The Hindi word “aatmanirbhar” means self-reliant. It became popular after the “Aatmanirbhar Bharat” policies of the current Indian government, and it was named Oxford Hindi Word of the Year 2020 [1].
The term should not be confused with being “self-contained” or “isolating away from the world” and it appropriately highlights the need for adopting this philosophy by Indian urological, surgical, and oncological communities with respect to penile cancer research.
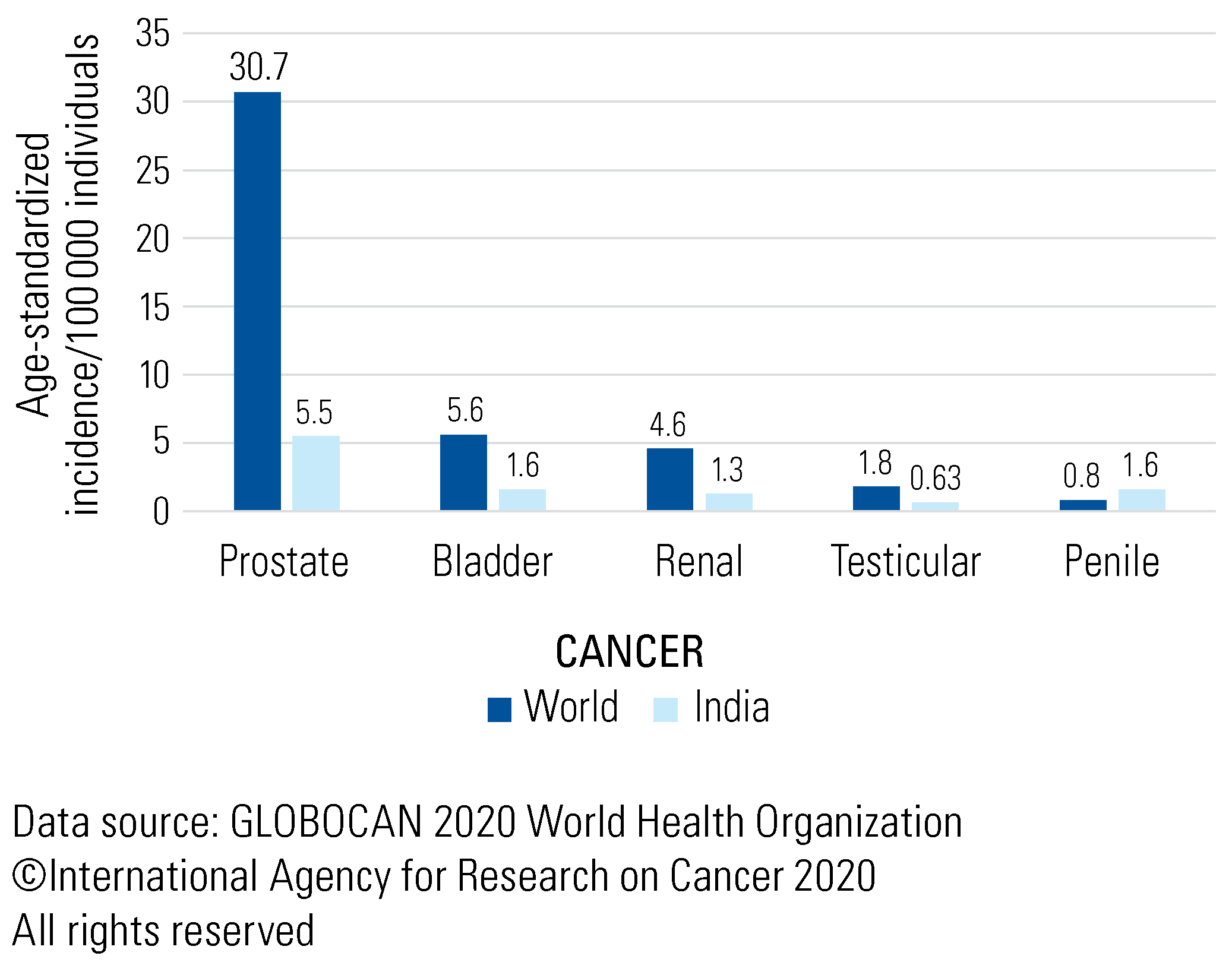
India has one of the highest incidences of penile cancer, with an age-standardized rate(ASR) of 1.4 and a crude rate of 1.3 which is almost the same as the rate for kidney cancer and not far behind that of bladder cancer [2]. In fact, penile cancer is the only urological cancer in which the ASR in India exceeds that of world (Figure 1). The European Union defines rare cancers as those with an incidence of less than 6 per 100000 population per year. By this definition, prostate, bladder, kidney, and penile cancers would all be considered rare in India. This is in contrast with high and high–medium-income countries (HIC, HMIC) where the incidence of penile cancer is much lower than that of other urological cancers. A recent editorial from the members of the newly formed Global Society of Rare Genitourinary Tumors (GSRGT) pointed out the dichotomy of penile cancer research and incidence: 90% of the publications related to rare genitourinary cancers come from HIC and HMIC, despite these countries having the lowest incidence of these cancers [3]. Despite having one of the highest incidences of penile cancer, India has hardly any ongoing clinical trials. The meagre involvement of low and low–middle-income countries (LMIC) in clinical and translational cancer research is well-documented. A recent study reported that only 8% of randomized clinical trials in oncology are from LMIC [4]. In other urological cancer sites, the evidence generated in HIC bridges the need for clinical practice in LIC and LMIC. For instance, even though > 60% of prostate cancer patients in India present with metastases compared with < 4% in the United States, almost all practice-changing evidence that transformed the management of meta- static prostate cancer in the last decade was generated in the United States, the United Kingdom, and Europe [5]. This however may not be possible with rare tumors like penile cancer. India should consider this as both a responsibility and an opportunity to lead the way in generating evidence for this not so rare cancer here.
Figure 1.
ASR of urological cancers in India versus the world.
