Survival Trend of Tuberculosis Patients and Risk Factors Associated with Mortality and Developing Drug-Resistant Tuberculosis in Hospital Pulau Pinang, Malaysia: A Retrospective Study
Abstract
Highlights
- Higher rate of mortality among drug addict TB patients and an association with abnormal laboratory values.
- Relapsed TB and alcohol consumers are a high-risk population for developing MDR-TB.
- Assist clinicians in identifying high-risk patients prior to or early in the course of TB treatment, which helps improve treatment outcomes.
- Further research is necessary to identify risk factors associated with MDR-TB.
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Diagnosis and Treatment
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Sociodemographic and Clinical Characteristics
3.2. Drug Resistant Patterns of TB Patients
3.3. Treatment Outcomes and Associated Factors of Mortality among TB Patients
3.4. Treatment Outcomes and Associated Factors for Developing Multidrug Resistant TB
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Global Tuberculosis Report. 2020. Available online: https://www.who.int/publications/i/item/9789240013131 (accessed on 15 March 2022).
- World Health Organization (WHO). Global Tuberculosis Report. 2021. Available online: https://www.who.int/publications/i/item/9789240037021 (accessed on 30 March 2022).
- Mohidem, N.A.; Osman, M.; Hashim, Z.; Muharam, F.M.; Elias, S.M.; Shaharudin, R. Association of sociodemographic and environmental factors with spatial distribution of tuberculosis cases in Gombak, Selangor, Malaysia. PLoS ONE 2021, 16, e0252146. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Malaysia (MOH). Clinical Practice Guidelines Management of Tuberculosis (Fourth Edition). Available online: http://www.moh.gov.my (accessed on 15 March 2022).
- World Health Organization (WHO). Malaysia Tuberculosis Country Profile. 2018. Available online: https://www.aidsdatahub.org/sites/default/files/resource/malaysia-tb-country-profile-2018.pdf (accessed on 18 March 2022).
- Minstry of Health Malaysia (MOH). National Strategic Plan. 2016. Available online: https://www.aidsdatahub.org/resource/national-strategic-plan-tuberculosis-2016-2020 (accessed on 18 March 2022).
- Merican, M.I.; Rohaizat, Y.; Haniza, S. Developing the Malaysian health system to meet the challenges of the future. Med. J. Malays. 2004, 59, 84–93. [Google Scholar]
- Ministry of Health Malaysia (MOH). Managment of Drug Resistant Tuberculosis. 2016. Available online: https://www.moh.gov.my/moh/resources/Penerbitan/CPG/Respiratory/CPG%20Management%20of%20Drug%20Resistant%20TB.pdf (accessed on 18 March 2022).
- Iqbal, S.; Ahmed, U.; Khan, M.A. Haematological Parameters Altered in Tuberculosis [Internet]. Pak. J. Physiol. 2015, 11, 13–16. Available online: http://www.pps.org.pk/PJP/11-1/Sumaira.pdf13 (accessed on 18 March 2022).
- Goto, H.; Horita, N.; Tashiro, K.; Nagai, K.; Yamamoto, M.; Sato, T.; Hara, Y.; Nagakura, H.; Shibata, Y.; Watanabe, H.; et al. The platelet count can predict in-hospital death in HIV-negative smear-positive pulmonary tuberculosis inpatients. Intern. Med. 2018, 57, 1391–1397. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.W.; Kim, S.-H.; Lee, S.N.; Lee, S.J.; Lee, M.K.; Lee, J.-H.; Shin, K.C.; Yong, S.J.; Lee, W.-Y. Risk factors related with mortality in patient with pulmonary tuberculosis. Tuberc. Respir. Dis. 2012, 73, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.-L.; Yin, Q.-Y.; Han, C.; Liu, F.-L.; Wang, M.-S. Risk factors for death in tuberculosis patients requiring ICU care. Epidemiol. Infect. 2021, 149, 1–18. [Google Scholar] [CrossRef]
- Rohini, K.; Bhat, M.S.; Srikumar, P.S.; Kumar, A.M. Assessment of Hematological Parameters in Pulmonary Tuberculosis Patients. Indian J. Clin. Biochem. 2016, 31, 332–335. [Google Scholar] [CrossRef]
- Ismail, I.; Bulgiba, A. Predictors of Death during Tuberculosis Treatment in TB/HIV Co-Infected Patients in Malaysia. PLoS ONE 2013, 8, e73250. [Google Scholar] [CrossRef]
- Kruger, S.; Ewig, S.; Marre, R.; Papassotiriou, J.; Richter, K.; von Baum, H.; Suttorp, N.; Welte, T.; CAPNETZ Study Group. Procalcitonin predicts patients at low risk of death from community-acquired pneumonia across all CRB-65 classes. Eur. Respir. J. 2008, 31, 349–355. [Google Scholar] [CrossRef]
- Gounden, V.; Bhatt, H.; Jialal, I. Renal Function Tests; StatPearls Publishing: Treasure Island, FL, USA, 2018. Available online: https://www.ncbi.nlm.nih.gov/books/NBK507821/#!po=97.2222 (accessed on 22 November 2021).
