Abstract
In this report, we look at the relationship between prior circumcision and presenting stage of penile cancer. We performed an analysis of an international, multicenter database of 1254 penile cancer patients diagnosed from 1980 to 2019 in the United States, Europe, Brazil, and China, and analyzed the relationship between circumcision and presenting T and N stage. A total of 710 patients met the inclusion criteria and were statistically analyzed. We found that uncircumcised men with locally advanced tumors (T3–T4) had significantly higher risk of lymph node metastasis compared with circumcised men.
The genital microbiome is the only shared human microbiome [1]. Since circumcised men harbor different bacterial communities than uncircumcised men [2], we hypothesized that circumcised men may present with a different penile squamous cell carcinoma (PSCC) disease burden than uncircumcised men. Were this the case, it could manifest as a difference in either the T or N stage of the subsequent disease. To our knowledge, no prior study has discussed the relationship of prior circumcision with the presenting tumor stage. In order to do so, we performed a retrospective cohort study.
Large clinical datasets of patients with PSCC are uncommon given the rarity of the disease [3]. We have collaborated on an international, multicenter retrospective database of 1254 penile cancer patients diagnosed from 1980 to 2019 in the United States, Europe, Brazil, and China. Previous publications from our group have discussed correlates of chemotherapy and lymph node dissection use by participating institutions [4,5,6], and association between human papillomavirus (HPV) infection and radiosensitivity [7]. For this report, we analyzed the relation between circumcision and presenting T and N stage. Patients treated with circumcision during the surgery of the primary lesion or those without data on time of circumcision were excluded.
