Abstract
Objectives: To review the methods of surgical complication reporting in urological journals, to determine the current utilisation of the Clavien Dindo classification, and to make comparison with previous reports over the last 10 years. Methods: A search was performed of all journal articles published in 5 major urological journals from January 2021 to April 2022, inclusive. All articles reporting surgical outcomes or complications were analysed. The current trend in complication reporting was compared with the results of the systematic search of the same 5 urological journals performed in 2012 by Yoon et al. Results: A total of 137 articles were identified. The Clavien Dindo classification was the most common method used (105/137, 76.6%) followed by a text-based descriptive classification (31/137, 22.6%). Notably, the Clavien Dindo classification was the only standardised method used in any of the articles examined. The prevalence of Clavien Dindo classification usage is 76.6% in the articles analysed in our search compared with the 33.3% reported by Yoon et al. in their search of papers published in the same 5 urological journals between 2010 and 2012. Conclusions: There has been a significant increase in the adoption of the Clavien Dindo classification in the reporting of complications in major urological journals in the last decade. This is a favourable trend which is likely in response to the ad hoc EAU Guidelines Panel 2012 recommendations. With more than 20% of journal articles still using descriptive text-based classifications, we should continue to encourage further implementation of standardised criteria, particularly the Clavien Dindo classification.
1. Introduction
The reporting of postoperative complications is fundamental for the assessment of surgical outcomes to promote quality improvement and innovation for best patient care. A uniform system of reporting facilitates universal and accurate grading of complications and easier comparison of reported experience for surgical procedures across time and across institutions [1,2]. In 2007, S. Machele Donat made clear the need for a standardised guideline for complication reporting for urological procedures [1]. She identified an alarmingly high percentage of studies reporting complications without uniform definitions or severity grading. Of studies that did report complication severity, most used qualitative categorisation with heterogeneity in definitions across studies, making cross comparison impossible [1].
Clavien et al. proposed a set of criteria for the reporting of postoperative complications based on the grade of treatment required for the complication in 1992 [3]. Postoperative treatments and therapeutic events are often well documented by nursing and medical staff during an admission [4]. This is proposed to be advantageous in reducing the under reporting of postoperative complications and particularly useful in retrospective evaluation [4,5]. In 2004, Clavien et al. updated their classification, increasing the number of grades from a 5 to 7, with increased emphasis on life-threatening complication and long-term disability to increase the applicability of the criteria across the surgical literature [4]. This modified version has since been referred to as the CDC and has had a broad uptake across surgical specialties (Online Supplementary Table S1) [6].
The objective of the CDC is to provide a simple, reproducible system for postoperative complication reporting that is devoid of imprecise and subjective terms such as “major” or “minor” [6]. In 2012, the EAU Guidelines Panel assessment made a recommendation for the use of the CDC for uniform reporting in urology, and in 2018, the EAU Guidelines Panel validated the CDC for use in the field of urology [3,6].
Yoon et al. in 2013 reported that between 2010 and 2012, the use of the CDC in the urological literature was 33.3% but found a trend to increasing uptake in that same period [7]. We anticipate this trend to have continued in the decade following the 2012 Ad Hoc EAU Guidelines Panel recommendations for uniform reporting of complications [2]. We examine the methods of complication reporting in major urological journals in 2021 and 2022 to determine the current use of the CDC in urological studies and to compare this with the results found 10 years ago by Yoon et al. [7].
2. Methods
We performed a search of all journal articles published from January 2021 to April 2022, inclusive, in European Urology, BJU International, The Journal of Urology, Urology, and International Journal of Urology. These 5 major urological journals were chosen for their impact factors and because they publish in English, and to enable direct comparison with the trends identified by Yoon et al. at the time of the EAU Guidelines Panel 2012 recommendations for uniformed reporting of complications [2].
A Medline index search was used to identify all articles reporting surgical outcomes in the 5 journals. The predefined search terms “operative” or “perioperative” or “postoperative” were combined with “outcome” or “complication,” “morbidity” or “adverse event” (Online Supplementary Table S2). The full text of each identified article was retrieved and individually evaluated to identify the methodology of complication reporting. Case reports, review articles, and letters to the editor were excluded, as were articles reporting on radiological imaging, intravesical chemotherapy or radiotherapy, and articles reporting no complications.
The articles identified and the methodology of surgical complication reporting were recorded in a standardised data extraction form for statistical analysis in Excel 2022. Complications reported by type of complication or using adjectival descriptors (such as major or minor) were categorised as a text-based descriptive classification. The proportion and percentage of articles using different reporting methodologies was calculated for each journal and across the journals. These findings were compared with the proportions and percentages reported in the 2013 systematic search of the same 5 urological journals by Yoon et al. to identify changes or trends [7].
