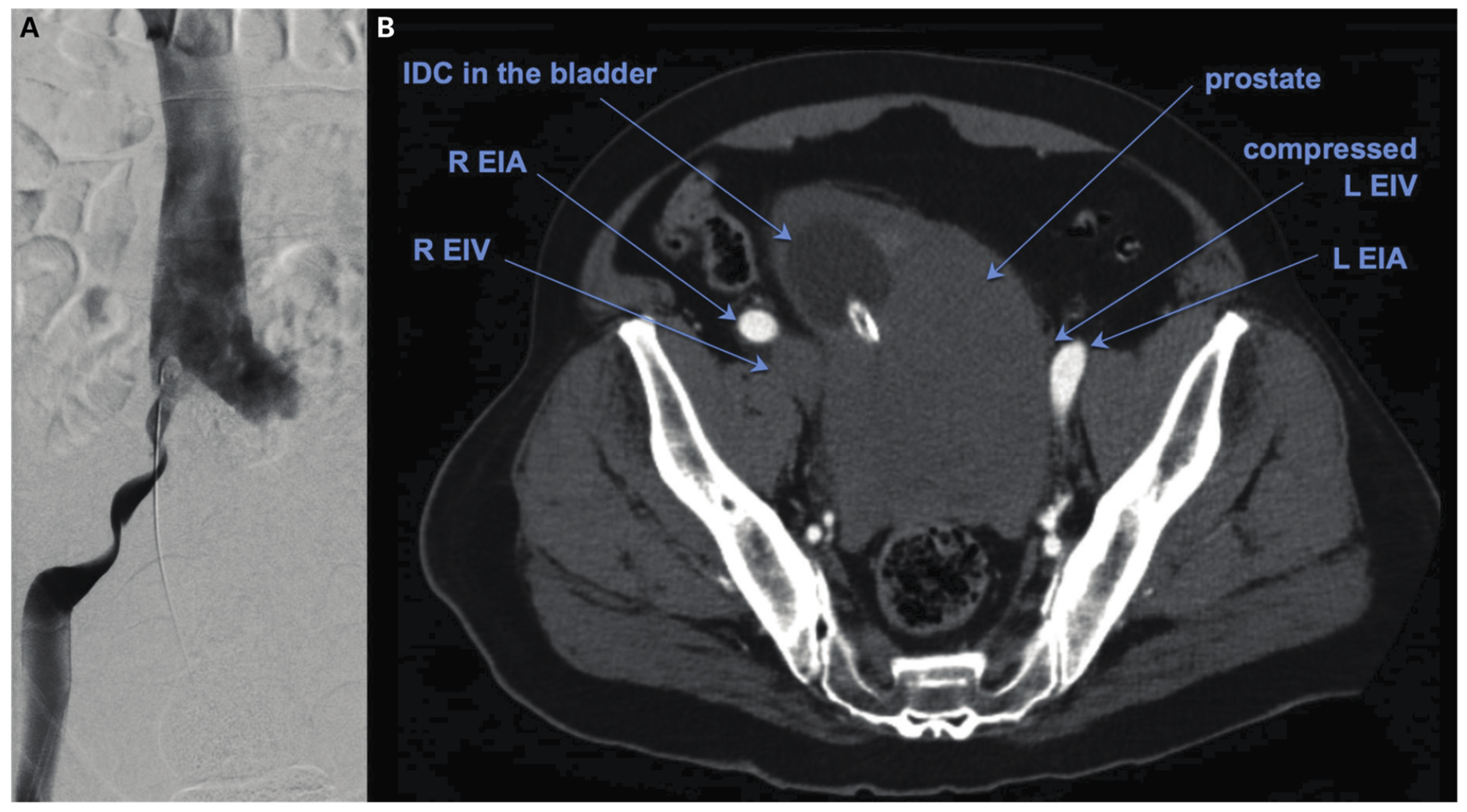
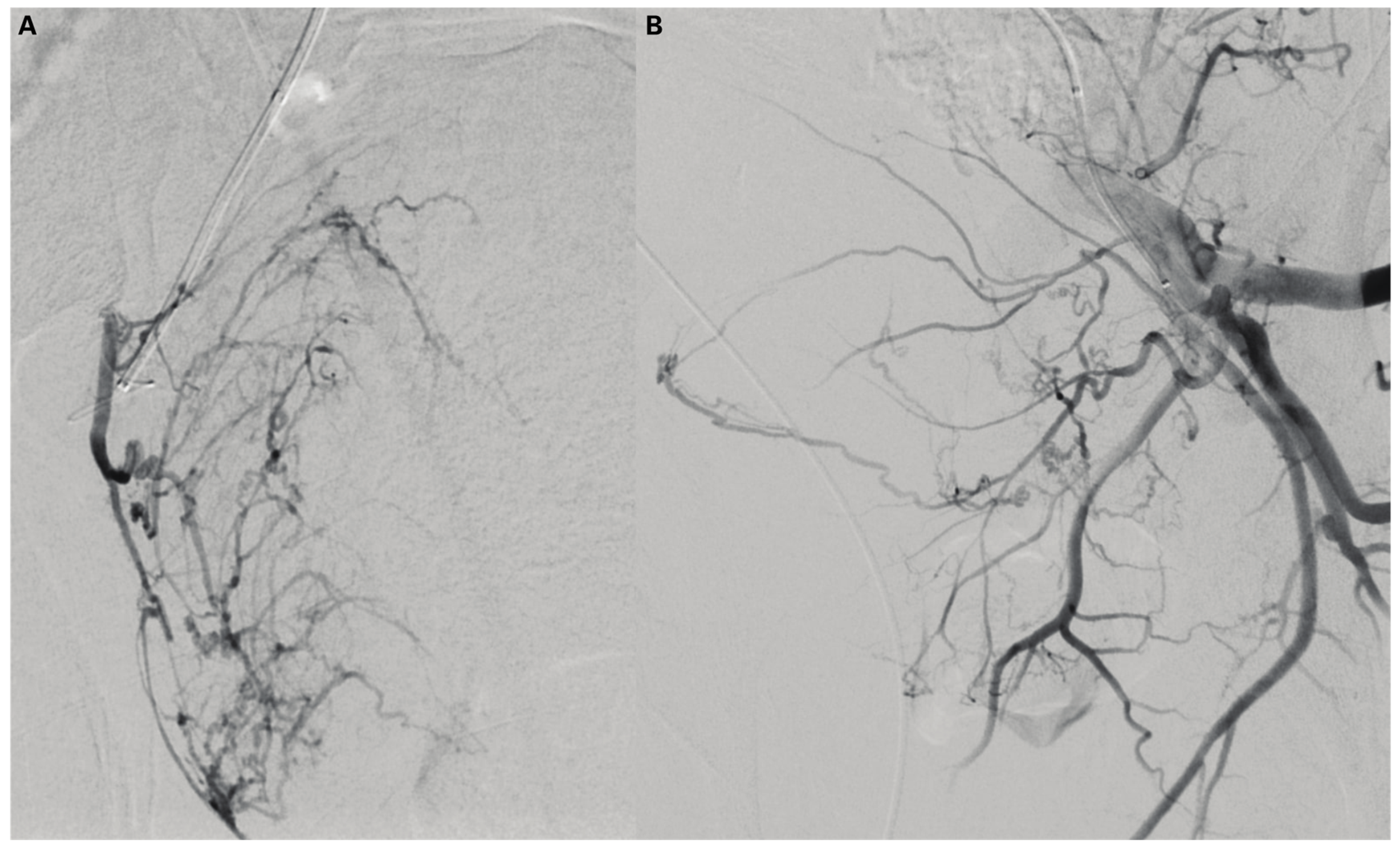
Prostate Artery Embolisation of Megaprostate Causing External Iliac Vein Compression
Conflicts of Interest
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2023 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.
Share and Cite
Nassour, A.-J.; Copping, R.; Bhoopathy, S.V.; Myint, M.; Mancuso, P.; Catt, J.; Schlaphoff, G. Prostate Artery Embolisation of Megaprostate Causing External Iliac Vein Compression. Soc. Int. Urol. J. 2023, 4, 495-496. https://doi.org/10.48083/LDJH4423
Nassour A-J, Copping R, Bhoopathy SV, Myint M, Mancuso P, Catt J, Schlaphoff G. Prostate Artery Embolisation of Megaprostate Causing External Iliac Vein Compression. Société Internationale d’Urologie Journal. 2023; 4(6):495-496. https://doi.org/10.48083/LDJH4423
Chicago/Turabian StyleNassour, Anthony-Joe, Ross Copping, Sankara V. Bhoopathy, Michael Myint, Pascal Mancuso, Jules Catt, and Glen Schlaphoff. 2023. "Prostate Artery Embolisation of Megaprostate Causing External Iliac Vein Compression" Société Internationale d’Urologie Journal 4, no. 6: 495-496. https://doi.org/10.48083/LDJH4423
APA StyleNassour, A.-J., Copping, R., Bhoopathy, S. V., Myint, M., Mancuso, P., Catt, J., & Schlaphoff, G. (2023). Prostate Artery Embolisation of Megaprostate Causing External Iliac Vein Compression. Société Internationale d’Urologie Journal, 4(6), 495-496. https://doi.org/10.48083/LDJH4423



