1. Introduction
Primary and secondary prevention and modern, up-to-date diagnosis are important challenges oncology faces today. This is due to a substantial number of new cases and the increasing rate of genitourinary cancer-related mortality worldwide. According to epidemiological data, cancers of the genitourinary system are the most common malignancies, especially in men. The second most common cancer in men is prostate cancer, with almost 1.3 million new cases worldwide (including 450 thousand in Europe) and more than 300 thousand deaths reported in 2018 [
1,
2,
3].
Bladder cancer is responsible for almost 200 000 deaths per year; more than 500 000 new cases worldwide are registered annually (including almost 200 000 in Europe) [
1,
2,
3]. In 2018, kidney cancer was diagnosed in 400 000 patients (including 136.5 thousand new cases in Europe) and caused 175 000 deaths worldwide (almost 55 000 in Europe) [
1,
2,
3]. As for testicular cancer, 71 000 new cases and 9.5 thousand deaths were reported worldwide in 2018 [
1,
2]. Other urogenital cancers are less prevalent. Testicular cancer predominantly occurs in adolescents and young men, whereas prostate cancer is highly prevalent in middle-aged and older men [
2].
There are many factors that affect cancer incidence, prevalence, recurrences, morbidity, and mortality; however, patients’ behaviour may play a critical role in the treatment progress [
4]. Adherence to treatment, including compliance with screening and medication protocol, self-examination, physical activities, taking care of mental health, avoidance of harmful occupational and environmental exposure, adequate diet, cessation or reduction of tobacco smoking and alcohol consumption, and many other activities may facilitate cancer treatment [
2,
4,
5,
6]. Nevertheless, most preventive and protective strategies depend on the patient’s health-awareness. In patients with urogenital cancer, starting treatment, intimate character of the disease, lack of education, advanced age, and other unfavourable factors warrant specific support from health care specialists.
Successful cooperation between the health specialist and the patient requires informed consent for planned therapeutic procedures. The information provided to the patient should be not only based on reliable medical knowledge (in accordance with the principles of evidence-based medicine) that is consistent and understandable but also individually tailored to the patient’s clinical situation. Involving the patient in therapeutic decisions, preceded by multifaceted education, has become a priority for clinicians throughout the medical world [
7].
2. Objectives
The purpose of our study was to develop an educational method that would effectively enhance health-awareness among cancer patients. A “real-life scenario” from a urologist’s consulting room was the basis for developing an educational method. The presentation of a concrete patient story was intended to draw attention to selected aspects concerning risk factors, diagnosis, and treatment. In addition, we attempted to obtain feedback from educational meeting participants to assess this form of knowledge transfer.
3. Materials and Methods
Four different “real-life scenarios” from a urologist’s consulting room that addressed prostate, kidney, bladder, and testicular cancers were prepared. The presentation of the scenes took place during an educational meeting for people keen on learning more about uro-oncology. The participants included members of “Gladiator,” uro-oncological patients’ organization [
8], as well as other survivors, supporters, friends, and patients’ relatives.
