The Swiss Sleep House Bern—A New Approach to Sleep Medicine
Abstract
1. Unmet Needs of Sleep Medicine
1.1. The Central Role of Sleep for Health, Well-Being, Creativity, and Productivity Is Underestimated
1.2. Sleep Loss and Sleep–Wake Circadian Disorders in the General Population Are Highly Prevalent but Underdiagnosed and Undertreated despite Their High Impact on Health, Well-Being, Creativity, and Productivity
1.3. Education in Sleep Medicine and Health Care-Related Sleep Research Are Underdeveloped
1.4. The Implementation of Emerging New Technologies to Monitor Sleep and Sleep–Wake Circadian Disorders Is Insufficient
1.5. Reimbursement of Sleep Medicine Is Inadequate and Specialized Care Is Limited to a Few Centers
2. The Swiss Sleep House Bern (SSHB): A New Approach to Address the Unmet Needs of Sleep Medicine
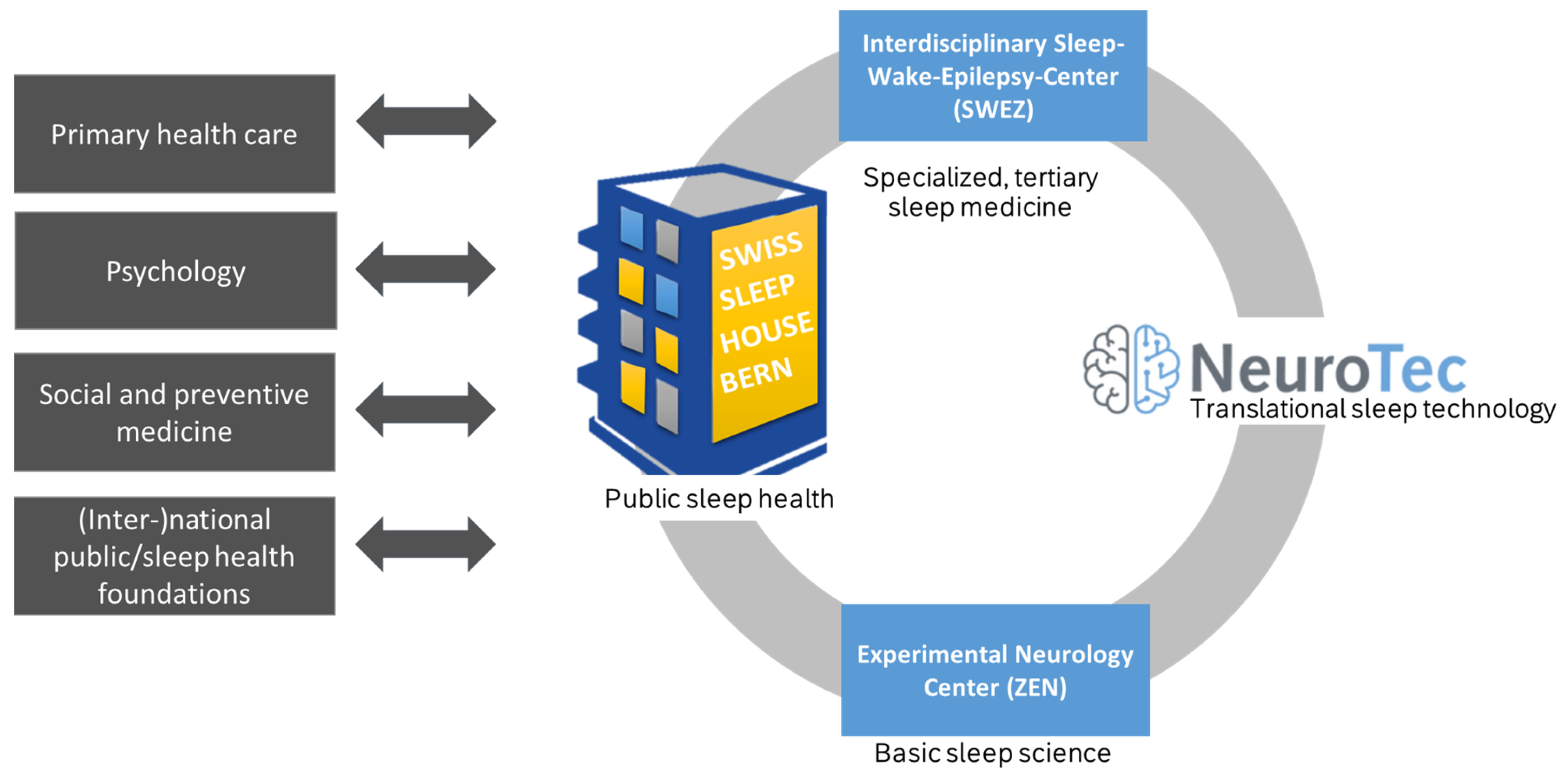
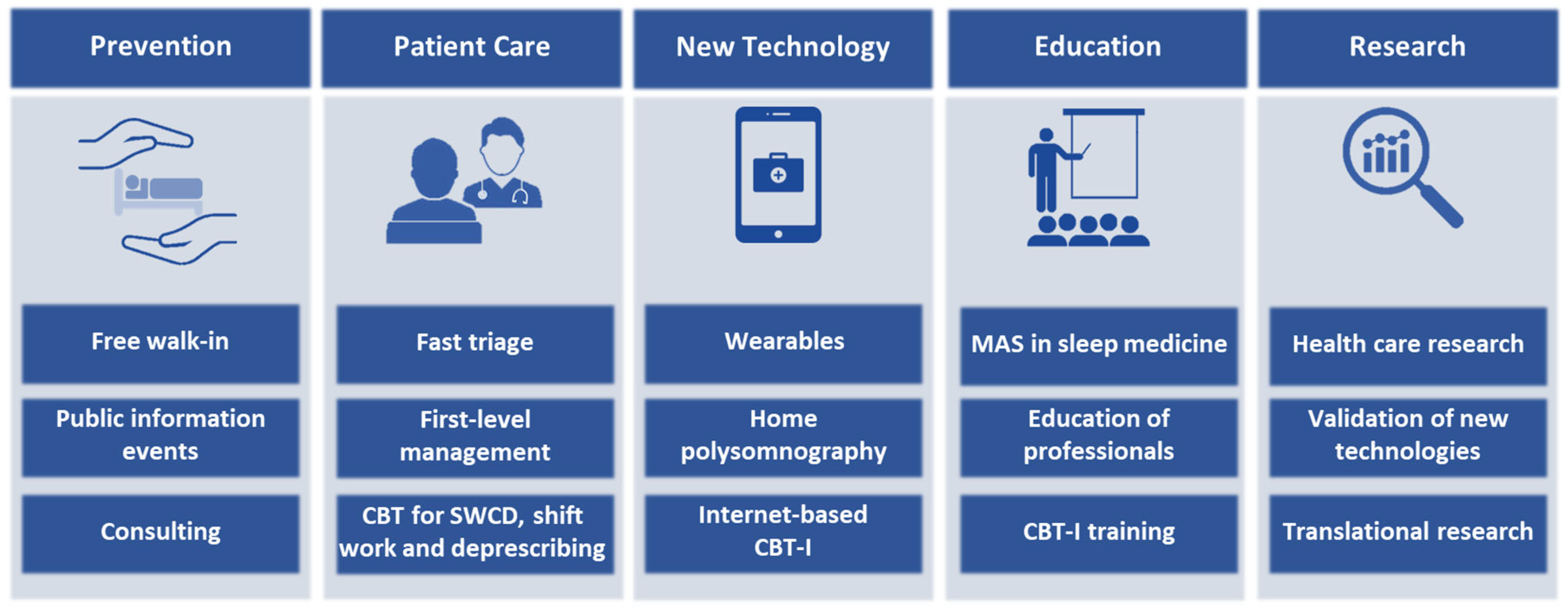
2.1. Structure and Organization of Swiss Sleep House Bern (SSHB)
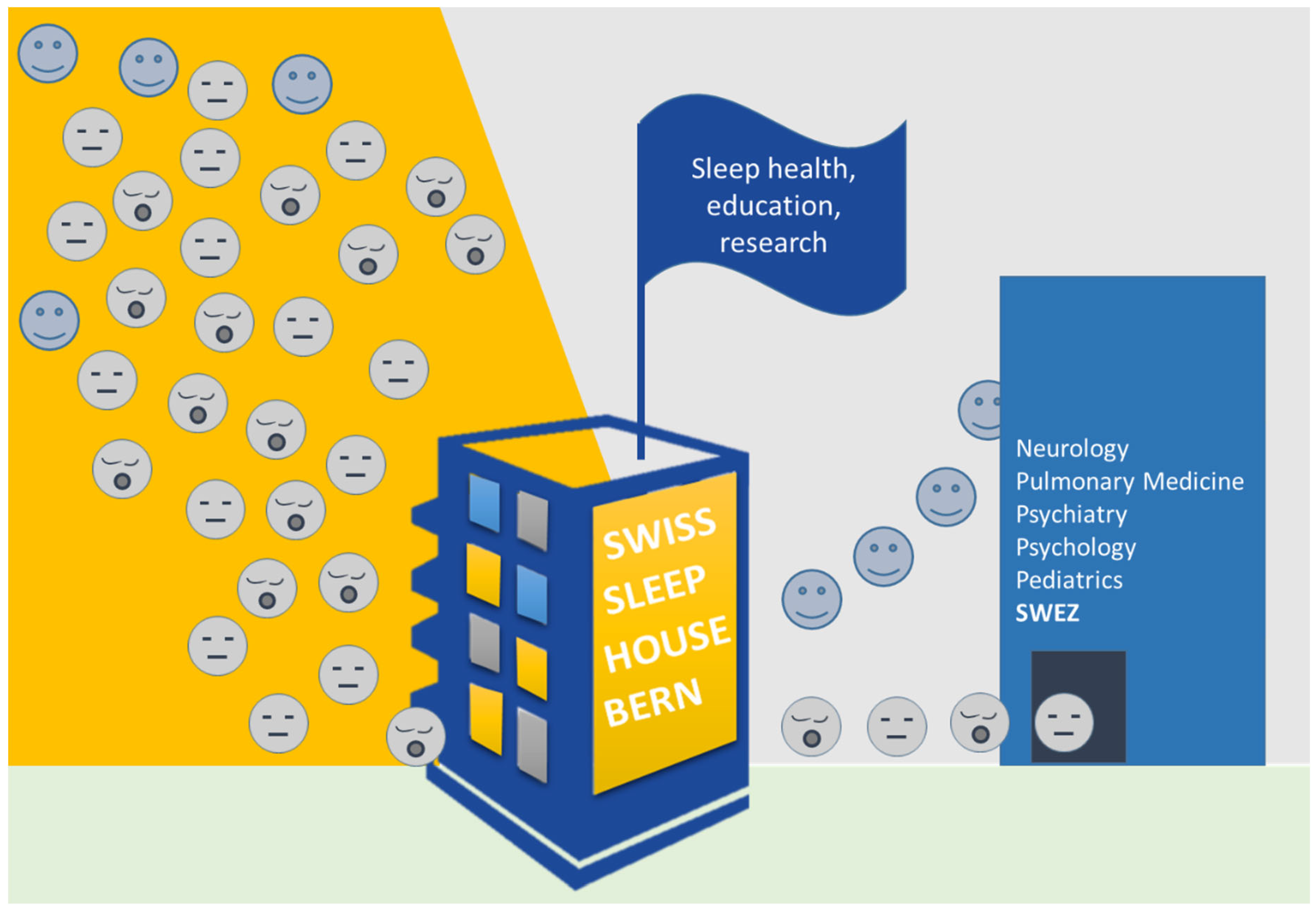
2.2. Promotion of Sleep Health and Prevention of Sleep Loss in Sleep–Wake Circadian Disorders
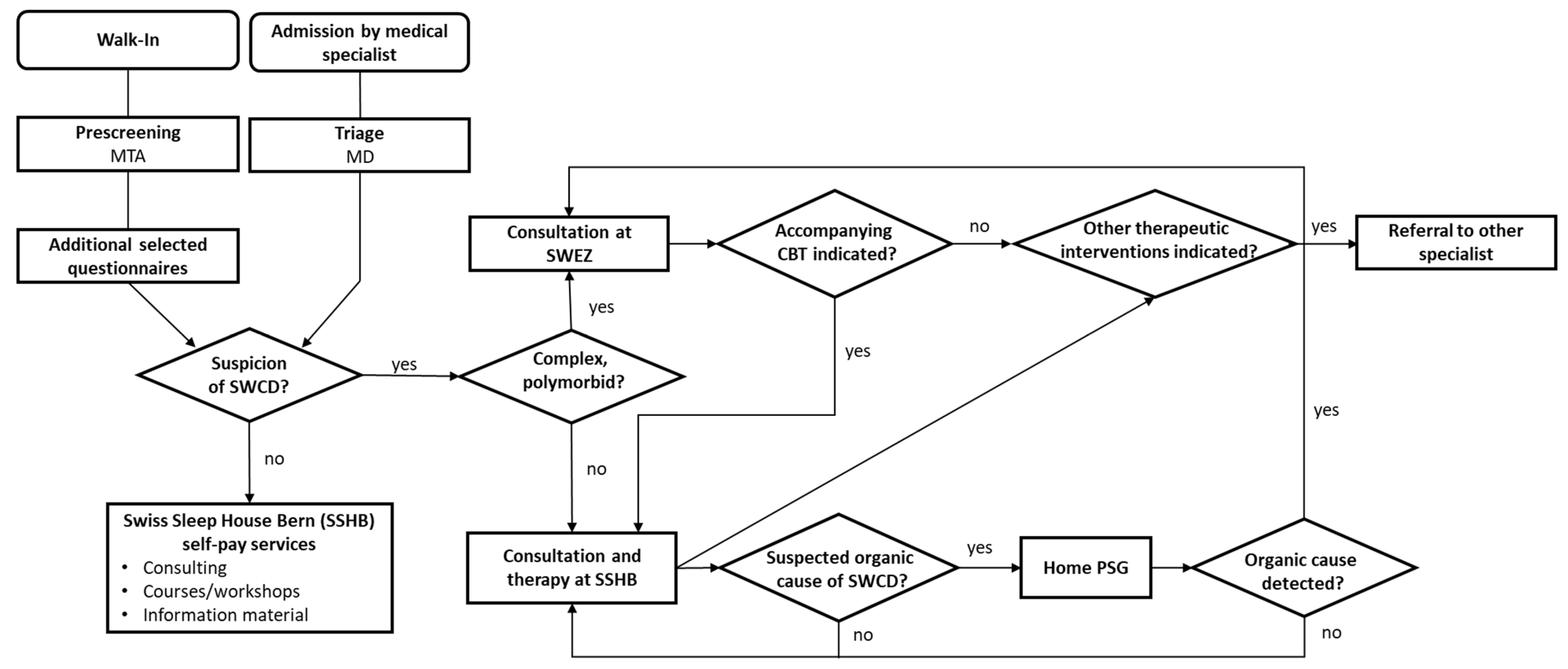
2.3. Lowering the Burden of Undiagnosed and Insufficiently Treated Sleep–Wake Circadian Disorders
2.4. Application of Novel Technologies, Telemedicine, and Data Science in Sleep Medicine
2.5. Education of Health Care Professionals
2.6. Interdisciplinary Health Care Sleep Research
3. Concluding Remarks
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Buysse, D.J. Sleep health: Can we define it? Does it matter? Sleep 2014, 37, 9–17. [Google Scholar] [CrossRef]
- Vorster, A.P.A.; van Someren, E.; Pack, A.; Huber, R.; Schmidt, M.H.; Bassetti, C.L.A. Sleep Health. Clin. Transl. Neurosci. 2024, 8, 8. [Google Scholar] [CrossRef]