3. Results
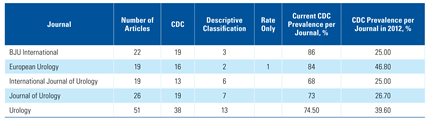
The Medline index search found 239 journal articles reporting on surgical outcomes in the 15 months from 1 January 2021 to 3 April 2022, inclusive (Online Supplementary Table S2). Application of the inclusion and exclusion criteria yielded 137 journal articles reporting 1 or more surgical complications (Figure 1).
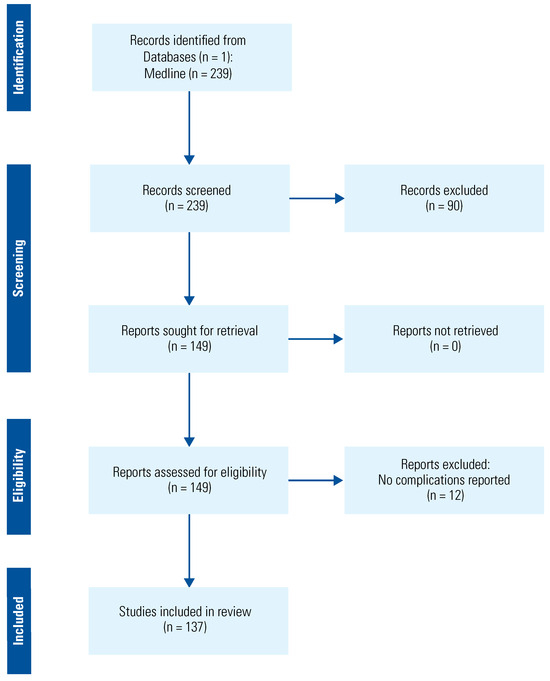
Figure 1.
Identification of studies for review.
The CDC was the most common method used (105 of 137 articles, 76.6%). The next most common classification system was text-based descriptive classification (31 of 137 articles, 22.6%). One article reported a complication rate but with no complication classification used (1 of 137, 0.7%) (Figure 2). Notably, the CDC was the only standardised method used in any of the articles examined.

Figure 2.
Methods of complication reporting.
Articles published in BJU International and European Urology had the highest rate of CDC use, (19 of 22 articles [86%] and 16 of 19 articles [84%], respectively) (Table 1). This is in keeping with the journals’ recommendation that authors use a recognized structured reporting system, which is considered further in the discussion below.

Table 1.
Methodology of complication reporting with current and 2012 CDC prevalence calculations: a breakdown by journal.
Our study found CDC usage of 76.6% compared with 33.3% reported by Yoon et al. in articles published in the same 5 urological journals between 2010 and 2012 [7]. We also found that CDC use accounted for 100% of standardised criteria used for complication reporting compared with 89.5% reported by Yoon et al. in 2010 to 2012 (Figure 3) [7].
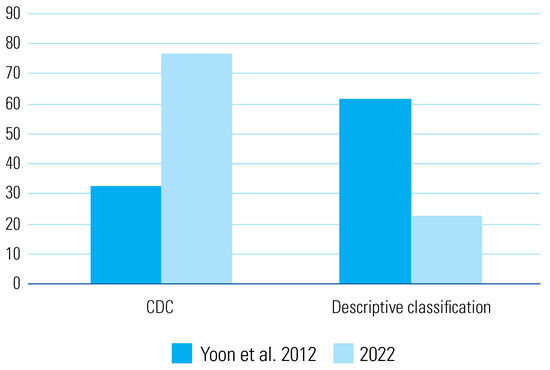
Figure 3.
Comparison of 2012 and 2022 classification use.
4. Discussion
Yoon et al. found increasing use of the CDC for postoperative complication reporting in 5 major urological journals between 2010 and 2012 [7]. The CDC had a prevalence of 21.4% in 2010, which rose to 50.2% by 2012 [7]. After the EAU Guidelines Panel 2012 recommendation for the use of the CDC, we sought to assess the current use of the CDC reported in the urological literature. In the same 5 urological journals from January 2021 to April 2022, the prevalence of CDC use was 76.6%. As search strategies differed, we cannot draw direct comparisons with the results from Yoon et al.; however, it is clear there has been a notable trend towards urologists favouring standardised reporting in the decade since the EAU recommendations [7]. This will allow standardised comparison of outcomes of surgical procedures within an institution, across institutions, and over time, leading to improved patient care and health economics [1,2,3,4,7].