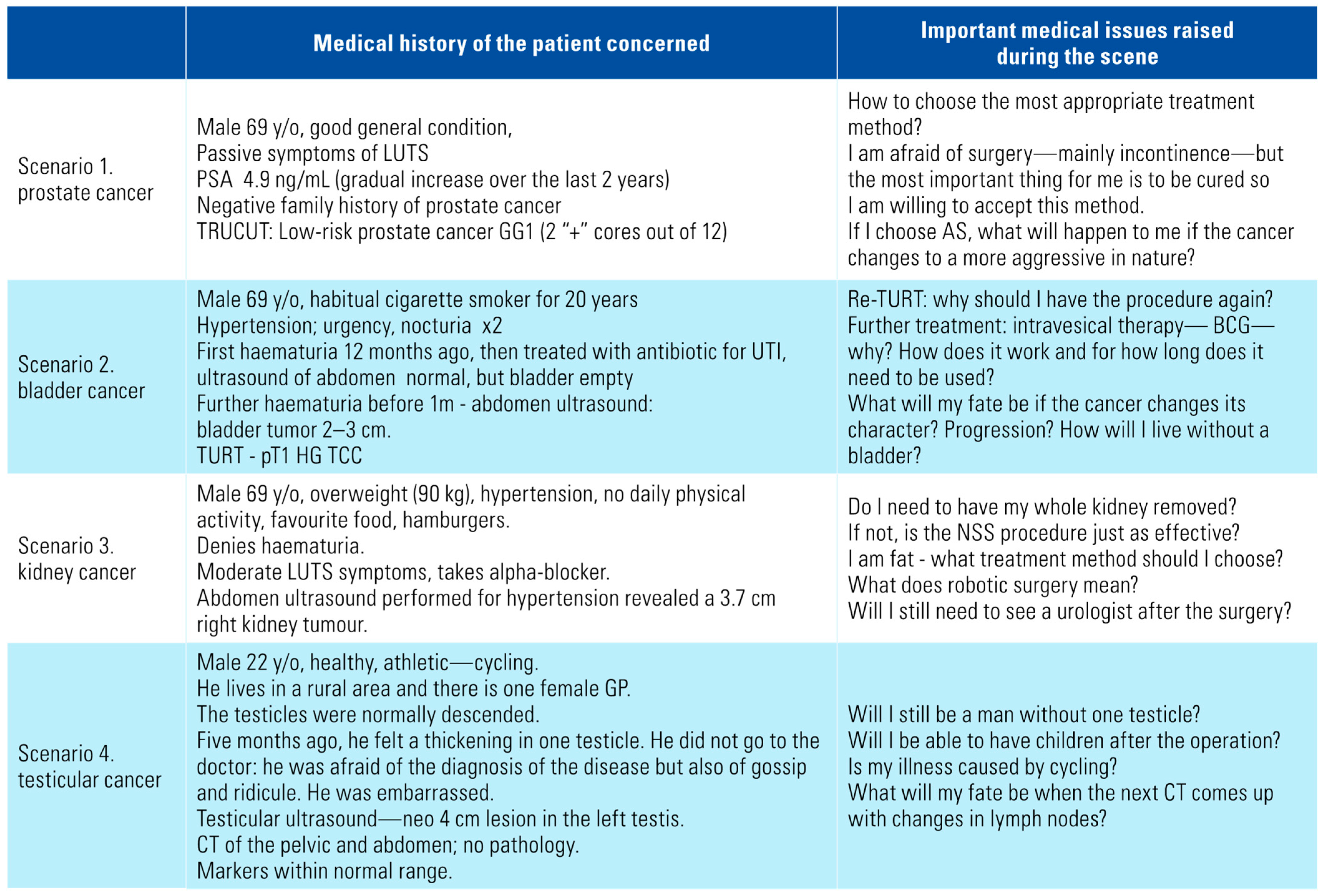
We had carefully prepared each scene in advance, based on our own clinical experience and prior discussions with members of Gladiator and other patients. Through the choice of topics in the scenes, we intended to draw particular attention to principal issues in selected uro-oncologic diseases. In terms of prevention and symptoms, the negative influence of tobacco on the development of urological tumors or the role of haematuria as an important urological symptom were particularly emphasized. After discussing the topics in detail with members of the Gladiator community, we decided to pay special attention to the issue of active surveillance as a safe, evidence-based treatment and nephron-sparing surgery as an effective therapeutic option and good oncological efficacy - these aspects are often raised by patients in conversations with doctors, which was pointed out by the members of Gladiator to the authors of this work. Overall, all scenarios included the most important cancer risk factors, typical symptoms, determination of the right moment for shared decision-making and follow-up after the treatment. Each scene in the urological consulting room consisted of subsequent modules: history-taking, discussion on clinical tests results, recommendations on various forms of therapy and analysis of possible side effects of the treatment and means of dealing with complications. Actors of the real-life scenario were urologists; one played the doctor and the other played a patient. After the presentation of each topic, a multidisciplinary team consisting of experts in urology, oncology, radiotherapy, and physiotherapy worked on the stage in the simulated neighbouring office. Experts gave commentaries and guidance for the patient, highlighting the most essential elements of the scene and, if necessary, answering questions from the participants (
Figure 1).