- Bassetti, C.L.A.; Heldner, M.R.; Adorjan, K.; Albanese, E.; Allali, G.; Arnold, M.; Bègue, I.; Bochud, M.; Chan, A.; do Cuénod, K.Q.; et al. The Swiss Brain Health Plan 2023–2033. Clin. Transl. Neurosci. 2023, 7, 38. [Google Scholar] [CrossRef]
- Lim, D.C.; Najafi, A.; Afifi, L.; Bassetti, C.L.A.; Buysse, D.J.; Han, F.; Högl, B.; Melaku, Y.A.; Morin, C.M.; Pack, A.I.; et al. The need to promote sleep health in public health agendas across the globe. Lancet Public Health 2023, 8, e820–e826. [Google Scholar] [CrossRef] [PubMed]
- Brodt, S.; Inostroza, M.; Niethard, N.; Born, J. Sleep—A brain-state serving systems memory consolidation. Neuron 2023, 111, 1050–1075. [Google Scholar] [CrossRef] [PubMed]
- Gorgoni, M.; D’Atri, A.; Lauri, G.; Rossini, P.M.; Ferlazzo, F.; De Gennaro, L. Is sleep essential for neural plasticity in humans, and how does it affect motor and cognitive recovery? Neural Plast. 2013, 2013, 103949. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Lai, C.S.; Cichon, J.; Ma, L.; Li, W.; Gan, W.B. Sleep promotes branch-specific formation of dendritic spines after learning. Science 2014, 344, 1173–1178. [Google Scholar] [CrossRef] [PubMed]
- Xie, L.; Kang, H.; Xu, Q.; Chen, M.J.; Liao, Y.; Thiyagarajan, M.; O’Donnell, J.; Christensen, D.J.; Nicholson, C.; Iliff, J.J.; et al. Sleep drives metabolite clearance from the adult brain. Science 2013, 342, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Fultz, N.E.; Bonmassar, G.; Setsompop, K.; Stickgold, R.A.; Rosen, B.R.; Polimeni, J.R.; Lewis, L.D. Coupled electrophysiological, hemodynamic, and cerebrospinal fluid oscillations in human sleep. Science 2019, 366, 628–631. [Google Scholar] [CrossRef] [PubMed]
- Wennberg, A.M.V.; Wu, M.N.; Rosenberg, P.B.; Spira, A.P. Sleep Disturbance, Cognitive Decline, and Dementia: A Review. Semin. Neurol. 2017, 37, 395–406. [Google Scholar] [CrossRef]
