. Usually, no treatment is required unless the patient is symptomatic. CT or MR angiography should be performed to delineate the vascular supply before any intervention.
Author Contributions
Conceptualization, N.K. and K.R.; methodology, N.K.; software, S.S.; validation, N.K., S.S. and K.R.; formal analysis, K.R.; investigation, N.K.; resources, S.S.; data curation, K.R.; writing—original draft preparation, N.K.; writing—review and editing, K.R.; visualization, S.S.; supervision, N.K.; project administration, N.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study did not require ethical approval.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this case.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Carlson, H.E. Supernumerary kidney as a cause of uretero-pelvic obstruction. J. Urol. 1946, 56, 179–182. [Google Scholar] [CrossRef] [PubMed]
- Manandhar, S.; Khanal, A. Fused right supernumerary kidney: A case report. JNMA J. Nepal. Med. Assoc. 2019, 57, 376–378. [Google Scholar] [CrossRef] [PubMed]
- Vakade, A.D.; Sudin, S.R.; Sasidharan, K.; Jayasudha, S. Supernumerary kidney forming isthmus of horseshoe kidney: A rare presentation. Indian J. Urol. 2020, 36, 138–139. [Google Scholar] [CrossRef] [PubMed]
- Sthephens, F.D.; Smith, E.D.; Hutson, J.M. Normal embriology of the upper urinary tract and kidneys. In Congenital Anomalies of the Kidney, Urinary and Genital Tracts; Martin Dunitz: London, UK, 2002; p. 28392. [Google Scholar]
- Koureas, A.P.; Panourgias, E.C.; Gouliamos, A.D.; Trakadas, S.J.; Vlahos, L.J. Imaging of a supernumerary kidney. Eur. Radiol. 2000, 10, 1722–1723. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).