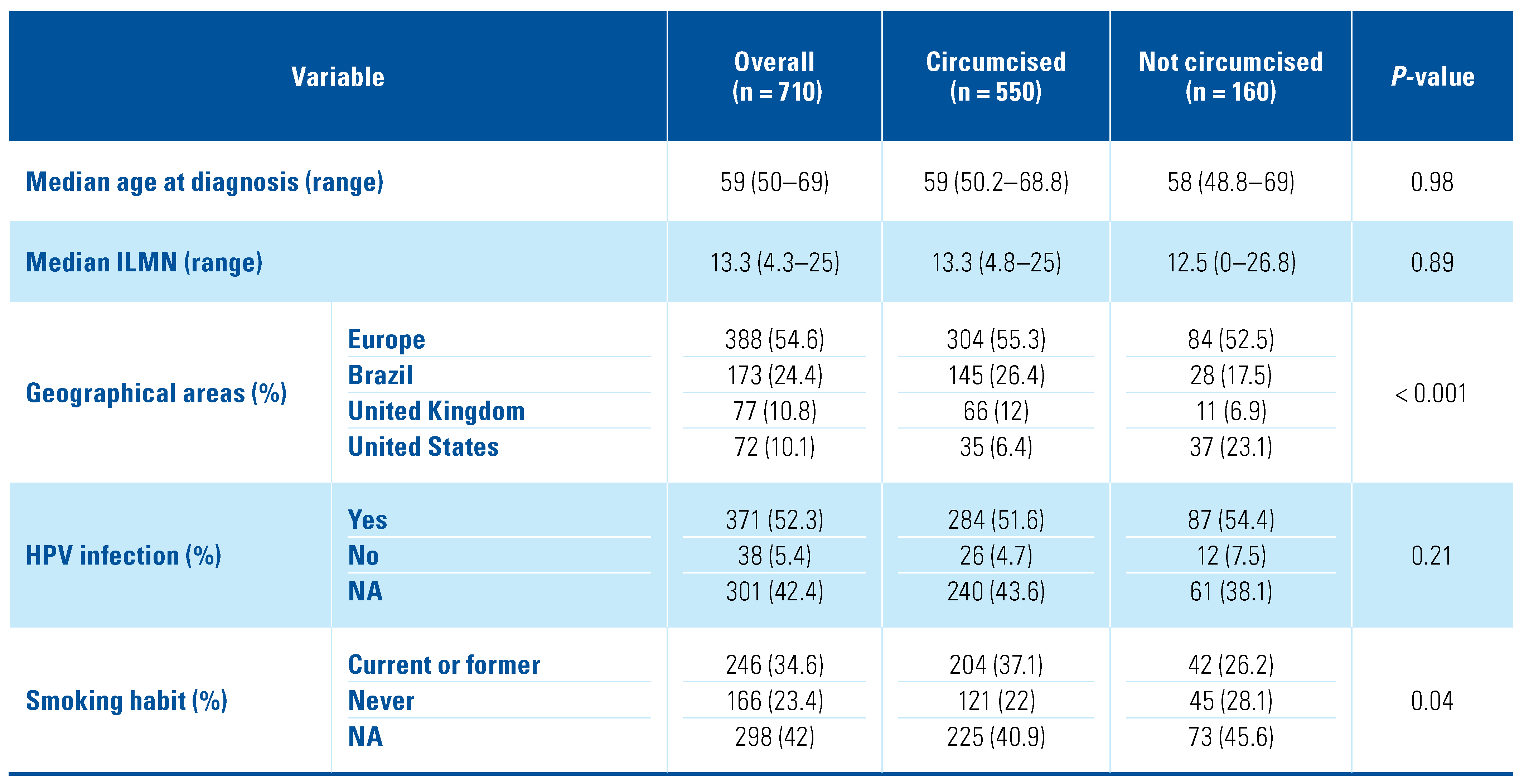
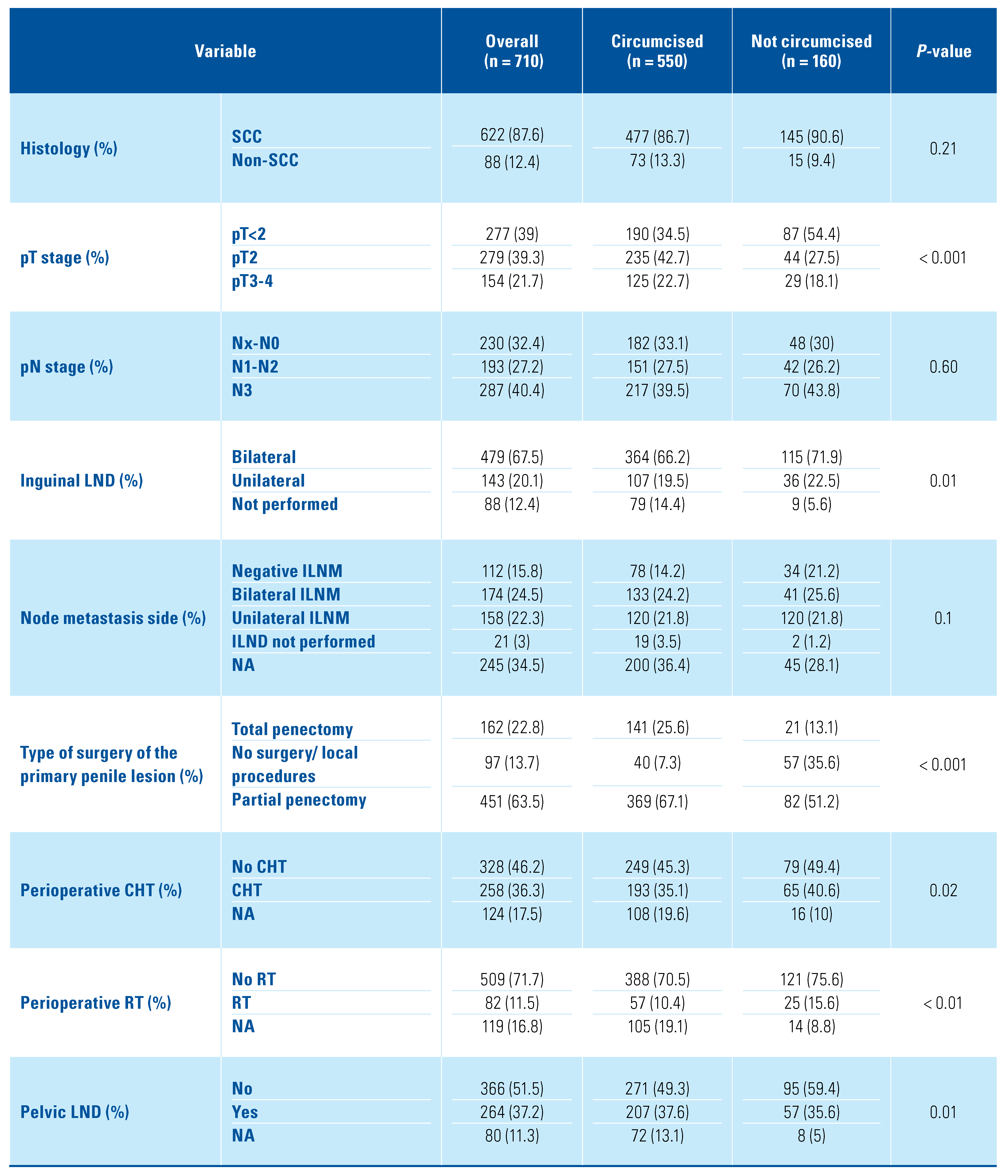
For this analysis, 710 patients met the inclusion criteria (Figure 1). Patient characteristics are summarized in Table 1. Descriptive statistics included frequencies and proportions for categorical variables. Medians and interquartile ranges (IQR) were reported for continuous variables. The statistical significance of differences in medians and proportions between circumcised and uncircumcised men with penile cancer was tested with the Kruskal-Wallis and chi-square tests, respectively.
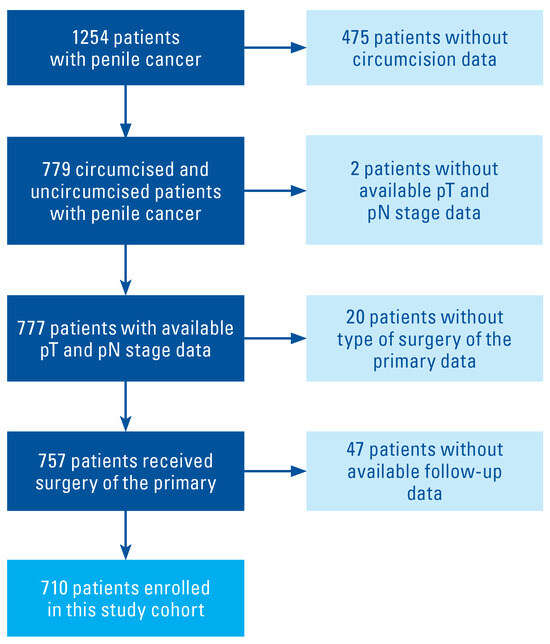
Figure 1.
Inclusion/exclusion criteria and study population.

Table 1.
Epidemiological, geographical, and disease-specific characteristics of 710 penile cancer patients treated within 9 tertiary referral institutions.