- Devarbhavi, H.; Singh, R.; Patil, M.; Sheth, K.; Adarsh, C.K.; Balaraju, G. Outcome and determinants of mortality in 269 patients with combination anti-tuberculosis drug-induced liver injury. J. Gastroenterol. Hepatol. 2013, 28, 161–167. [Google Scholar] [CrossRef]
- Dominguez De Villota, E.; Mosquera, J.M.; Rubio, J.J.; Galdos, P.; Diez Balda, V.; de la Serna, J.L.; Tomas, M.I. Intensive Care Medicine Association of a Low Serum Albumin with Infection and Increased Mortality in Critically Ill Patients. Intensive Care Med. 1980, 7, 19–22. [Google Scholar] [CrossRef] [PubMed]
- Rothschild, M.A.; Oratz, M.; Schreiber, S.S. Special Articles Serum Albumin. Hepatology. 1988. Available online: https://aasldpubs.onlinelibrary.wiley.com/doi/abs/10.1002/hep.1840080234 (accessed on 20 November 2021).
- Alavi, S.M.; Salami, N. The Causes and Risk Factors of Tuberculosis Deaths in Khuzestan. Acta Med. Iran 2009, 47, 89–92. [Google Scholar]
- Saeed, A.M.; Raafat, R.H.; Elbaz, E.M. Study of addiction in newly diagnosed patients with pulmonary tuberculosis in Abbasia Chest Hospital. Egypt. J. Bronchol. 2018, 12, 105–113. [Google Scholar]
- Alavi-Naini, R.; Moghtaderi, A.; Metanat, M.; Mohammadi, M.; Zabetian, M. Factors associated with mortality in tuberculosis patients. J. Res. Med. Sci. 2013, 18, 52–55. [Google Scholar] [PubMed]
- Chan, C.K.; Wong, K.H.; Lee, M.P.; Chan, K.C.; Leung, C.C.; Leung, E.C.; Mak, I.K. Risk factors associated with 1-year mortality among patients with HIV-associated tuberculosis in areas with intermediate tuberculosis burden and low HIV prevalence. Hong Kong Med. J. 2018, 24, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Kourbatova, E.V.; Borodulin, B.E.; Borodulina, E.A.; Del Rio, C.; Blumberg, H.M.; Leonard, M.K., Jr. Risk factors for mortality among adult patients with newly diagnosed tuberculosis in Samara, Russia. Int. J. Tuberc. Lung Dis. 2006, 10, 1224–1230. [Google Scholar] [PubMed]
- Deiss, R.G.; Rodwell, T.C.; Garfein, R.S. Tuberculosis and illicit drug use: Review and update. Clin. Infect. Dis. 2009, 48, 72–82. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Integrating Collaborative TB and HIV Services within a Comprehensive Package of Care for People who Inject Drugs. 2016. Available online: www.who.int (accessed on 20 November 2021).