Notably, 3 of the 5 urological journals assessed made recommendations with varied strength for use of a validated or structured reporting system within their journal inclusion criteria. The BJU International author guidelines state that the CDC “should” be used, European Urology guidelines“ encourage” authors to use a structured system and advise the use of CDC, whilst Journal of Urology includes “name of validated system” for complication reporting in the author checklist [8,9,10].Requiring validated and structured reporting systems or mandating use of the CDC to foster uniform reporting should be encouraged. Standardised complication reporting is likely associated with higher quality reporting. The 2012 ad hoc EAU Guideline Panel found that only 23% of papers reporting complications in urologic oncology fulfilled 7 or more of the Martin criteria for accurate and comprehensive reporting of surgical complications, compared with 77.9% of those that used the CDC system [2].
Translatable reporting with standardised criteria such as the CDC has particular benefit when comparing new surgical techniques. Donat described the difficulty in performing randomised control trials on surgical techniques, particularly with the continued introduction of more minimally invasive techniques in urology, and postulated that standardised complication reporting would allow for comparison of techniques in these circumstances [1]. The use of the CDC in describing complications of new techniques and in clinical trials is more evident in the literature [11,12] and should be encouraged.
A limitation of our paper is that we did not assess the correct application of the CDC, as this was considered beyond the scope of our investigation. Analysis of the studies using the Martin criteria would have been another method to assess the quality of complication in these papers [1,2,13]. The CDC has been recommended and validated for the reporting of only postoperative, and not intraoperative, complications in urology [2,6]. Despite this, in their 2018 validation survey, the EAU Guidelines Ad Hoc Panel found great inter-rater variability in responses assessing the applicability of the CDC to cases with intraoperative complications [6]. This may have arisen from the lack of a standard or recommended system for intraoperative complication reporting in the urological literature at the time. In 2019, the EAU ad hoc Complications Guidelines Panel proposed the Intraoperative Adverse Incident classification (EAUiaiC), which consists of 8 grades for reporting intraoperative complications for urological procedures [14].
Despite increasing use of the CDC in the urological literature, we found that 22.6% of papers still used non-standardised descriptive reporting of postoperative complications. Several concerns with the CDC have been raised, including the significant inter-rater variability, possible inapplicability to the paediatric population, lack of mechanism to differentiate between early and late postoperative complications, reporting only the single most severe complication in the postoperative period, and not considering the patient perspective [6,16]. These shortcomings may have contributed to the decision to use a descriptive style of reporting instead of the CDC in some of these studies. This has led to proposals for modification to the CDC, or alternatively for urology-specific or procedure-specific classifications to be implemented [6,15,16].
A recent proposal by the Complications After Major and Minor Urological Surgery (CAMUS) Collaboration is to produce a urology-specific system for complication reporting to rectify the apparent shortcomings of the CDC [16]. The CAMUS Delphi trial, to be completed by December 2023, is aiming to find a consensus in reporting [17]. The authors suggest consideration for structured and specific reporting parameters, reporting of patient risk profiles, inclusion of nursing and patient opinions, and prospective reporting in creating a future system for reporting in urology [16]. Although such a system would provide in-depth and comprehensive insight, the simplicity and ease of application of the CDC may facilitate its wide usage and help accelerate a trend towards uniform reporting across the literature [5].
5. Conclusions
The CDC have been widely adopted for reporting of postoperative complications in the urological literature in the decade since the EAU highly recommended its use. However, 22.6% of studies reporting surgical complications in the 5 major urological journals assessed did not use any form of standardised reporting. Limitations of the CDC have been identified, and in response, there have been proposals for a move towards comprehensive urology-specific or procedure-specific complication reporting systems. Despite the criticisms, the simplicity of the CDC makes it easy to apply and likely contributes to its growing use. Ultimately, the increasing use of CDC in the urological literature should be encouraged as it advances the field towards uniform reporting of complications.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/2563-6499/4/5/392/s1.
Funding
The authors declare no funding.
Institutional Review Board Statement
This investigation was performed following the principles of the Declaration of Helsinki. Ethics Committee approval was not required as the study did not involve human participants or animal care or use.