The scenarios of the scenes are presented in
Table 1. For better understanding of each treatment case, the results of medical tests, information from patients’ histories, treatment options, etc., were presented on a big screen in the form of slides (
Figure 1).
After the presentation of all the scenes, the participants were asked to fill in an 18-item questionnaire covering sociodemographic data (eg, place of residence, level of education), assessment of participants’ knowledge on genitourinary cancers, evaluation of the presented “scenes from urological consulting room” among others (the whole questionnaire is available in online Appendix 1). Before answering the questions, all participants provided informed consent. The experimental protocol and informed consent procedure were in compliance with the Helsinki Convention.
4. Statistical analysis
The questionnaire included questions with the possibility to enter a numerical value, to choose one option or mark multiple answers. When only one option was possible in the question, the percentage of each answer was referred to the number of respondents who had answered this question. When 2 or more answers were permitted, the percentage of each answer was related to the number of all answers. Frequency of responses was evaluated using chi-squared test. In the case of continuous variables, the multiple comparison was investigated by the Kruskal-Wallis test, followed by pairwise comparison analysis based on Scheffe’s procedure. P < 0.05 was considered statistically significant, unless otherwise indicated. The statistical analysis was performed in Matlab (MathWorks, Natick,, U.S.; ver. 2019b).
5. Results
Four separate scenes from the urologist’s office were presented according to a pre-determined plan. During the conversation between the “patient” and the urologist, relevant data such as results of laboratory tests were presented on a large screen above the stage (
Figure 1). After each cancer-related conversation, individual experts from the multidisciplinary team presented their comments. After all the scenes, 181 participants of the meeting completed the questionnaire. The participants could have experienced cancer personally, but it was not mandatory. The average age of respondents was 69.6 ± 6.3 years and 67% were between 65 and 75 years of age. 67% had primary or secondary education and 33% had higher education. 21% of respondents were living in a village, 35% in a city with up to 100 000 residents and 44% in a city with more than 100 000 residents. The group consisted of pensioners (80%), white-collar (15%) and blue-collar workers (5%); 14 people declared double status of employment.
A considerable proportion of participants indicated more than one source of information to increase their knowledge about the disease. The sources of information were
lectures by health professionals (30% of answers)
the Internet (29% of answers)
printed educational materials (19% of answers)
one-to-one peer support from other patients, family members and friends (11%)
scientific literature (7%)
other sources including television (5%).
As for websites, Gladiator webpage was chosen as the best source of information about “uro-cancer.” The second most popular Internet source was the website of the Polish Society of Urology.
Each scene (prostate, bladder, kidney and testicular cancer) was similarly appreciated, with 30% votes for the prostate cancer scene, 24% votes for the testicular cancer scene, and 23% for bladder and kidney cancer scenes each.
Participants’ knowledge of urogenital cancer was rated “poor” or “moderate” by 62%, “quite big” by 32%, and “extensive” by only 6%. Respondents living in a village, in a city with up to 100 000 or in a city of over 100 000 residents rated their knowledge about cancer significantly differently (
P < 0.01) (
Figure 2A). Forty-eight percent of people living in the countryside and only 6% of people living in a city with more than 100 000 residents evaluated their knowledge as poor (
Figure 2A). A total of 12% of subjects living in bigger cities (with more than 100 000residents) claimed that their knowledge about cancer was extensive, while none of the villagers marked this option (
Figure 2A).
Information presented during our educational meeting was understandable and rather understandable for 95% of participants. A statistically significant difference (
P < 0.01) was found in assessing the intelligibility of the presented information between white-collar workers, blue-collar workers, and pensioners (
Figure 2B). 89% of white-collar workers claimed that the lecture was fully understandable, while the material was fully understood by 76% of blue-collar workers and by 70% of pensioners (
Figure 2B).
The way of education provided during our meeting contributed to a significant increase of knowledge of cancer diseases according to 95% of the participants. For 98%, the presented material allowed to better understand the “patient’s path” with a given cancer at a given stage, and such a method was preferred in patients’ education. Concomitantly, the quality of the meeting content was assessed as “good” by 97% of the participants. Only 3% evaluated the lecture content as “moderate.” A total of 89% of the participants expressed their need for further education about cancer, while only 5% were not interested in continuing their education, and 6% of respondents hesitated about whether to learn or not.