- Dooley, K.E.; Lahlou, O.; Knudsen, J.; Elmessaoudi, M.D.; Cherkaoui, I.; El Aouad, R. Risk factors for tuberculosis treatment failure, default, or relapse and outcomes of retreatment in Morocco. BMC Public Health 2011, 11, 140. [Google Scholar] [CrossRef]
- Boonsarngsuk, V.; Tansirichaiya, K.; Kiatboonsri, S. Thai drug-resistant tuberculosis predictive scores. Singap. Med. J. 2009, 50, 378–384. [Google Scholar]
- Elmi, O.S.; Hasan, H.; Abdullah, S.; Jeab, M.Z.M.; Ba, Z.; Naing, N.N. Treatment outcomes of patients with multidrug-resistant tuberculosis (MDR-TB) compared with non-MDR-TB infections in peninsular Malaysia. Malays. J. Med. Sci. 2016, 23, 17–25. [Google Scholar] [CrossRef]
- Mekonnen, F.; Tessema, B.; Moges, F.; Gelaw, A.; Eshetie, S.; Kumera, G. Multidrug resistant tuberculosis: Prevalence and risk factors in districts of metema and west armachiho, Northwest Ethiopia. BMC Infect. Dis. 2015, 15, 461. [Google Scholar] [CrossRef] [PubMed]
- Saldanha, N.; Runwal, K.; Ghanekar, C.; Gaikwad, S.; Sane, S.; Pujari, S. High prevalence of multi drug resistant tuberculosis in people living with HIV in Western India. BMC Infect. Dis. 2019, 19, 391. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.H.; Sulaiman, S.A.S.; Laghari, M.; Hassali, M.A.; Muttalif, A.R.; Bhatti, Z.; Ming, L.C.; Talpur, B.A. Treatment outcomes and risk factors of extra-pulmonary tuberculosis in patients with co-morbidities. BMC Infect. Dis. 2019, 19, 691. [Google Scholar] [CrossRef] [PubMed]
- Laghari, M.; Sulaiman, S.A.S.; Khan, A.H.; Memon, N. Epidemiology of tuberculosis and treatment outcomes among children in Pakistan: A 5 year retrospective study. PeerJ 2018, 2018, e5253. [Google Scholar] [CrossRef]
- Sosa, A.d.J.; Byarugaba, D.K.; Amabile-Cuevas, C.F.; Hsueh, P.-R.; Kariuki, S.; Okeke, I.N. Antimicrobial Resistance in Developing Countries; Springer: New York, NY, USA, 2010. [Google Scholar]
- Shariff, N.M.; Shah, S.A.; Kamaludin, F. Previous treatment, sputum-smear nonconversion, and suburban living: The risk factors of multidrug-resistant tuberculosis among Malaysians. Int. J. Mycobacteriol. 2016, 5, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Tekkel, M.; Rahu, M.; Loit, H.M.; Baburin, A. Risk factors for pulmonary tuberculosis in Estonia. Int. J. Tuberc. Lung Dis. 2002, 6, 887–894. [Google Scholar]