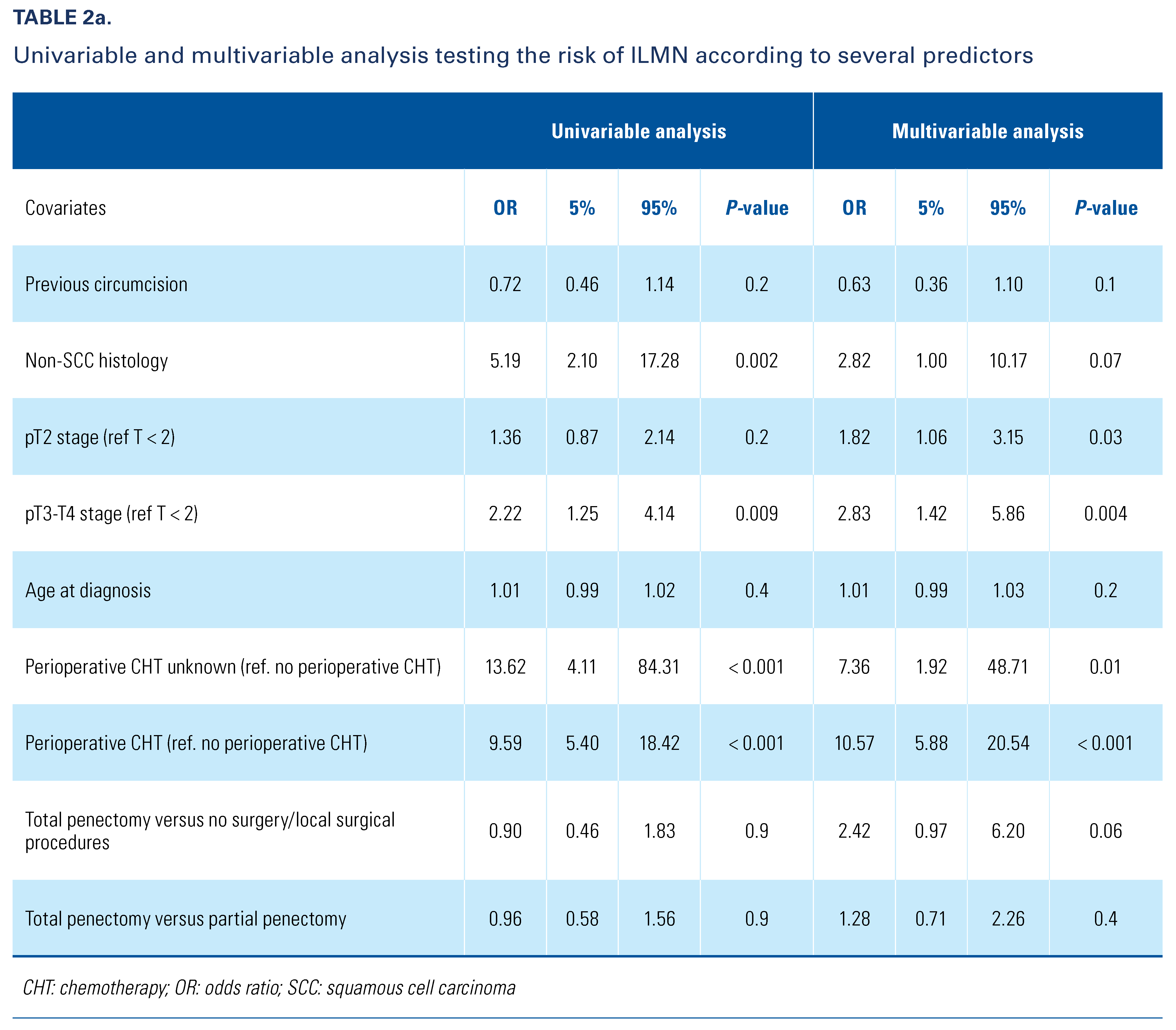
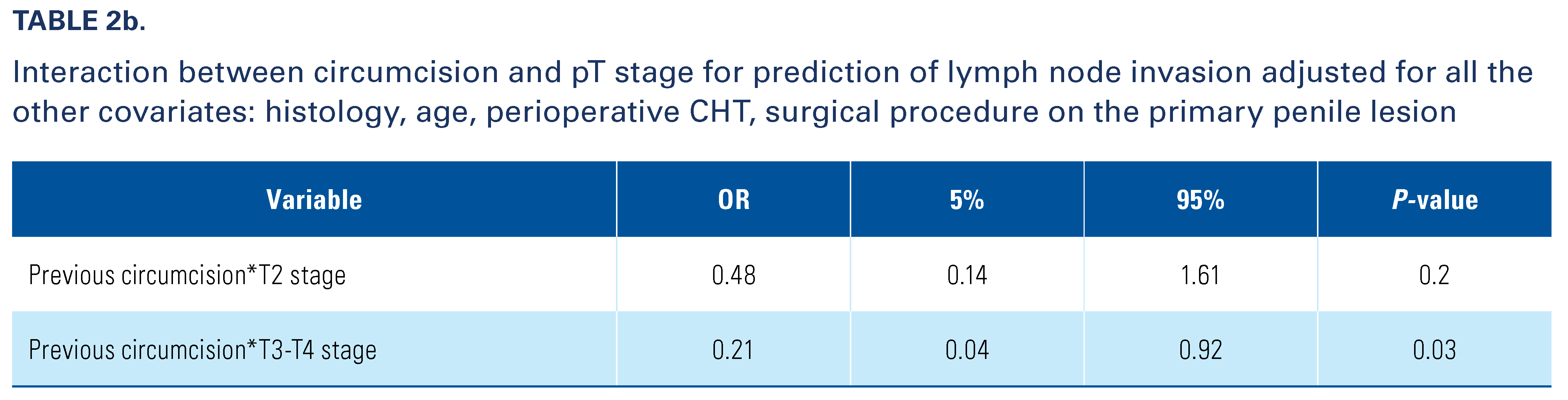
Analyses were organized in several steps. First, we explored predictors of inguinal lymph node metastases (ILNM) among several variables including circumcision, histology (squamous cell versus non- squamous cell), T stage (T< 2 versus T2 versus T3–T4), age at penile cancer diagnosis, use of perioperative chemotherapy, surgical procedure to the primary (total penectomy versus partial penectomy versus no surgery/ local surgical procedures). The choice of the predictors for this multivariable model has been made based on clinical relevance. Second, to assess whether the higher risk of ILNM in locally advanced tumors (T3–T4) was different by circumcision status, we tested an interaction with T stage and circumcision. Third, we depicted the probability of inguinal lymph node metastases for circumcised and uncircumcised men with penile cancer across T sub-stages.