6. Discussion
Health-awareness plays a key role in the prevention and treatment of cancer, and it precedes the shift towards patient involvement in health care decisions. Studies conducted so far have revealed that the health-awareness of uro-oncological patients is limited [
5,
9,
10,
11,
12,
13,
14,
15]. In a Dutch study that included 1793 urinary bladder cancer survivors, only 20% were able to report at least one possible cause for their cancer, with smoking being the most common causal explanation (10%), followed by occupational exposure (5%) and heredity (2%), while 80% of patients did not report any culprit [
9]. In another study [
10], 94.6% of urological patients considered smoking as a risk factor for chronic obstructive pulmonary disease, 92.1% for lung cancer, and 91.6% for heart and vascular problems, while only 58.4% were aware of smoking as a risk factor for bladder cancer. In the study by Yuruk et al. [
11], 46.5% of bladder cancer patients were aware of the connection between smoking and bladder cancer but only 4.1% of smoking patients were referred to smoking cessation programs. Patients’ awareness of the causal relationship between smoking and obesity and kidney cancer was significantly lower than their awareness of, for example, the relationship between smoking and lung cancer or obesity and colon cancer [
12]. Alarming evidence is emerging on the knowledge and performance of testicular self-examination: 88% of 275 male university students reported no knowledge on testicular self-examination; of the remaining 12% only 36% performed it [
15]. According to a Polish survey (204 respondents, average age 23.5 years, 93% associated with medicine), 33% did not know how to perform testicular self-examination; the respondents indicated school (46%) and media such as Internet or television (38%) as sources of information, whereas only 11% indicated a physician or a nurse [
16]. In a study investigating factors influencing health-awareness, more scanty knowledge of the disease was associated with increased age and lower education level among low-income prostate cancer patients [
14]. Importantly, well-educated patients are becoming better prepared for shared decision-making, which contributes to improving the effectiveness of therapy [
7].
In our study, the participants of the educational meeting were aware of their lack of knowledge of urogenital cancer; 62% rated their knowledge as poor or moderate, 32% as fairly high, but only 6% stated that they had an extensive knowledge of urogenital cancer. Moreover, 48% of respondents living in rural areas and 6% of residents of big cities rated their knowledge as “poor” (
Figure 2). “Fairly high” and “extensive” knowledge of cancer was declared by 54% of respondents living in urban areas, whereas among villagers, 28% rated their knowledge as quite big and none rated it as extensive. Based on the data obtained, there is no doubt that educational activities in the field of uro-oncology should be addressed particularly to people living in rural areas, and each such activity should be individualized, tailored to the possibilities and needs of a given group of recipients. Further research is needed to develop a final educational model. There is a possibility of using this concept in education conducted in smaller agglomerations, where patients would have easier access to a centre where meetings would take place.
There have been numerous studies evaluating the usefulness of the so-called decision-support tools, which include leaflets, videos or online materials presented to patients before or during a urological appointment. According to 2017 Cochrane review, including 105 of such studies conducted on a total of 31 043 people and involving a variety of clinical situations from across medicine, people who used decision-support tools felt better informed, and had better knowledge of the available treatment options and more accurate expectations about the benefits and possible harmful effects of these options. At the same time, decision-support tools did not negatively affect health outcomes or patients’ satisfaction [
17].
In relation to prostate cancer, among other things, the usefulness of leaflets distributed to patients, edited to raise awareness of screening, has been demonstrated [
18]. The benefit of supplementing traditional brochures with video-based information for prostate cancer patients prepared for radiotherapy has also been documented [
19].
Patients, for example those diagnosed with low-risk prostate cancer and under active surveillance, may experience anxiety about postponing the treatment and continuing to function with an identified, untreated cancer. They may also experience fear of disease progression, as well as stress caused by frequent medical examinations and the need for repeated prostate biopsies. A review of studies on the factors influencing therapeutic decision-making and the quality-of-life assessment in this group of patients has demonstrated a significant role of medical professionals and the key need for an individual approach, considering patients’ life experiences and expectations [
20].