- Yang, L.; Wu, D.-L.; Guo, H.-G.; Liu, J.-W. A study of the psychological and social factors in patients with pulmonary tuberculosis. Chin. J. Tuberc. Respir. Dis. 2003, 26, 704–707. [Google Scholar]
- Song, W.M.; Liu, J.Y.; Fu, Q.; Xu, T.T.; Li, S.J.; Tao, N.N.; Li, H.C. The Impact of Alcohol Drinking and Tobacco Smoking On The Drug-Resistance of Newly Diagnosed Tuberculosis. Respir. Med. 2021, 12, e059149. [Google Scholar]
- Zetola, N.M.; Modongo, C.; Kip, E.C.; Gross, R.; Bisson, G.P.; Collman, R.G. Alcohol use and abuse among patients with multidrug-resistant tuberculosis in Botswana. Int. J. Tuberc. Lung Dis. 2012, 16, 1529–1534. [Google Scholar] [CrossRef]
- Workie, M.G.; Aycheh, M.W.; Birhanu, M.Y.; Tsegaye, T.B. Treatment interruption among drug-susceptible pulmonary tuberculosis patients in southern ethiopia. Patient Prefer. Adherence 2021, 15, 1143–1151. [Google Scholar] [CrossRef]
- Akkaif, M.A.; Bitar, A.N.; Al-Kaif, L.A.; Daud, N.A.A.; Sha’aban, A.; Noor, D.A.M.; Ibrahim, B. The Management of Myocardial Injury Related to SARS-CoV-2 Pneumonia. J. Cardiovasc. Dev. Dis. 2022, 9, 307. [Google Scholar] [CrossRef] [PubMed]
- Akkaif, M.A.; Sha’aban, A.; Cesaro, A.; Jaber, A.A.S.; Vergara, A.; Yunusa, I.; Ibrahim, B. The impact of SARS-CoV-2 treatment on the cardiovascular system: An updated review. Inflammopharmacology 2022, 30, 1143–1151. [Google Scholar] [CrossRef] [PubMed]



| Drug | Daily Dose (mg/day) |
|---|---|
| 1 Akurit 2 | 2–5 tab/day |
| 2 Akurit 4 | 2–5 tab/day |
| Pyridoxine | 10–50 |
| Isoniazid | 150–300 |
| Rifampicin | 300–600 |
| Ethambutol | 400–1600 |
| Pyrazinamide | 250–2000 |
| Streptomycin | 500–1000 |
| Levofloxacin | 250–1000 |
| Ethionamide | 250–500 |
| Kanamycin | 500–1000 |
| Moxifloxacin | 400–800 |
| Clofazimine | 100–200 |
| Cycloserine | 250 |
| Meropenem | 1000 |
| Augmentin | 1200 |
| Bedaquiline | 200 |
| Linezolid | 600 |
| Ofloxacin | 40 |
| Clarithromycin | 500 |
| Outcome | Definition |
|---|---|
| Cured | A pulmonary TB patient with bacteriologically confirmed TB at the beginning of treatment who was smear- or culture-negative in the last month of treatment and on at least one previous occasion. |