Uncircumcised patients harbored T< 2 tumors more frequently than did circumcised men (54.4% versus 34.5%; P < 0.001) (Table 1). No statistical difference was found regarding N stage between circumcised and uncircumcised men. Furthermore, circumcision rates differed with smoking and geographic patient variables, and with several treatment variables including extent of surgery and delivery of chemotherapy and radiother- apy. Multivariable analyses showed a clear and expected association between advanced pT stages and higher risk of ILNM, as well as between use of perioperative chemo- therapy and higher risk of ILNM. Conversely, no asso- ciation was found between circumcision and the risk of ILNM. Nevertheless, we found that circumcision, compared with no-circumcision, conferred a lower risk of ILNM (Table 2) in patients with locally advanced tumors (T3–T4). The risk of ILNM according to T stage in circumcised versus uncircumcised penile cancer patients is depicted in Figure 2.

Table 2.
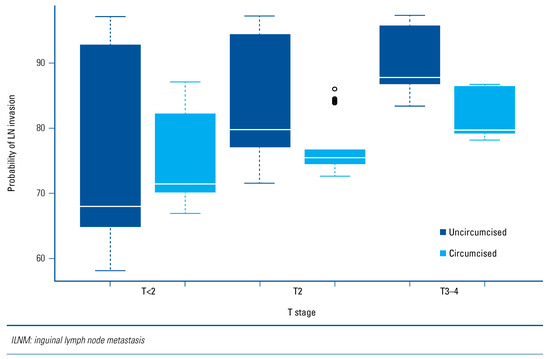
Figure 2.
Risk of ILNM according to T-stage in circumcised versus uncircumcised penile cancer patients.