Another available way to raise health-awareness is to draw on the experience of others affected by the same disease, for example through support groups in which patients share their experiences, either through face-to-face support (peer-to-peer) or social media on the Internet (online support groups). Both modalities are viewed positively by patients and have a significant impact on their treatment decisions, with older patients benefiting more from regular face-to-face support meetings, and younger patients more often using social media as an easily accessible and quick source of information, especially in emergencies [
21].
The diagnosis of cancer is a significant stress for the patient and his relatives. They look for comprehensible and reliable information to make therapeutic decisions. Despite many websites coming to rescue, patients still expect detailed information and direct recommendations from their physicians [
22].
The role of relatives, particularly female partners, in achieving appropriate health-awareness and making therapeutic decisions based on solid knowledge of the subject is crucial. Women have the potential to impact their household and family members’ health-seeking behaviours. Marital status has been a well-documented predictive factor for women regarding cervical and breast cancer screening, which is also true for prostate cancer screening in men [
23]. In a paper by Blanchard et al., 97% of married women reported some influence on health care decisions undertaken by their husbands with prostate cancer [
24]. Knowledge about prostate cancer was associated with marital status, income, age, and educational level of women [
24]. Therefore, it seems reasonable for women to participate in the process of educating men about prostate cancer or other uro-oncological conditions they may experience.
7. Limitations
Both the method of building health-awareness in uro-oncology proposed by the authors and the present study evaluating it have limitations. Playing scenes in the office creates organizational difficulties and requires prior preparation and discussion among professionals, which is time-consuming. It may also pose logistical difficulties because of the need to bring together as many patients as possible and at least a few professionals from different urological disciplines. The educational method we propose has the potential to be replicated on a larger scale, in particular with the use of modern means of communication, including the Internet. Potential archiving of the educational meeting in a video form and then making the recording available on the Internet, social media, educational websites, etc. allows free and repeated access (at any time) to educational materials and creates the opportunity for a potentially large audience. A certain limitation of the work is lack of detailed medical histories of participants affected by cancer, which may have influenced the degree of assessment of the educational scenes. Belonging to a patients’ organization may have resulted in some participants presenting more extensive knowledge of uro-oncology. The choice of specific topics for the scenes in the clinic considerably limits the scope of the issues discussed. Planning new (eg, suggested by the audience) topics to be discussed during subsequent educational meetings enables the continuous development of this method.
The presented survey was designed by us and was not adapted from any previously published study. Therefore, there is no validation, which limits the ability to assess the effectiveness of our method. Another limitation of our study is the lack of a tool to objectively measure the difference in urological awareness of participants before and after the meeting. Our goal was to evaluate the educational concept; therefore, all research methods and the whole concept require further research.
None of the methods used is perfect or sufficient by itself to provide comprehensive information for patients to make conscious decisions in the therapeutic process. In our opinion, combining different available methods and using them in the optimal way is an important part of modern uro-oncological awareness education. New methods used recently, such as social media or online support groups, have not been assessed in comprehensive studies. Moreover, their obvious limitation is the need to own and skilfully use electronic equipment with Internet access; this may pose a problem, given the age distribution of the urological cancer patient population. In addition, patients tend to verify any information found on the Internet during an individual conversation with a specialist [
25].
The proposed type of educational meeting would be a good compromise between the limited time allotted to an individual patient and patients’ needs. Finally, the assessment of the educational meeting and the feedback from participants fit in the concept of patient-centred outcome, which is aimed at giving patients an opportunity to arrange the agenda of educational meetings.
8. Conclusion
Methods of education tailored to the possibilities and expectations of cancer patients may increase their health-awareness and translate into clinical outcomes. We propose and report on a type of educational meeting, conducted in a group of patients and health professionals, which includes scenes of “real-life scenarios” from the urological consulting room. Patients are learning how to cope with cancer and treatment as well as getting involved in self-care and shared decision-making. The effectiveness and patients’ perception of this method, as well as its impact on therapeutic decisions and outcomes, require further research and evaluation. However, the presented results seem promising.