- Bassetti, C.L.A.; Randerath, W.; Vignatelli, L.; Ferini-Strambi, L.; Brill, A.; Bonsignore, M.R.; Grote, L.; Jennum, P.; Leys, D.; Minnerup, J.; et al. EAN/ERS/ESO/ESRS statement on the impact of sleep disorders on risk and outcome of stroke. Eur. J. Neurol. 2020, 27, 1117–1136. [Google Scholar] [CrossRef]
- Scott, A.J.; Webb, T.L.; Martyn-St James, M.; Rowse, G.; Weich, S. Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep Med. Rev. 2021, 60, 101556. [Google Scholar] [CrossRef]
- Fan, M.; Sun, D.; Zhou, T.; Heianza, Y.; Lv, J.; Li, L.; Qi, L. Sleep patterns, genetic susceptibility, and incident cardiovascular disease: A prospective study of 385,292 UK biobank participants. Eur. Heart J. 2020, 41, 1182–1189. [Google Scholar] [CrossRef]
- Li, X.; Xue, Q.; Wang, M.; Zhou, T.; Ma, H.; Heianza, Y.; Qi, L. Adherence to a Healthy Sleep Pattern and Incident Heart Failure: A Prospective Study of 408,802 UK Biobank Participants. Circulation 2021, 143, 97–99. [Google Scholar] [CrossRef] [PubMed]
- Fietze, I.; Rosenblum, L.; Salanitro, M.; Ibatov, A.D.; Eliseeva, M.V.; Penzel, T.; Brand, D.; Westermayer, G. The Interplay Between Poor Sleep and Work-Related Health. Front. Public Health 2022, 10, 866750. [Google Scholar] [CrossRef] [PubMed]
- Amiri, S.; Behnezhad, S. Sleep disturbances and risk of sick leave: Systematic review and meta-analysis. Sleep Biol. Rhythm. 2020, 18, 283–295. [Google Scholar] [CrossRef]
- Wu, Q.J.; Sun, H.; Wen, Z.Y.; Zhang, M.; Wang, H.-Y.; He, X.-H.; Jiang, Y.-T.; Zhao, Y.-H. Shift work and health outcomes: An umbrella review of systematic reviews and meta-analyses of epidemiological studies. J. Clin. Sleep Med. 2022, 18, 653–662. [Google Scholar] [CrossRef]
