Urological Involvement in the Multidisciplinary Management of Placenta Accreta Spectrum in a Centralised, High-Volume Centre: A Retrospective Analysis
Abstract
:Introduction
Materials and Methods
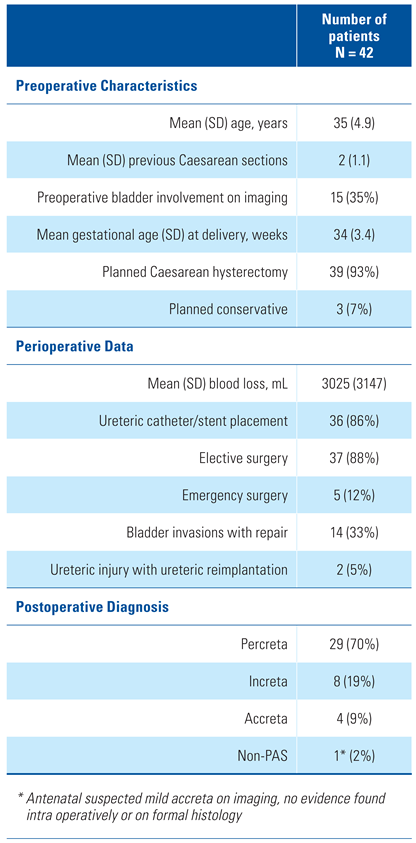
Results
Discussion
Conclusions
Acknowledgments
Conflicts of Interest
References
- Wortman, A.C.; Alexander, J.M. Placenta accreta, increta, and percreta. Obstet. Gynecol. Clin. N. Am. 2013, 40, 137–154. [Google Scholar] [CrossRef] [PubMed]
- Marcellin, L.; Delorme, P.; Bonnet, M.P.; Grange, G.; Kayem, G.; Tsatsaris, V.; et al. Placenta percreta is associated with more frequent severe maternal morbidity than placenta accreta. Am. J. Obstet. Gynecol. 2018, 219, 193.e1–193.e9. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, J.M.; Barton, J.R.; Donaldson, E.S. The management of placenta percreta: Onservative and operative strategies. Am. J. Obstet. Gyneco l.. 1996, 175, 1632–1638. [Google Scholar] [CrossRef] [PubMed]
- Carusi, D.A. The placenta accreta spectrum: Epidemiology and risk factors. Clin. Obstet. Gynecol. 2018, 61, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Bowman, Z.S.; Eller, A.G.; Bardsley, T.R.; Greene, T.; Varner, M.W.; Silver, R.M. Risk factors for placenta accreta: A large prospective cohort. Am. J. Perinatol. 2014, 31, 799–804. [Google Scholar] [CrossRef] [PubMed]
- Eller, A.G.; Porter, T.T.; Soisson, P.; Silver, R.M. Optimal management strategies for placenta accreta. BJOG 2009, 116, 648–654. [Google Scholar] [CrossRef]
- Eller, A.G.; Bennett, M.A.; Sharshiner, M.; Masheter, C.; Soisson, A.P.; Dodson, M.; et al. Maternal morbidity in cases of placenta accreta managed by a multidisciplinary care team compared with standard obstetric care. Obstet. Gynecol. 2011, 117, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Garmi, G.; Salim, R. Epidemiology, etiology, diagnosis, and management of placenta accreta. Obstet. Gynecol. Int. 2012, 2012, 873929. [Google Scholar] [CrossRef] [PubMed]
- Norris, B.L.; Everaerts, W.; Posma, E.; Murphy, D.G.; Umstad, M.P.; Costello, A.J.; et al. The urologist’s role in multidisciplinary management of placenta percreta. BJU Int. 2016, 117, 961–965. [Google Scholar] [CrossRef] [PubMed]
- Ng, M.K.; Jack, G.S.; Bolton, D.M.; Lawrentschuk, N. Placenta percreta with urinary tract involvement: The case for a multidisciplinary approach. Urology 2009, 74, 778–782. [Google Scholar] [CrossRef] [PubMed]
- Vakili, B.; Chesson, R.R.; Kyle, B.L.; Abbas, S.; Echols, K.T.; Gist, R.; et al. The incidence of urinary tract injury during hysterectomy: A prospective analysis based on universal cystoscopy. Am. J. Obstet. Gynecol. 2005, 192, 1599–1604. [Google Scholar] [CrossRef]
- Shamshirsaz, A.A.; Fox, K.A.; Erfani, H.; Belfort, M.A. The role of centers of excellence with multidisciplinary teams in the management of abnormal invasive placenta. Clin. Obstet. Gynecol. 2018, 61, 841–850. [Google Scholar] [CrossRef] [PubMed]
- Shamshirsaz, A.A.; Fox, K.A.; Erfani, H.; Clark, S.L.; Salmanian, B.; Baker, B.W.; et al. Multidisciplinary team learning in the management of the morbidly adherent placenta: Outcome improvements over time. Am. J. Obstet. Gynecol. 2017, 216, 612.e1–612.e5. [Google Scholar] [CrossRef] [PubMed]
- Tam Tam, K.B.; Dozier, J.; Martin, J.N., Jr. Approaches to reduce urinary tract injury during management of placenta accreta, increta, and percreta: A systematic review. J. Matern. Fetal Neonatal Med. 2012, 25, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Merritt, A.J.; Crosbie, E.J.; Charova, J.; Achiampong, J.; Zommere, I.; Winter-Roach, B.; et al. Prophylactic pre-operative bilateral ureteric catheters for major gynaecological surgery. Arch. Gynecol. Obstet. 2013, 288, 1061–1066. [Google Scholar] [CrossRef] [PubMed]