| Treatment completed | A TB patient who completed treatment without evidence of failure BUT with no record to show that sputum smear or culture results in the last month of treatment and on at least one previous occasion were negative, either because tests were not done or because results are unavailable. |
| Died | A TB patient who dies for any reason before starting or during the course of treatment. |
| Treatment failed | A TB patient whose sputum smear or culture is positive at month 5 or later during treatment. |
| Lost to follow up | A TB patient who did not start treatment or whose treatment was interrupted for 2 consecutive months or more. |
| Not evaluated | A TB patient for whom no treatment outcome is assigned. This includes cases “transferred out” to another treatment unit, as well as cases for whom the treatment outcome is unknown to the reporting unit. |
| Treatment success | The sum of cured and treatment completed. |
| Variable | Median (IQR) | No. (%) | |
|---|---|---|---|
| Gender | Female | - | 90 (25.6) |
| Male | 261 (74.4) | ||
| Age (years) | 18–24 | 51.0 (74.0) | 56 (15.9) |
| >24–34 | 48 (13.7) | ||
| >34–44 | 54 (15.4) | ||
| >44–54 | 60 (17.1) | ||
| >54–64 | 73 (20.8) | ||
| ≥64 | 60 (17.1) | ||
| Race | Malay | - | 126 (35.9) |
| Chinese | 163 (46.4) | ||
| Indian | 45 (12.8) | ||
| * Other | 17 (4.8) | ||
| Marital status | Married | - | 226 (64.4) |
| Single | 125 (35.6) | ||
| Smoking Habbit | Non-smokers | - | 189 (53.8) |
| Smokers | 162 (46.2) | ||
| Alcohol consumption | No | - | 302 (86.0) |
| Yes | 49 (14.0) | ||
| Drug addiction | No | - | 292 (83.2) |
| Yes | 59 (16.8) | ||
| Imprisoned | No | - | 335 (95.4) |
| Yes | 16 (4.6) | ||
| Diabetes mellitus | Non-diabetics | - | 260 (74.1) |
| Diabetics | 91 (25.9) | ||
| Human immunodeficiency virus | Non-reactive | - | 310 (88.3) |
| Reactive | 41 (11.7) | ||
| Hepatitis B virus | Non-reactive | - | 338 (96.3) |
| Reactive | 13 (3.7) | ||
| Hepatitis C virus | Non-reactive | - | 323 (92.0) |
| Reactive | 28 (8.0) | ||
| Case category | New | - | 253 (72.1) |
| Relapse | 98 (27.9) | ||
| History of TB | No history | - | 256 (72.9) |
| History | 95 (27.1) | ||
| Variable | No. (%) | |
|---|---|---|