Debate continues about the potential role of circum- cision in subsequent development of PSCC [8,9]. To our knowledge, no prior study has discussed the association of prior circumcision with tumor stage at presentation. Our data reveal correlations between circumcision and PSCC staging. First, there is an association of prior circumcision with presenting T stage on multivariable analysis. Second, there is no association of circumcision with presenting N stage. These findings suggest there may be a difference in local microbiota in uncircumcised compared with circumcised individuals, which might contribute to development of PSCC.
Limitations of this analysis include a lack of broad generalizability, since data are lacking from Africa, India, and most of South America, and we consider our coverage of North America and Europe to be subopti- mal. Lack of data on HPV status on these patients is a limitation in terms of understanding its potential etiol- ogy in penile cancer, most notably in non-circumcised men. Specific analysis of large populations with equal access to health care would help clarify the potential role of the genital microbiome in this process.
Conflicts of Interest
None declared.
References
- Liu, C.M.; Hungate, B.A.; Tobian, A.A.; Ravel, J.; Prodger, J.L.; Serwadda, D.; et al. Penile microbiota and female partner bacterial vaginosis in Rakai, Uganda. mBio 2015, 6. [Google Scholar] [CrossRef] [PubMed]
- Nelson, D.E.; Dong, Q.; Van der Pol, B.; Toh, E.; Fan, B.; Katz, B.P.; et al. Bacterial communities of the coronal sulcus and distal urethra of adolescent males. PloS One 2012, 7, e36298. [Google Scholar] [CrossRef]
- Bandini, M.; Zhu, Y.; Ye, D.-W.; Ornellas, A.A.; Watkin, N.; Ayres, B.; et al. Contemporary treatment patterns and outcomes for patients with penile squamous cell carcinoma: identifying management gaps to promote multi-institutional collaboration. Eur Urol Oncol. 2021, 4, 121–123. [Google Scholar] [CrossRef] [PubMed]
- Necchi, A.; Lo Vullo, S.; Mariani, L.; Zhu, Y.; Ye, D.-W.; Ornellas, A.A.; et al. Nomogram-based prediction of overall survival after regional lymph node dissection and the role of perioperative chemotherapy in penile squamous cell carcinoma: retrospective multicenter study. Urol Oncol. 2019, 37, 531.e7–531.e15. [Google Scholar] [CrossRef]
- Johnstone, P.A.S.; Boulware, D.; Djajadiningrat, R.; Ottenhof, S.; Necchi, A.; Catanzaro, M.; et al. Primary penile cancer: the role of adjuvant radiation therapy in the management of extranodal extension in lymph nodes. Eur Urol Focus. 2019, 5, 737–741. [Google Scholar] [CrossRef] [PubMed]
- Tang, D.H.; Djajadiningrat, R.; Diorio, G.; Chipollini, J.; Ma, Z.; Schaible, B.J.; et al. Adjuvant pelvic radiation is associated with improved survival and decreased disease recurrence in pelvic node-positive penile cancer after lymph node dissection: a multi-institutional study. Urol Oncol. 2017, 35, 605.e17–605.e23. [Google Scholar] [CrossRef] [PubMed]
- Bandini, M.; Ross, J.S.; Zhu, Y.; Ye, D.-W.; Ornellas, A.A.; Watkin, N.; et al. Association between human papillomavirus infection and outcome of perioperative nodal radiotherapy for penile carcinoma. Eur Urol Oncol. 2021, 4, 802–810. [Google Scholar] [CrossRef] [PubMed]
- Thomas, A.; Necchi, A.; Muneer, A.; Tobias-Machado, M.; Tran, A.T.H.; Van Rompuy, A.-S.; et al. Penile cancer. Nat Rev Dis Primers 2021, 7, 11. [Google Scholar] [CrossRef] [PubMed]
- Bandini, M.; Ahmed, M.; Basile, G.; Watkin, N.; Master, V.; Zhu, Y.; et al. A global approach to improving penile cancer care. Nat Rev Urol. 2021, 22, 1–9. [Google Scholar] [CrossRef] [PubMed]
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2022 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.