- Beattie, L.; Kyle, S.D.; Espie, C.A.; Biello, S.M. Social interactions, emotion and sleep: A systematic review and research agenda. Sleep Med. Rev. 2015, 24, 83–100. [Google Scholar] [CrossRef] [PubMed]
- Kerkhof, G.A. Epidemiology of sleep and sleep disorders in The Netherlands. Sleep Med. 2017, 30, 229–239. [Google Scholar] [CrossRef]
- Ohayon, M.M. Epidemiological Overview of sleep Disorders in the General Population. Sleep Med. Res. 2011, 2, 1–9. [Google Scholar] [CrossRef]
- Bundesamt für Statistik. Gesundheitsstatistik 2019; Bundesamt für Statistik (BFS): Neuchâtel, Switzerland, 2019. [Google Scholar]
- Kocevska, D.; Lysen, T.S.; Dotinga, A.; Koopman-Verhoeff, M.E.; Luijk, M.P.C.M.; Antypa, N.; Biermasz, N.R.; Blokstra, A.; Brug, J.; Burk, W.J.; et al. Sleep characteristics across the lifespan in 1.1 million people from the Netherlands, United Kingdom and United States: A systematic review and meta-analysis. Nat. Hum. Behav. 2021, 5, 113–122. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Sleep Medicine (Ed.) International Classification of Sleep Disorders, 3rd ed.; American Academy of Sleep Medicine: Darien, IL, USA, 2014. [Google Scholar]
- Dennis, J.A.; Alazzeh, A.; Kumfer, A.M.; McDonald-Thomas, R.; Peiris, A.N. The Association of Unreported Sleep Disturbances and Systemic Inflammation: Findings from the 2005–2008 NHANES. Sleep Disord. 2018, 2018, 5987064. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.M. Epidemiology of insomnia: What we know and what we still need to learn. Sleep Med. Rev. 2002, 6, 97–111. [Google Scholar] [CrossRef] [PubMed]
- Maire, M.; Linder, S.; Dvorak, C.; Merlo, C.; Essig, S.; Tal, K.; Del Giovane, C.; Syrogiannouli, L.; Duss, S.B.; Heinzer, R.; et al. Prevalence and management of chronic insomnia in Swiss primary care: Cross-sectional data from the “Sentinella” practice-based research network. J. Sleep Res. 2020, 29, e13121. [Google Scholar] [CrossRef] [PubMed]