| DST for isoniazid | INH susceptible | 100 (28.5) |
| INH resistant | 10 (2.8) | |
| Not applicable | 241 (68.7) | |
| DST for rifampicin | RIF susceptible | 96 (27.4) |
| RIF resistant | 14 (4.0) | |
| Not applicable | 241 (68.7) | |
| DST for ethambutol | ETH susceptible | 105 (29.9) |
| ETH resistant | 3 (0.9) | |
| Not applicable | 243 (69.2) | |
| DST for streptomycin | STM susceptible | 103 (29.3) |
| STM resistant | 6 (1.7) | |
| Not applicable | 242 (68.9) | |
| DST for pyrazinamide | PZA susceptible | 6 (1.7) |
| PZA resistant | 3 (0.9) | |
| Not applicable | 342 (97.4) | |
| Outcomes | Drug-Susceptible TB (N = 325) | MDR-TB (N = 26) |
|---|---|---|
| Death | 73 (22.5%) | 5 (19.2%) |
| Cure | 171 (52.6%) | - |
| Treatment completed | 74 (22.8) | 21 (80.8%) |
| Treatment failure | 1 (0.3%) | - |
| Loss of follow up/default treatment | 6 (1.8%) | - |
| Variable | Chi-Square | df | Sig. (Log-Rank) | |
|---|---|---|---|---|
| Gender | Female Male | 2.050 | 1 | 0.152 |
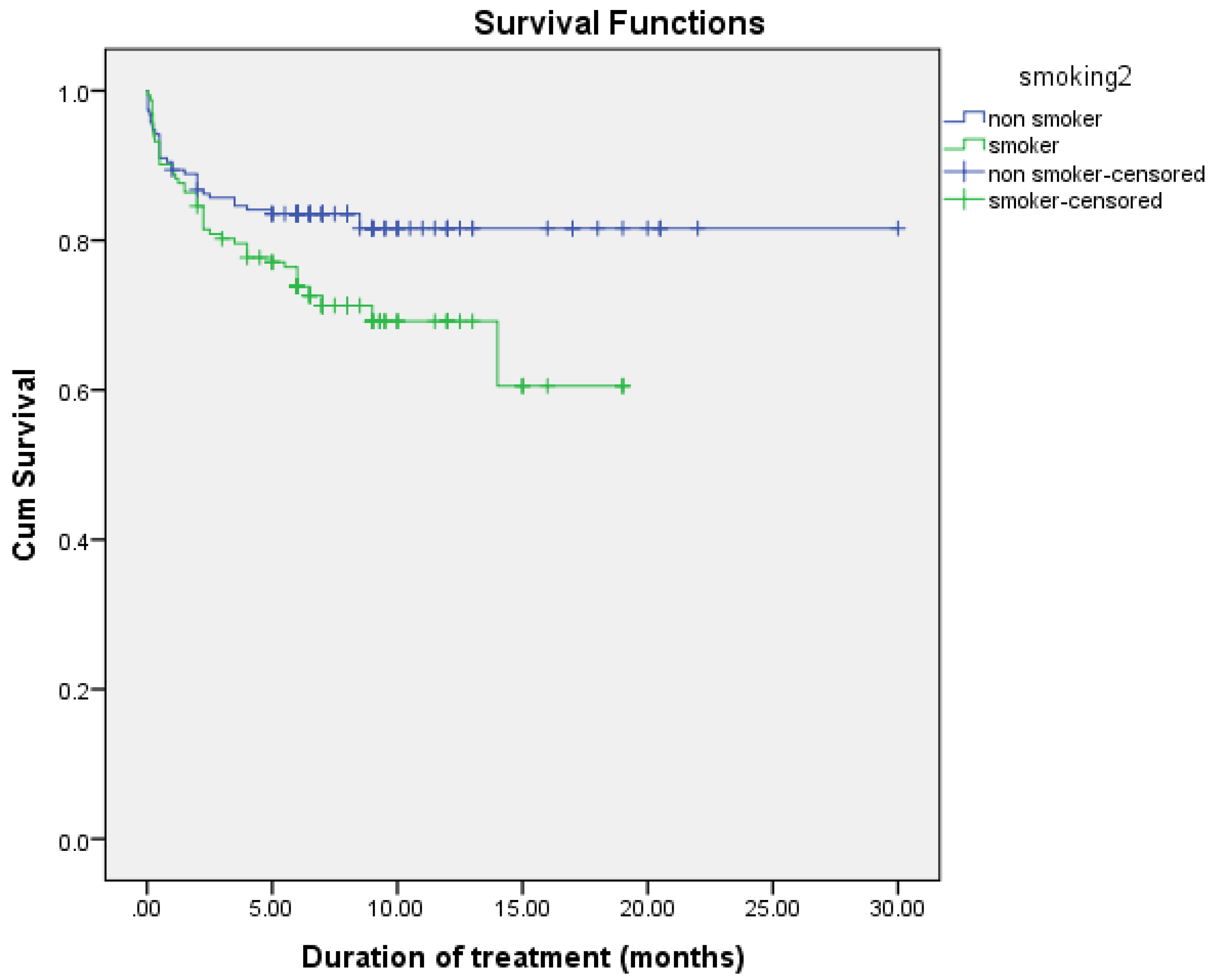
| Smoking habit | Non-smokers Smokers | 5.743 | 1 | 0.017 |
| Alcohol consumption | Non-drinkers Drinkers | 0.404 | 1 | 0.525 |
| Drug addiction | Non-drug addicts Drug addicts | 4.450 | 1 | 0.035 |
| History of TB | History No history | 0.093 | 1 | 0.760 |
| Diabetes mellitus | Diabetics Non-diabetics | 1.365 | 1 | 0.243 |
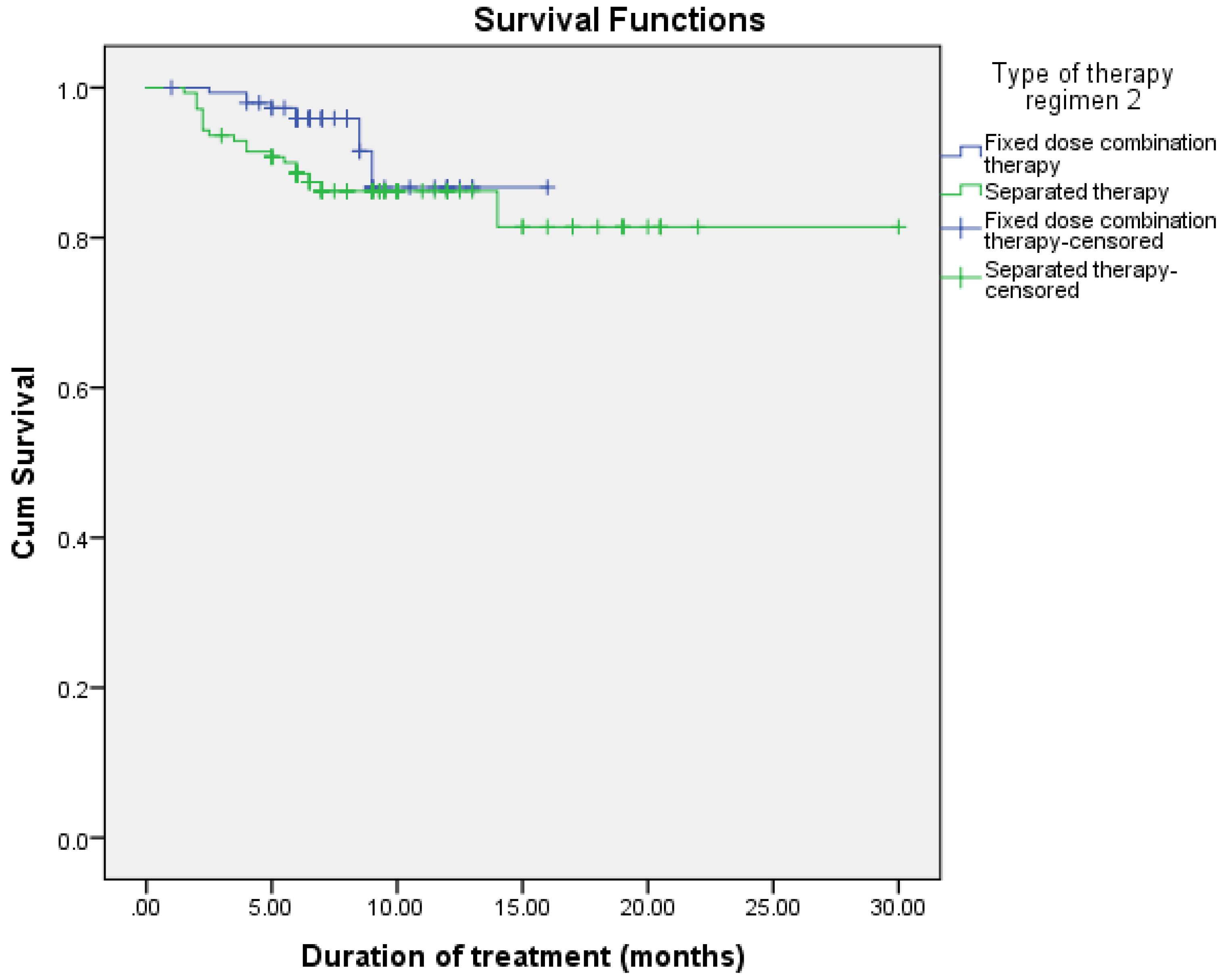
| Intensive phase regimen | Fixed-dose combination Separated therapy | 3.892 | 1 | 0.049 |
| Maintenance phase regimen | Fixed-dose combination Separated therapy | 3.834 | 1 | 0.000 |
| Variable | Treatment Outcome | Hazard Ratio (95% CI) | p-Value | ||
|---|---|---|---|---|---|
| Alive, N (%) | Died, N (%) | ||||
| Gender | Female Male | 70 (27.8) 182 (72.2) | 15 (20.5) 58 (79.5) | Referent 1.511 (0.844–2.705) | 0.165 |
| Smoking habit | Non-smokers Smokers | 151 (59.9) 101 (40.1) | 32 (43.8) 41 (56.2) | Referent 1.723 (1.081–2.746) | 0.022 |
| Alcohol consumption | Non-drinkers Drinkers | 224 (88.9) 28 (11.1) | 65 (89.0) 8 (11.0) | Referent 1.289 (0.708–2.349) | 0.407 |
| Drug addiction | Non-drug addicts Drug addicts | 216 (85.7) 36 (14.3) | 54 (74.0) 19 (26.0) | Referent 1.652 (0.960–2.843) | 0.050 |
| History of TB | History No history | 54 (21.4) 198 (78.6) | 23 (31.5) 50 (68.5) | Referent 0.960 (0.576–1.599) | 0.875 |