Data Availability Statement
The data sets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
Abstract Presentation: The abstract of this paper was presented at the 19th Urological Association of Asia (UAA) Congress as a poster presentation and at the 42nd Congress of the Société Internationale d’Urologie as an electronic poster with interim findings. The poster’s abstract was published in: (2022) Abstracts. Int. J. Urol. 29: 5–160: https://doi.org/10.1111/iju.15019 and in SIU Academy in the 42nd Congress event, training and education section: https://academy.siu-urology.org/siu/2022/the-42nd-congress-of-the-SIU/370932/amandeep.virk.prevalence.of.the.clavien.dindo.classification.in.the.reporting.html.
Conflicts of Interest
None declared.
References
- Donat, S.M. Standards for surgical complication reporting in urologic oncology: Time for a change. Urology 2007, 69, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Mitropoulos, D.; Artibani, W.; Graefen, M.; Remzi, M.; Rouprêt, M.; Truss, M. Reporting and grading of complications after urologic surgical procedures: An ad hoc EAU guidelines panel assessment and recommendations. Eur. Urol. 2012, 61, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Clavien, P.A.; Sanabria, J.R.; Strasberg, S.M. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery 1992, 111, 518–526. [Google Scholar] [PubMed]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Mitropoulos, D.; Artibani, W.; Biyani, C.S.; Bjerggaard Jensen, J.; Rouprêt, M.; Truss, M. Validation of the Clavien-Dindo Grading System in Urology by the European Association of Urology Guidelines Ad Hoc Panel. Eur. Urol. Focus 2018, 4, 608–613. [Google Scholar] [CrossRef] [PubMed]
- Yoon, P.D.; Chalasani, V.; Woo, H.H. Use of Clavien-Dindo classification in reporting and grading complications after urological surgical procedures: Analysis of 2010 to 2012. J. Urol. 2013, 190, 1271–1274. [Google Scholar] [CrossRef] [PubMed]
- Guide for Authors. Eur Urol. Available online: https://www.europeanurology.com/content/resources-for-authors#1500 (accessed on 10 April 2022).
- Author Guidelines. BJU Int. Available online: https://bjui-journals.onlinelibrary.wiley.com/hub/journal/1464410x/homepage/forauthors.html (accessed on 10 April 2022).
- Information for Authors. J Urol. Available online: https://www.auajournals.org/doi/10.1097/01.JU.0000553740.10987.2e (accessed on 10 April 2022).
- Bach, T.; Gilling, P.; El Hajj, A.; Anderson, P.; Barber, N. First multi-center all-comers study for the aquablation procedure. J. Clin. Med. 2020, 9, 603. [Google Scholar] [CrossRef] [PubMed]
- Yaxley, J.W.; Coughlin, G.D.; Chambers, S.K.; Occhipinti, S.; Samaratunga, H.; Zajdlewicz, L.; et al. Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: Early outcomes from a randomised controlled phase 3 study. Lancet 2016, 388, 1057–1066, https://doi.org/10.1016/S0140-6736(16)30592-X. Erratum in Lancet 2017, 389, e5. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.C., 2nd; Brennan, M.F.; Jaques, D.P. Quality of complication reporting in the surgical literature. Ann. Surg. 2002, 235, 803–813. [Google Scholar] [CrossRef] [PubMed]
- Biyani, C.S.; Pecanka, J.; Rouprêt, M.; Jensen, J.B.; Mitropoulos, D. Intraoperative Adverse Incident Classification (EAUiaiC) by the European Association of Urology ad hoc Complications Guidelines Panel. Eur. Urol. 2020, 77, 601–610. [Google Scholar] [CrossRef] [PubMed]
- Boeri, L.; Turetti, M.; Silvani, C.; Fulgheri, I.; Jannello, L.M.I.; Garbagnati, S.; et al. The comprehensive complication index as a tool for reporting the burden of complications after mini-percutaneous nephrolithotomy: Is it time to leave the Clavien-Dindo classification behind? World J. Urol. 2022, 40, 1829–1837. [Google Scholar] [CrossRef] [PubMed]
- Soliman, C.; Sathianathen, N.J.; Giannarini, G.; Wuethrich, P.Y.; Pan, H.Y.C.; Thomas, B.C.; et al. There is a need for a universal language in the reporting and grading of complication and intervention events to ensure comparability and improvement of surgical Care. Eur. Urol. 2022, 81, 440–445. [Google Scholar] [CrossRef] [PubMed]
- Soliman, C.; Mulholland, C.J.; Santaguida, P.; Sathianathen, N.J.; Lawrentschuk, N.; Giannarini, G.; et al. Protocol for CAMUS Delphi Study: A consensus on comprehensive reporting and grading of complications after urological surgery. Eur. Urol. Focus. 2022, 8, 1493–1511. [Google Scholar] [CrossRef] [PubMed]
- Page, M.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2023 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.