- Riemann, D.; Espie, C.A.; Altena, E.; Arnardottir, E.S.; Baglioni, C.; Bassetti, C.L.A.; Bastien, C.; Berzina, N.; Bjorvatn, B.; Dikeos, D.; et al. The European Insomnia Guideline: An update on the diagnosis and treatment of insomnia 2023. J. Sleep Res. 2023, 32, e14035. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.M.; O’Hara, R.; Vitiello, M.V. Epidemiology of restless legs syndrome: A synthesis of the literature. Sleep Med. Rev. 2012, 16, 283–295. [Google Scholar] [CrossRef] [PubMed]
- Arnardottir, E.S.; Bjornsdottir, E.; Olafsdottir, K.A.; Benediktsdottir, B.; Gislason, T. Obstructive sleep apnoea in the general population: Highly prevalent but minimal symptoms. Eur. Respir. J. 2016, 47, 194–202. [Google Scholar] [CrossRef]
- Bauters, F.; Debuyzere, M.; Chirinos, J.; Hertegonne, K.; Rietzschel, E. The prevalence of sleep-disordered breathing in the general population: Results of the Asklepios Cohort. Eur. Respir. J. 2018, 52 (Suppl. S62), PA4357. [Google Scholar] [CrossRef]
- Lettieri, C.J.; Williams, S.G.; Collen, J.F.; Wickwire, E.M. Treatment of Obstructive Sleep Apnea: Achieving Adherence to Positive Airway Pressure Treatment and Dealing with Complications. Sleep Med. Clin. 2020, 15, 227–240. [Google Scholar] [CrossRef]
- Schoch, O.D.; Baty, F.; Niedermann, J.; Rudiger, J.J.; Brutsche, M.H. Baseline predictors of adherence to positive airway pressure therapy for sleep apnea: A 10-year single-center observational cohort study. Respir. Int. Rev. Thorac. Dis. 2014, 87, 121–128. [Google Scholar] [CrossRef]
- Perez-Carbonell, L.; Mignot, E.; Leschziner, G.; Dauvilliers, Y. Understanding and approaching excessive daytime sleepiness. Lancet 2022, 400, 1033–1046. [Google Scholar] [CrossRef]