| Diabetes mellitus | Diabetics Non-diabetics | 68 (27.0) 184 (73.0) | 17 (23.3) 56 (76.7) | Referent 1.363 (0.783–2.373) | 0.274 |
| Intensive phase regimen | Fixed-dose combination Separated therapy | 204 (81.0) 48 (19.0) | 47 (66.2) 24 (33.8) | Referent 1.571 (0.976–2.5280) | 0.063 |
| Maintenance phase regimen | Fixed-dose combination Separated therapy | 141 (56.0) 102 (40.5) | 8 (11.0) 15 (20.5) | Referent 2.130 (0.914–4.963) | 0.080 |
| White blood cells, median (IQR) | 8.7 (30.6) | 1.071 (1.026–1.118) | 0.002 | ||
| Haemoglobin | 11.9 (13.1) | 0.809 (0.736–0.890) | 0.000 | ||
| Platelets | 309.0 (977.0) | 0.997 (0.996–0.999) | 0.000 | ||
| Neutrophils % | 71.5 (132.9) | 1.017 (1.006–1.029) | 0.003 | ||
| Lymphocytes % | 17.3 (80.7) | 0.943 (0.919–0.968) | 0.000 | ||
| Albumin | 28.0 (34.3) | 0.957 (0.939–0.976) | 0.000 | ||
| ALT | 18.0 (796.0) | 1.002 (0.999–1.006) | 0.157 | ||
| Urea | 3.9 (78.7) | 1.034 (1.020–1.048) | 0.000 | ||
| Creatinine | 72.0 (1322) | 1.001 (1.000–1.003) | 0.008 | ||
| Variable | HR (95% CI) | p-Value |
|---|---|---|
| Drug addiction | 1.836 (1.019–3.309) | 0.034 |
| White blood cells | 1.102 (1.057–1.148) | 0.000 |
| Platelets | 0.996 (0.995–0.998) | 0.000 |
| Albumin | 0.964 (0.940–0.990) | 0.006 |
| Urea | 1.029 (1.011–1.047) | 0.002 |
| Variable | Multi-Drug Resistant TB | Hazard Ratio (95% CI) | p-Value | ||
|---|---|---|---|---|---|
| Yes (N = 26) | No | ||||
| Gender | Female Male | 5 (19.2) 21 (80.8) | 85 (26.2) 240 (73.8) | Referent 2.024 (0.743–5.512) | 0.168 |
| Race | Malay Non-Malay | 4 (15.4) 22 (84.6) | 121 (37.2) 204 (62.8) | Referent 2.067 (0.692–6.174) | 0.193 |
| Marital status | Married Single | 9 (34.6) 17 (65.4) | 217 (66.8) 108 (33.2) | Referent 4.547 (1.960–10.548) | 0.000 |
| Smoking | Non-smokers Smokers | 6 (23.1) 20 (76.9) | 183 (56.3) 142 (43.7) | Referent 0.088 (0.026–0.301) | 0.000 |
| Drinking | Non-drinkers Drinkers | 13 (50.0) 13 (50.0) | 289 (88.9) 36 (11.1) | Referent 7.452 (3.206–17.324) | 0.000 |
| Drug addiction | Non-drug addicts Drug addicts | 22 (84.6) 4 (15.4) | 270 (83.1) 55 (16.9) | Referent 1.454 (0.491–4.305) | 0.499 |
| Imprisoned | Prisoners Non-Prisoners | 3 (11.5) 23 (88.5) | 13 (4.0) 312 (96.0) | Referent 0.270 (0.075–0.978) | 0.046 |
