A Prospective Evaluation of Different Frailty Indices in Patients Undergoing Transurethral Resection of Bladder Tumor
Abstract
:1. Introduction
2. Methods
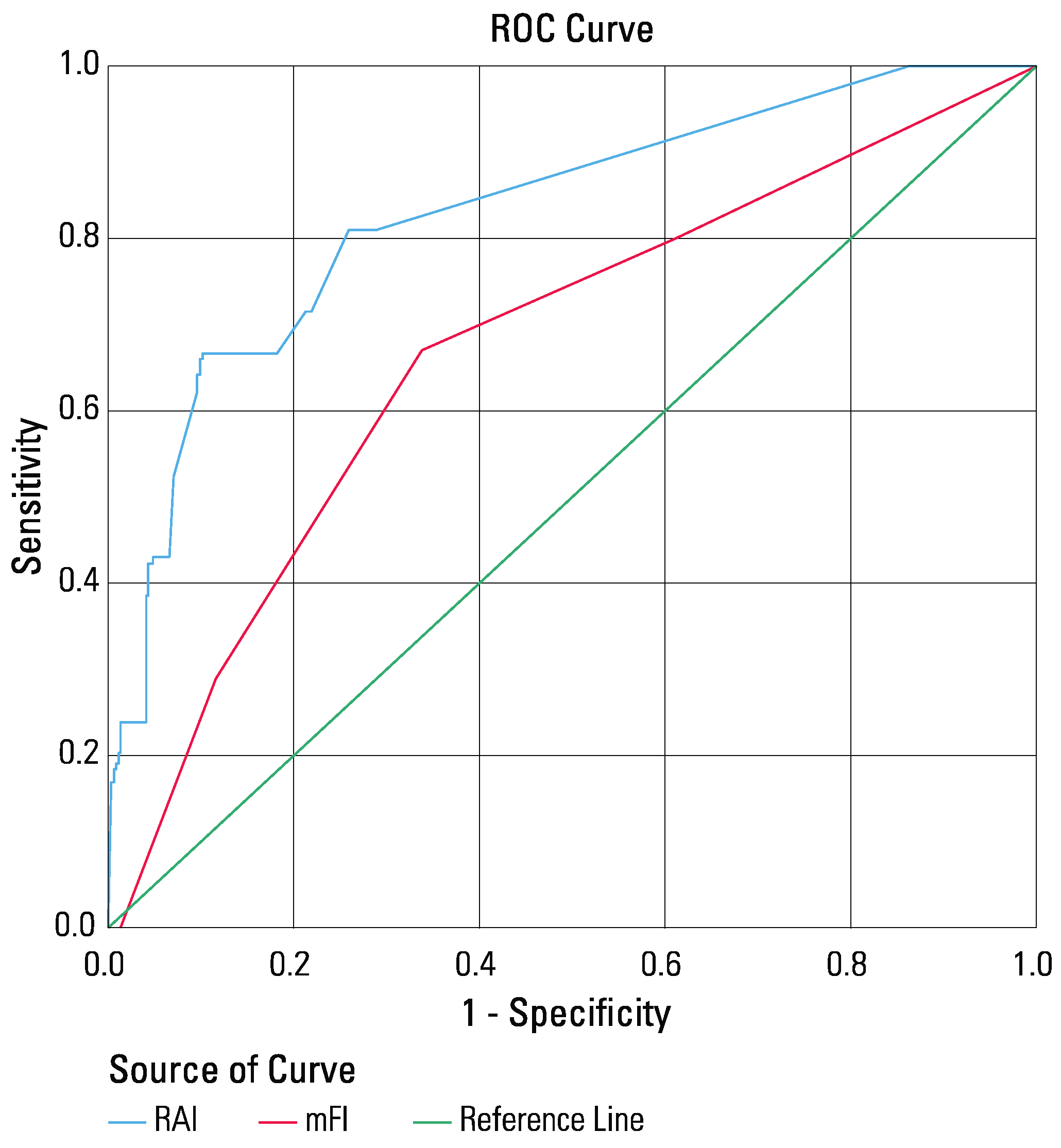
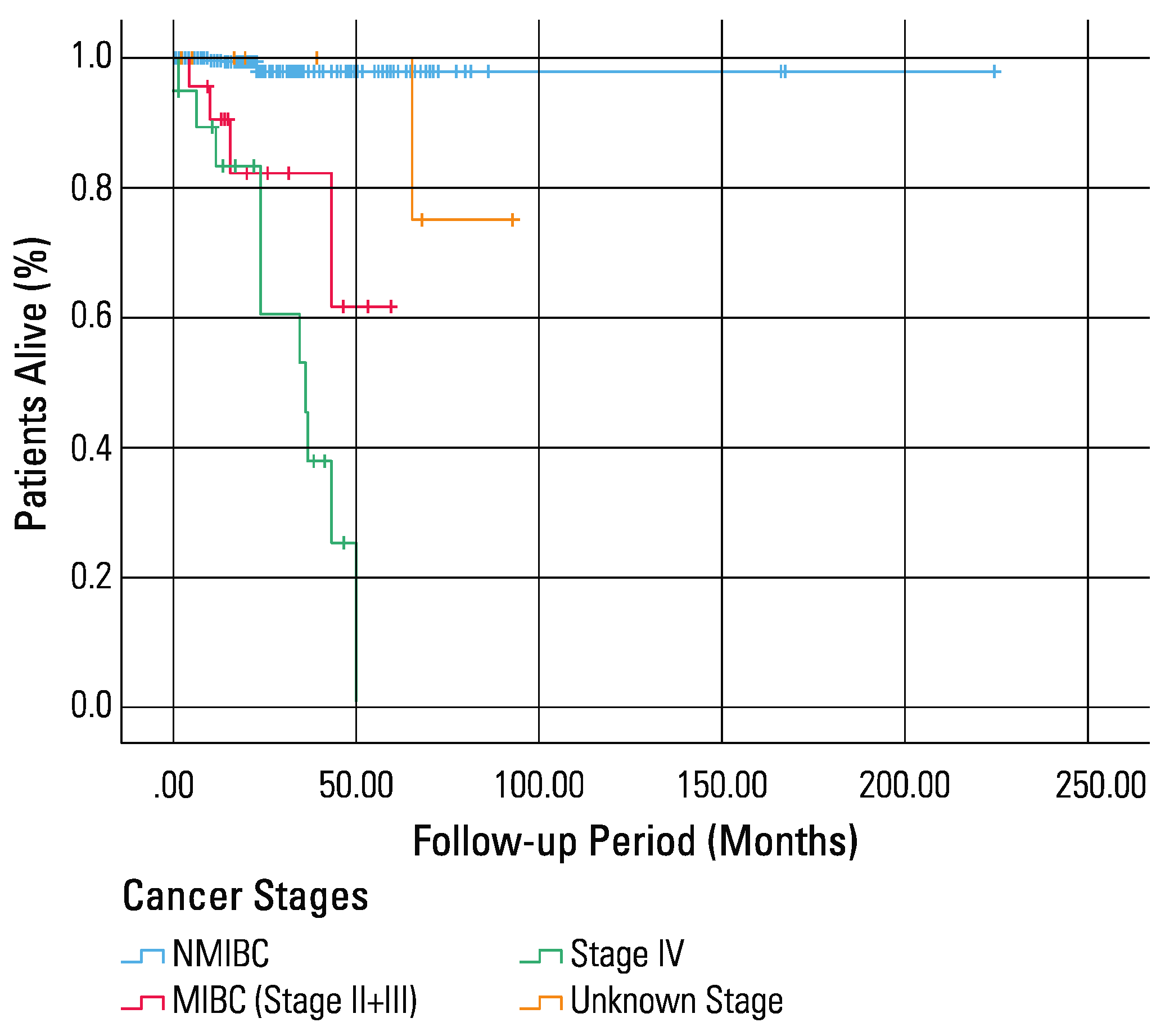
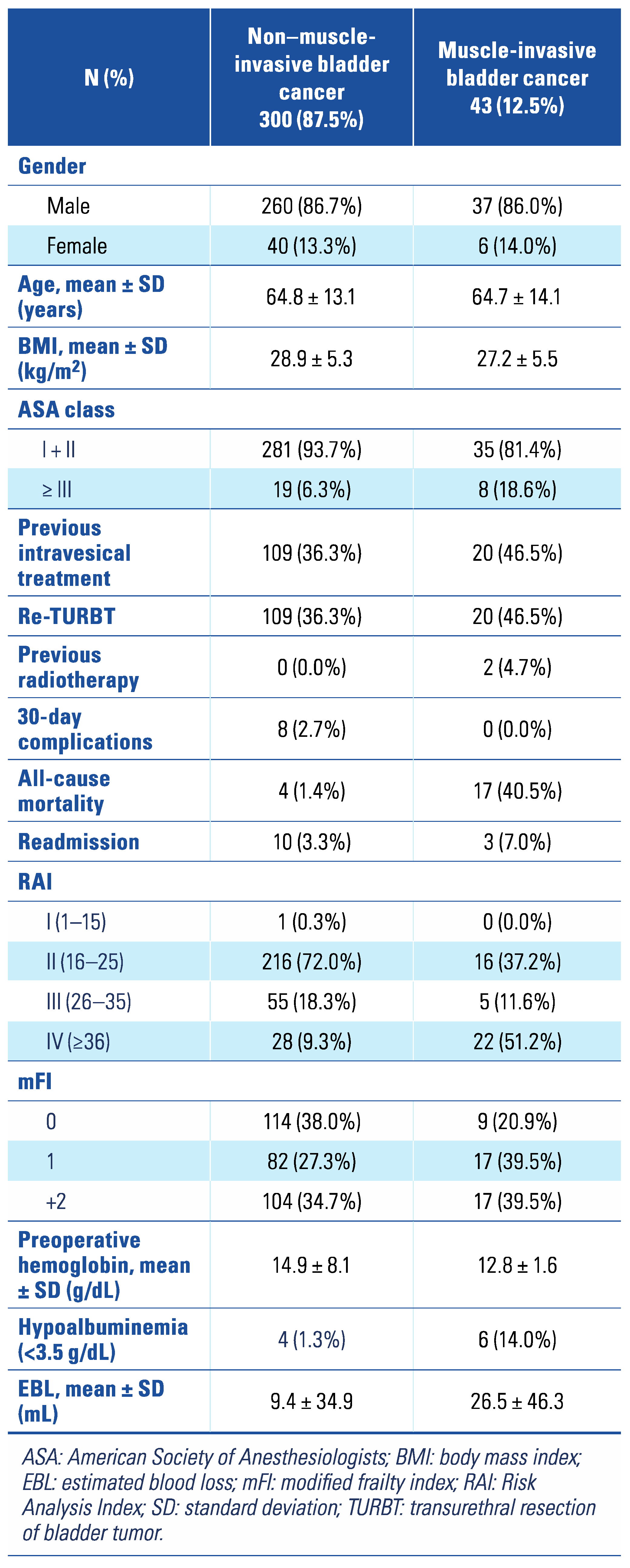
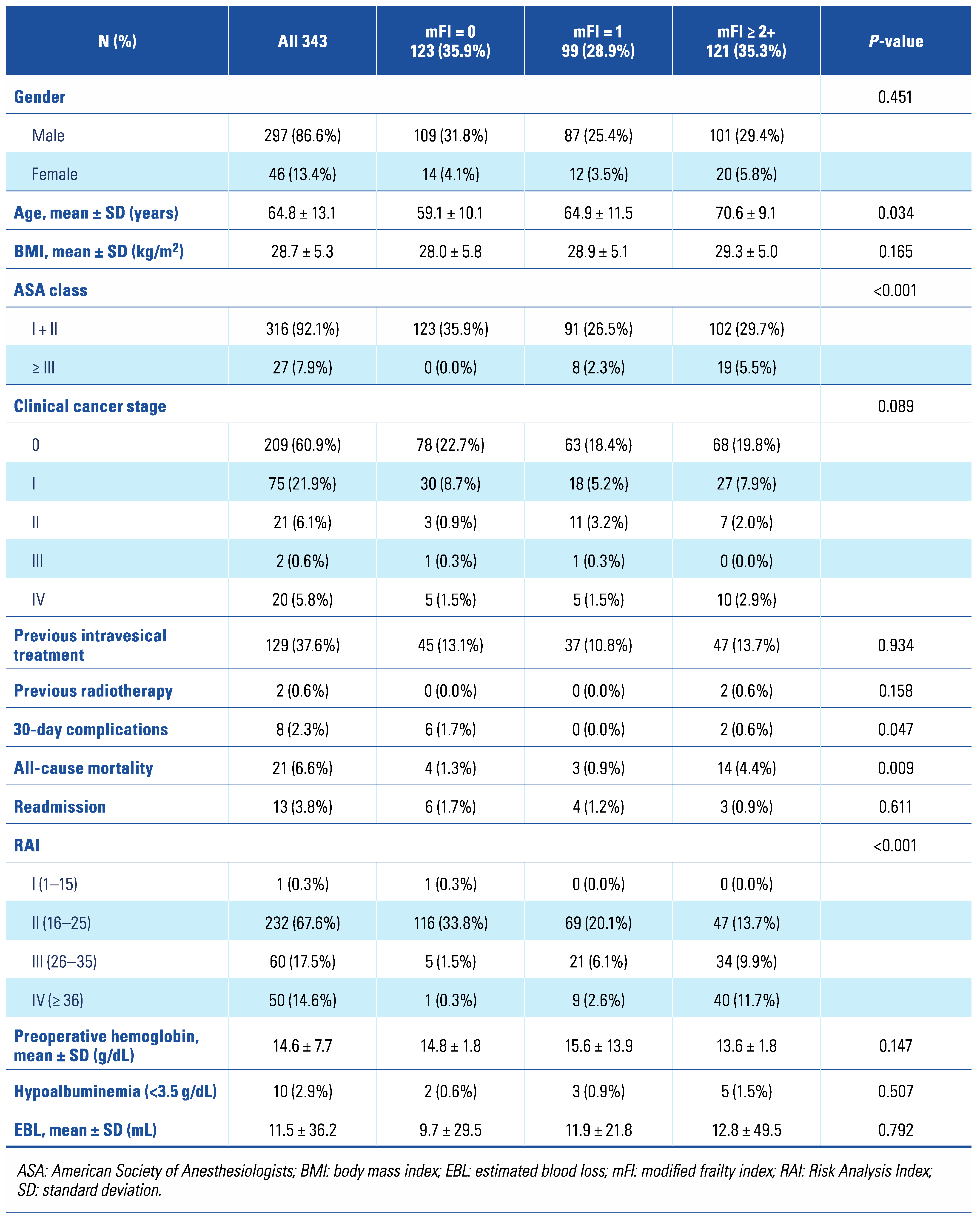
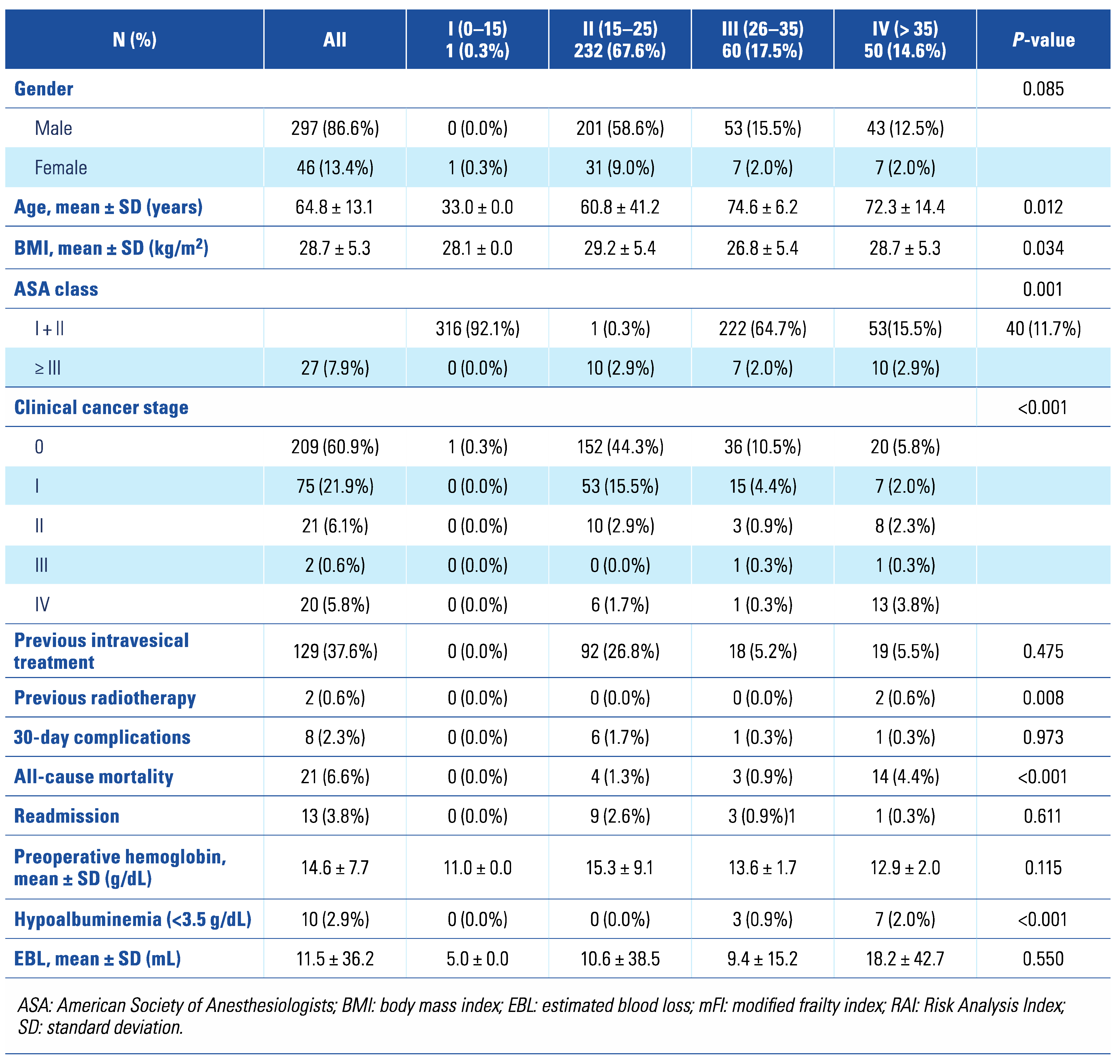
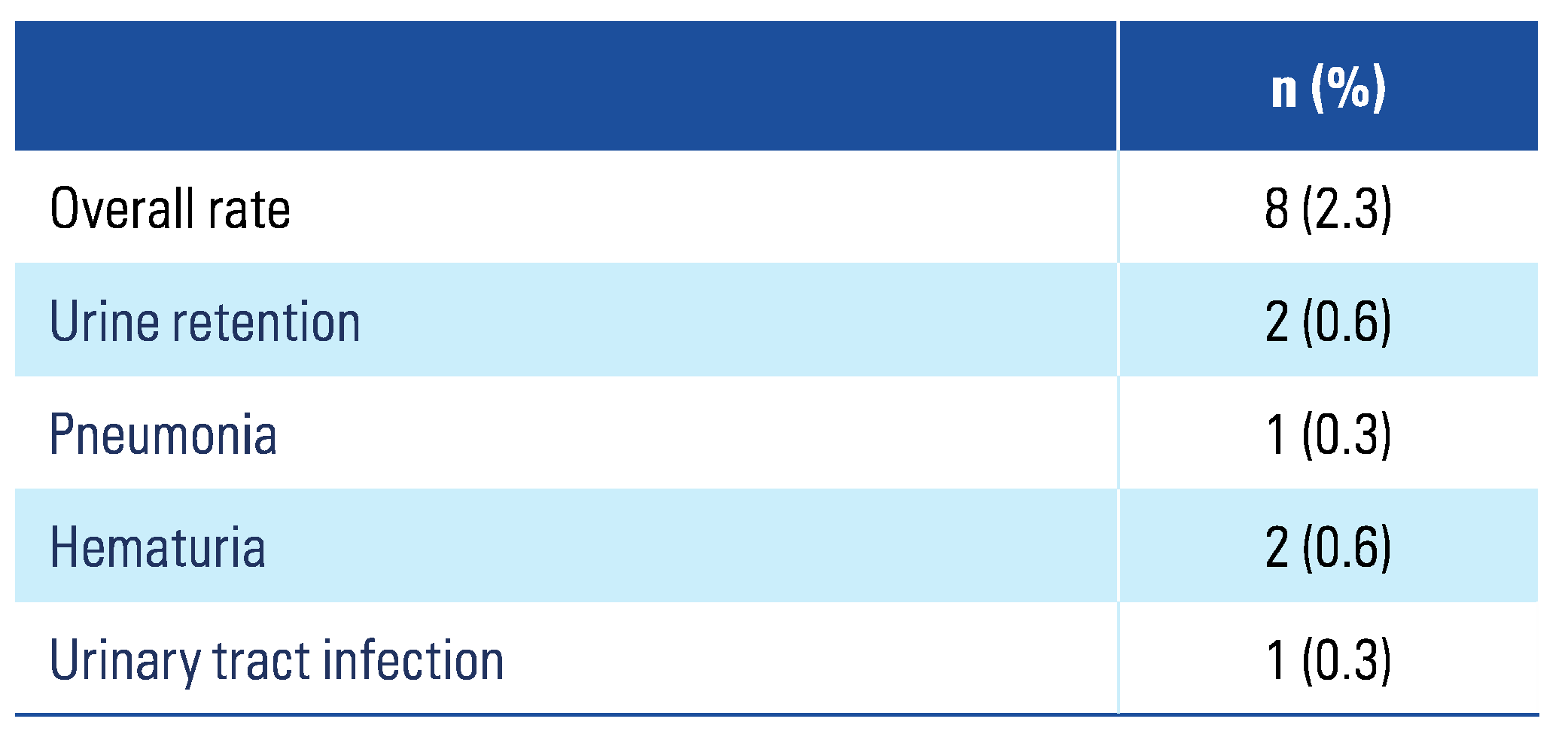
3. Results
4. Discussion
5. Conclusion
Conflicts of Interest
Abbreviations
| ASA | American Society of Anesthesiologists |
| AUC | area under the curve |
| CI | confidence interval |
| mFI | modified frailty index |
| MIBC | muscle-invasive bladder cancer |
| NMIBC | non–muscle-invasive bladder cancer |
| OS | overall survival |
| RAI | Risk Analysis Index |
| ROC | receiver operating characteristic |
| TURBT | transurethral resection of bladder tumor |
References
- Amrock, L.G.; Deiner, S. The implication of frailty on preoperative risk assessment. Curr Opin Anaesthesiol. 2014, 27, 330–335. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Anaya, D.A.; Johanning, J.; Spector, S.A.; Katlic, M.R.; Perrino, A.C.; Feinleib, J.; et al. Summary of the panel session at the 38th Annual Surgical Symposium of the Association of VA Surgeons: what is the big deal about frailty? JAMA Surg. 2014, 149, 1191–1197. [Google Scholar] [CrossRef] [PubMed]
- Buigues, C.; Juarros-Folgado, P.; Fernández-Garrido, J.; Navarro-Martínez, R.; Cauli, O. Frailty syndrome and pre-operative risk evaluation: a systematic review. Arch Gerontol Geriatr. 2015, 61, 309–321. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.-S.; Watts, J.N.; Peel, N.M.; Hubbard, R.E. Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr. 2016, 16, 157. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Traven, S.A.; Reeves, R.A.; Slone, H.S.; Walton, Z.J. Frailty predicts medical complications, length of stay, readmission, and mortality in revision hip and knee arthroplasty. J Arthroplasty. 2019, 34, 1412–1416. [Google Scholar] [CrossRef] [PubMed]
- Wahl, T.S.; Graham, L.A.; Hawn, M.T.; Richman, J.; Hollis, R.H.; Jones, C.E.; et al. Association of the modified frailty index with 30-day surgical readmission. JAMA Surg. 2017, 152, 749–757. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rothenberg, K.A.; Stern, J.R.; George, E.L.; Trickey, A.W.; Morris, A.M.; Hall, D.E.; et al. Association of frailty and postoperative complications with unplanned readmissions after elective outpatient surgery. JAMA Netw Open. 2019, 2, e194330. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Burg, M.L.; Clifford, T.G.; Bazargani, S.T.; Lin-Brande, M.; Miranda, G.; Cai, J.; et al. Frailty as a predictor of complications after radical cystectomy: a prospective study of various preoperative assessments. In Urologic Oncology: Seminars and Original Investigations; Elsevier, 2019; pp. 40–47. [Google Scholar]
- Chimukangara, M.; Helm, M.C.; Frelich, M.J.; Bosler, M.E.; Rein, L.E.; Szabo, A.; et al. A 5-item frailty index based on NSQIP data correlates with outcomes following paraesophageal hernia repair. Surg Endosc. 2017, 31, 2509–2519. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- 1Hall, D.E.; Arya, S.; Schmid, K.K.; Blaser, C.; Carlson, M.A.; Bailey, T.L.; et al. Development and initial validation of the Risk Analysis Index for measuring frailty in surgical populations. JAMA Surg. 2017, 152, 175–182. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shinall, M.C., Jr.; Arya, S.; Youk, A.; Varley, P.; Shah, R.; Massarweh, N.N.; et al. Association of preoperative patient frailty and operative stress with postoperative mortality. JAMA Surg. 2020, 155, e194620. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Voskamp, M.J.H.; Vermeer, M.; Molijn, G.J.; Cornel, E.B. The usefulness of the modified frailty index for muscle-invasive bladder cancer patients treated with radical cystectomy. Curr Urol. 2020, 14, 32–37. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chappidi, M.R.; Kates, M.; Patel, H.D.; Tosoian, J.J.; Kaye, D.R.; Sopko, N.A.; et al. Frailty as a marker of adverse outcomes in patients with bladder cancer undergoing radical cystectomy. In Urologic Oncology: Seminars and Original Investigations; Elsevier, 2016; p. 256–e1. [Google Scholar]
- Butros, S.R.; McCarthy, C.J.; Karaosmanoğlu, A.D.; Shenoy-Bhangle, A.S.; Arellano, R.S. Feasibility and effectiveness of image-guided percutaneous biopsy of the urinary bladder. Abdom Imaging. 2015, 40, 1838–1842. [Google Scholar] [CrossRef] [PubMed]
- 1Bryan, R.T.; Liu, W.; Pirrie, S.J.; Amir, R.; Gallagher, J.; Hughes, A.I.; et al. Comparing an imaging-guided pathway with the standard pathway for staging muscle-invasive bladder cancer: preliminary data from the BladderPath Study. Eur Urol. 2021, 80, 12–15. [Google Scholar] [CrossRef] [PubMed]
- Pereira, J.F.; Pareek, G.; Mueller-Leonhard, C.; Zhang, Z.; Amin, A.; Mega, A.; et al. The perioperative morbidity of transurethral resection of bladder tumor: implications for quality improvement. Urology 2019, 125, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Ferro, M.; Vartolomei, M.D.; Cantiello, F.; Lucarelli, G.; Di Stasi, S.M.; Hurle, R.; et al. High-grade T1 on re-transurethral resection after initial high-grade