- Moradi, A.; Nazari, S.S.H.; Rahmani, K. Sleepiness and the risk of road traffic accidents: A systematic review and meta-analysis of previous studies. Transp. Res. Part F Traffic Psychol. Behav. 2019, 65, 620–629. [Google Scholar] [CrossRef]
- Blachier, M.; Dauvilliers, Y.; Jaussent, I.; Helmer, C.; Ritchie, K.; Jouven, X.; Tzourio, C.; Amouyel, P.; Besset, A.; Ducimetiere, P.; et al. Excessive daytime sleepiness and vascular events: The Three City Study. Ann. Neurol. 2012, 71, 661–667. [Google Scholar] [CrossRef] [PubMed]
- Jaussent, I.; Bouyer, J.; Ancelin, M.L.; Berr, C.; Foubert-Samier, A.; Ritchie, K.; Ohayon, M.M.; Besset, A.; Dauvilliers, Y. Excessive sleepiness is predictive of cognitive decline in the elderly. Sleep 2012, 35, 1201–1207. [Google Scholar] [CrossRef] [PubMed]
- Holding, B.C.; Sundelin, T.; Schiller, H.; Akerstedt, T.; Kecklund, G.; Axelsson, J. Sleepiness, sleep duration, and human social activity: An investigation into bidirectionality using longitudinal time-use data. Proc. Natl. Acad. Sci. USA 2020, 117, 21209–21217. [Google Scholar] [CrossRef]
- Bassetti, C.L.M. Sleep and Neurology Stroke. 1. Overview. In Sleep Medicine Textbook, 2nd ed.; Bassetti, C., McNicholas, W., Paunio, T., Peigneux, P., Eds.; European Sleep Research Society (ESRS): Regensburg, Germany, 2021. [Google Scholar]
- Shen, Y.; Lv, Q.-K.; Xie, W.-Y.; Gong, S.-Y.; Zhuang, S.; Liu, J.-Y.; Mao, C.-J.; Liu, C.-F. Circadian disruption and sleep disorders in neurodegeneration. Transl. Neurodegener. 2023, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- Steele, T.A.; St Louis, E.K.; Videnovic, A.; Auger, R.R. Circadian Rhythm Sleep-Wake Disorders: A Contemporary Review of Neurobiology, Treatment, and Dysregulation in Neurodegenerative Disease. Neurotherapeutics 2021, 18, 53–74. [Google Scholar] [CrossRef]