| History of TB | History No history | 18 (69.2) 8 (30.8) | 77 (23.7) 248 (76.3) | Referent 0.400 (0.168–0.952) | 0.038 |
| Case category | New Relapse | 5 (19.2) 21 (80.8) | 248 (76.3) 77 (23.7) | Referent 3.649 (1.306–10.196) | 0.014 |
| MTB culture at baseline | Growth No growth | 6 (5.0) 6 (50.0) | 8 (12.3) 57 (87.7) | Referent 0.300 (0.093–0.971) | 0.044 |
| Intensive phase regimen | Fixed-dose combination Separated therapy | 3 (12.0) 22 (88.0) | 269 (82.8) 56 (17.2) | Referent 0.101 (0.029–0.355) | 0.000 |
| Variable | HR (95% CI) | p-Value |
|---|---|---|
| Relapse TB | 3.035 (1.028–8.957) | 0.044 |
| Alcohol consumption | 7.591 (3.097–18.610) | 0.000 |
| Being single | 6.817 (2.599–17.879) | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yaghi, A.R.; Shaheed, H.S.; Harun, S.N.; Hyder Ali, I.A.; Khan, A.H. Survival Trend of Tuberculosis Patients and Risk Factors Associated with Mortality and Developing Drug-Resistant Tuberculosis in Hospital Pulau Pinang, Malaysia: A Retrospective Study. Adv. Respir. Med. 2022, 90, 467-482. https://doi.org/10.3390/arm90060054
Yaghi AR, Shaheed HS, Harun SN, Hyder Ali IA, Khan AH. Survival Trend of Tuberculosis Patients and Risk Factors Associated with Mortality and Developing Drug-Resistant Tuberculosis in Hospital Pulau Pinang, Malaysia: A Retrospective Study. Advances in Respiratory Medicine. 2022; 90(6):467-482. https://doi.org/10.3390/arm90060054
Chicago/Turabian StyleYaghi, Aseel Rezeq, Heba Saleh Shaheed, Sabariah Noor Harun, Irfhan Ali Hyder Ali, and Amer Hayat Khan. 2022. "Survival Trend of Tuberculosis Patients and Risk Factors Associated with Mortality and Developing Drug-Resistant Tuberculosis in Hospital Pulau Pinang, Malaysia: A Retrospective Study" Advances in Respiratory Medicine 90, no. 6: 467-482. https://doi.org/10.3390/arm90060054
APA StyleYaghi, A. R., Shaheed, H. S., Harun, S. N., Hyder Ali, I. A., & Khan, A. H. (2022). Survival Trend of Tuberculosis Patients and Risk Factors Associated with Mortality and Developing Drug-Resistant Tuberculosis in Hospital Pulau Pinang, Malaysia: A Retrospective Study. Advances in Respiratory Medicine, 90(6), 467-482. https://doi.org/10.3390/arm90060054