T1 confers worse oncological outcomes: results of a multi-institutional study. Urol Int. 2018, 101, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Shahait, M.; Labban, M.; Dobbs, R.W.; Cheaib, J.G.; Lee, D.I.; Tamim, H.; et al. A 5-item frailty index for predicting morbidity and mortality after radical prostatectomy: an analysis of the American College of Surgeons National Surgical Quality Improvement Program database. J Endourol. 2021, 35, 483–489. [Google Scholar] [CrossRef] [PubMed]


 |
 |
 |
 |
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2023 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.
Share and Cite
Abunaser, N.; El-Achkar, A.; Chaar, M.K.A.; Ababneh, A.; Halaseh, S.A.; Farkouh, A.; Abo-Hijleh, R.; Shahait, A.D.; Salah, S.; Shahait, M. A Prospective Evaluation of Different Frailty Indices in Patients Undergoing Transurethral Resection of Bladder Tumor. Soc. Int. Urol. J. 2023, 4, 187-194. https://doi.org/10.48083/NQEF6409
Abunaser N, El-Achkar A, Chaar MKA, Ababneh A, Halaseh SA, Farkouh A, Abo-Hijleh R, Shahait AD, Salah S, Shahait M. A Prospective Evaluation of Different Frailty Indices in Patients Undergoing Transurethral Resection of Bladder Tumor. Société Internationale d’Urologie Journal. 2023; 4(3):187-194. https://doi.org/10.48083/NQEF6409
Chicago/Turabian StyleAbunaser, Neebal, Adnan El-Achkar, Mohamad K. Abou Chaar, Ali Ababneh, Sattam A. Halaseh, Ala’a Farkouh, Ramiz Abo-Hijleh, Awni D. Shahait, Samer Salah, and Mohammed Shahait. 2023. "A Prospective Evaluation of Different Frailty Indices in Patients Undergoing Transurethral Resection of Bladder Tumor" Société Internationale d’Urologie Journal 4, no. 3: 187-194. https://doi.org/10.48083/NQEF6409
APA StyleAbunaser, N., El-Achkar, A., Chaar, M. K. A., Ababneh, A., Halaseh, S. A., Farkouh, A., Abo-Hijleh, R., Shahait, A. D., Salah, S., & Shahait, M. (2023). A Prospective Evaluation of Different Frailty Indices in Patients Undergoing Transurethral Resection of Bladder Tumor. Société Internationale d’Urologie Journal, 4(3), 187-194. https://doi.org/10.48083/NQEF6409