- Voysey, Z.J.; Barker, R.A.; Lazar, A.S. The Treatment of Sleep Dysfunction in Neurodegenerative Disorders. Neurotherapeutics 2021, 18, 202–216. [Google Scholar] [CrossRef]
- Gustavsson, A.; Svensson, M.; Jacobi, F.; Allgulander, C.; Alonso, J.; Beghi, E.; Dodel, R.; Ekman, M.; Faravelli, C.; Fratiglioni, L.; et al. Cost of disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol. 2011, 21, 718–779. [Google Scholar] [CrossRef] [PubMed]
- Watson, N.F. Health Care Savings: The Economic Value of Diagnostic and Therapeutic Care for Obstructive Sleep Apnea. J. Clin. Sleep Med. 2016, 12, 1075–1077. [Google Scholar] [CrossRef]
- American Academy of Sleep Medicine (Ed.) Hidden Health Crisis Costing America Billions. Underdiagnosing and Undertreating Obstructive Sleep Apnea. Draining Healthcare System; American Academy of Sleep Medicine: Darien, IL, USA, 2016. [Google Scholar]
- Tinguely, G.; Landolt, H.P.; Cajochen, C. Schlafgewohnheiten, Schlafqualität und Schlafmittelkonsum der Schweizer Bevölkerung–Ergebnisse aus einer neuen Umfrage bei einer repräsentativen Stichprobe. Therapeutische Umschau 2014, 71, 637–646. [Google Scholar] [CrossRef]
- Bundesamt für Statistik. Schichtarbeitende in der Schweiz 2002–2022; Bundesamt für Statistik (BFS): Neuchâtel, Switzerland, 2024. [Google Scholar]
- Mindell, J.A.; Bartle, A.; Wahab, N.A.; Ahn, Y.; Ramamurthy, M.B.; Huong, H.T.D.; Kohyama, J.; Ruangdaraganon, N.; Sekartini, R.; Teng, A.; et al. Sleep education in medical school curriculum: A glimpse across countries. Sleep Med. 2011, 12, 928–931. [Google Scholar] [CrossRef] [PubMed]