- Warshak, C.R.; Ramos, G.A.; Eskander, R.; Benirskche, K.; Saenz, C.C.; Kelly, T.F.; et al. Effect of predelivery diagnosis in 99 consecutive cases of placenta accreta. Obstet. Gynecol. 2010, 115, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Gielchinsky, Y.; Mankuta, D.; Rojansky, N.; Laufer, N.; Gielchinsky, I.; Ezra, Y. Perinatal outcome of pregnancies complicated by placenta accreta. Obstet. Gynecol. 2004, 104, 527–530. [Google Scholar] [CrossRef] [PubMed]
- Berkley, E.M.; Abuhamad, A.Z. Prenatal diagnosis of placenta accreta: Is sonography all we need? J. Ultrasound Med. 2013, 32, 1345–1350. [Google Scholar] [CrossRef] [PubMed]
- Ballas, J.; Hull, A.D.; Saenz, C.; Warshak, C.R.; Roberts, A.C.; Resnik, R.R.; et al. Preoperative intravascular balloon catheters and surgical outcomes in pregnancies complicated by placenta accreta: A management paradox. Am. J. Obstet. Gynecol. 2012, 207, 216.e1–216.e5. [Google Scholar] [CrossRef] [PubMed]
- Bishop, S.; Butler, K.; Monaghan, S.; Chan, K.; Murphy, G.; Edozien, L. Multiple complications following the use of prophylactic internal iliac artery balloon catheterisation in a patient with placenta percreta. Int. J. Obstet. Anesth. 2011, 20, 70–73. [Google Scholar] [CrossRef]
- Yu, S.C.H.; Cheng, Y.K.Y.; Tse, W.T.; Sahota, D.S.; Chung, M.Y.; Wong, S.S.M.; et al. Perioperative prophylactic internal iliac artery balloon occlusion in the prevention of postpartum hemorrhage in placenta previa: A randomized controlled trial. Am. J. Obstet. Gynecol. 2020, 223, 117.e1–117.e13. [Google Scholar] [CrossRef] [PubMed]
- Robinson, B.K.; Grobman, W.A. Effectiveness of timing strategies for delivery of individuals with placenta previa and accreta. Obstet. Gynecol. 2010, 116, 835–842. [Google Scholar] [CrossRef] [PubMed]
- Balayla, J.; Bondarenko, H.D. Placenta accreta and the risk of adverse maternal and neonatal outcomes. J. Perinat. Med. 2013, 41, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Silver, R.M.; Fox, K.A.; Barton, J.R.; Abuhamad, A.Z.; Simhan, H.; Huls, C.K.; et al. Center of excellence for placenta accreta. Am. J. Obstet. Gynecol. 2015, 212, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Al-Khan, A.; Gupta, V.; Illsley, N.P.; Mannion, C.; Koenig, C.; Bogomol, A.; et al. Maternal and fetal outcomes in placenta accreta after institution of team-managed care. Reprod. Sci. 2014, 21, 761–771. [Google Scholar] [CrossRef] [PubMed]
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2022 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.
Share and Cite
Kelly, B.D.; Moorhead, R.; Wetherell, D.; Gilchrist, T.; Furrer, M.; Perera, M.; Norris, B.; Wrede, D.; Umstad, M.; Kearsley, J.; et al. Urological Involvement in the Multidisciplinary Management of Placenta Accreta Spectrum in a Centralised, High-Volume Centre: A Retrospective Analysis. Soc. Int. Urol. J. 2022, 3, 28-32. https://doi.org/10.48083/OLRA4694
Kelly BD, Moorhead R, Wetherell D, Gilchrist T, Furrer M, Perera M, Norris B, Wrede D, Umstad M, Kearsley J, et al. Urological Involvement in the Multidisciplinary Management of Placenta Accreta Spectrum in a Centralised, High-Volume Centre: A Retrospective Analysis. Société Internationale d’Urologie Journal. 2022; 3(1):28-32. https://doi.org/10.48083/OLRA4694
Chicago/Turabian StyleKelly, Brian D., Rebecca Moorhead, David Wetherell, Tracey Gilchrist, Marcalain Furrer, Marlon Perera, Briony Norris, David Wrede, Mark Umstad, Jamie Kearsley, and et al. 2022. "Urological Involvement in the Multidisciplinary Management of Placenta Accreta Spectrum in a Centralised, High-Volume Centre: A Retrospective Analysis" Société Internationale d’Urologie Journal 3, no. 1: 28-32. https://doi.org/10.48083/OLRA4694
APA StyleKelly, B. D., Moorhead, R., Wetherell, D., Gilchrist, T., Furrer, M., Perera, M., Norris, B., Wrede, D., Umstad, M., Kearsley, J., & Al-Shammaa, F. (2022). Urological Involvement in the Multidisciplinary Management of Placenta Accreta Spectrum in a Centralised, High-Volume Centre: A Retrospective Analysis. Société Internationale d’Urologie Journal, 3(1), 28-32. https://doi.org/10.48083/OLRA4694