The results of 2 recent surveys representing different parts of the world have clearly highlighted the lack of consensus and the variation in patterns of practice in penile cancer management. The first survey was conducted by eUROGEN across 10 European countries and found a significant variation in techniques of dynamic sentinel lymph node biopsy (DSNB) and templates and boundaries of inguinal lymph node dissection [6]. The more recent survey amongst 1003 members of the Society of Urologic Oncology (SUO) highlighted a poor utilization of DSNB despite strong evidence showing its oncological efficacy and favourable immediate and long-term morbidity [7]. While we expect similar lack of consensus amongst Indian centres, the difference is that we have the potential to answer many of these questions for ourselves and for the rest of the world. The implication of human papilloma virus (HPV) is being explored in the West in relation to aggressiveness of surgery of primary, selection of patients for radiotherapy, and prognostication. While similar studies have been done on Indian patients with head and neck cancers, for penile cancer even basic data about incidence and serotyping of HPV are lacking. Penile length has a global variation, and an Indian study found flaccid and stretched lengths of our men to be shorter than those in the western countries [8]. Shorter length combined with pre-pubic fat causes buried penis, which might translate into more patients requiring a total penectomy. Construction and validation of tools to gather quality of life information with respect to urinary and sexual function and options of penile reconstruction need exploration. The European Association of Urology risk stratification has been conventionally used since 2016 when it was first published. Recent studies have looked at factors that could better predict micro metastatic disease in clinically node negative groins, and it is encouraging to see 2 such large single-centre series from India [9]. Reflecting the findings of the SUO survey, the use of inguinal sentinel node biopsy in India is limited. The standardization of the more frequently used surgical procedure, its boundaries, and false negative rates are missing in urological guidelines, and India is clearly in a position to fill this gap. The perioperative management of node positive penile cancer patients has a series of unanswered questions related to chemotherapy, radiotherapy, sequencing, and extent. The InPACT trial is a pragmatically designed study which should put to rest many of these issues and can make a difference in the outcome of many patients globally [10]. Unfortunately, the trial has a slow accrual rate and although India sees a higher proportion of node positive patients at presentation and can potentially contribute significantly to the accrual rate of this trial, not even a single Indian centre has been on board for this study so far.
So, how to address this dichotomy of paucity of studies despite a higher incidence of disease in this part of the world? Lack of centralization of health and cancer care has been considered by some as a possible impetus. Considering the vastness of this country and variability in health insurance schemes, empowering decentralized cancer care is a more sustainable long-term solution. The National Cancer Grid (NCG) envisioned this almost a decade ago and has now close to 250 cancer centres on board [5]. One of the mandates of NCG is to facilitate basic, translational, and clinical research in cancer, and collaboration of centres treating penile cancer from NCG could be an easy pathway.
India has the advantage of having a spectrum of treatment modalities across its centres. Use of Tc99m-nanocolloid and or indocyanine green when DSNB is performed, and open, laparoscopic, or robotic approaches when the groins are addressed invasively, are all practiced in the same country. Collaboration across centres could convert this variation in treatment practice into an advantage that may not be possible in many other countries.
The ongoing pandemic has made it very clear that geographical distance is not an impediment to education, and collaborative research should follow the same path.
The Urological Society of India and the Association of Surgeons of India with its surgical oncology chapter (IASO) and NCG will support future penile cancer research that will put India on the map.
Conflicts of Interest
None declared.
References
- “Aatmanirbharta” selected as Oxford Hindi word of 2020. Times of India. February 4, 2021. Available at: indiatimes.com. Accessed September 28, 2022.
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021. [CrossRef] [PubMed]
- Bandini, M.; Ahmed, M.; Basile, G.; Watkin, N.; Master, V.; Zhu, Y.; et al. A global approach to improving penile cancer care. Nat Rev Urol. 2021, 19, 231–239, Erratum in Nat Rev Urol. 2022, 19, 253. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.C.; Sharma, S.; Del Paggio, J.C.; Hopman, W.M.; Gyawali, B.; Mukherji, D.; et al. An analysis of contemporary oncology randomized clinical trials from low/middle-income vs high-income countries. JAMA Oncol. 2021, 7, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Sirohi, B.; Chalkidou, K.; Pramesh, C.S.; Anderson, B.O.; Loeher, P.; El Dewachi, O.; et al. Developing institutions for cancer care in low-income and middle-income countries: from cancer units to comprehensive cancer centres. Lancet Oncol. 2018, 19, e395–e406. [Google Scholar] [CrossRef] [PubMed]
- Fankhauser, C.D.; Ayres, B.E.; Issa, A.; Albersen, M.; Watkin, N.; Muneer, A.; et al. Practice patterns among penile cancer surgeons performing dynamic sentinel lymph node biopsy and radical inguinal lymph node dissection in men with penile cancer: A eUROGEN survey. Eur Urol Open Sci. 2021, 24, 39–42. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Marilin, N.; Master, V.A.; Pettaway, C.A.; Spiess, P.E. Current practice patterns of society of urologic oncology members in performing inguinal lymph node staging/therapy for penile cancer: a survey study. Urol Oncol. 2021, 39, 439.e9–439.e15. [Google Scholar] [CrossRef] [PubMed]
- Promodu, K.; Shanmughadas, K.V.; Bhat, S.; Nair, K.R. Penile length and circumference: an Indian study. Int J Impot Res. 2007, 19, 558–563. [Google Scholar] [CrossRef] [PubMed]
- Sali, A.P.; Prakash, G.; de Cássio Zequi, S.; da Costa, W.H.; Murthy, V.; Soares, F.A.; et al. A comparative study of AJCC and the modified staging system in pT2/pT3 penile squamous cell carcinoma - a validation on an external data set. Histopathology. 2022, 80, 566–574. [Google Scholar] [CrossRef] [PubMed]
- Canter, D.J.; Nicholson, S.; Watkin, N.; Hall, E.; Pettaway, C.; InPACT Executive Committee. The International Penile Advanced Cancer Trial (InPACT): Rationale and Current Status. Eur Urol Focus. 2019, 5, 706–709. [Google Scholar] [CrossRef] [PubMed]
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2022 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.