- Romiszewski, S.; May, F.E.K.; Homan, E.J.; Norris, B.; Miller, M.A.; Zeman, A. Medical student education in sleep and its disorders is still meagre 20 years on: A cross-sectional survey of UK undergraduate medical education. J. Sleep Res. 2020, 29, e12980. [Google Scholar] [CrossRef]
- Quan, S.F. Graduate medical education in sleep medicine: Did the canary just die? J. Clin. Sleep Med. 2013, 9, 101. [Google Scholar] [CrossRef]
- Ramar, K.; Malhotra, R.K.; Carden, K.A.; Martin, J.L.; Abbasi-Feinberg, F.; Aurora, R.N.; Kapur, V.K.; Olson, E.J.; Rosen, C.L.; Rowley, J.A.; et al. Sleep is essential to health: An American Academy of Sleep Medicine position statement. J. Clin. Sleep Med. 2021, 17, 2115–2119. [Google Scholar] [CrossRef] [PubMed]
- Sorscher, A.J. How is your sleep: A neglected topic for health care screening. J. Am. Board Fam. Med. 2008, 21, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Gnarra, O.; Wulf, M.A.; Schäfer, C.; Nef, T.; Bassetti, C.L.A. Rapid eye movement sleep behavior disorder: A narrative review from a technological perspective. Sleep 2023, 46, zsad030. [Google Scholar] [CrossRef] [PubMed]
- Dietmann, A.; Wenz, E.; van der Meer, J.; Ringli, M.; Warncke, J.D.; Edwards, E.; Schmidt, M.H.; Bernasconi, C.A.; Nirkko, A.; Strub, M.; et al. The Swiss Primary Hypersomnolence and Narcolepsy Cohort study (SPHYNCS): Study protocol for a prospective, multicentre cohort observational study. J. Sleep Res. 2021, 30, e13296. [Google Scholar] [CrossRef] [PubMed]
- Zhu, G.; Catt, M.; Cassidy, S.; Birch-Machin, M.; Trenell, M.; Hiden, H.; Woodman, S.; Anderson, K.N. Objective sleep assessment in >80,000 UK mid-life adults: Associations with sociodemographic characteristics, physical activity and caffeine. PLoS ONE 2019, 14, e0226220. [Google Scholar] [CrossRef]
- Wainberg, M.; Jones, S.E.; Beaupre, L.M.; Hill, S.L.; Felsky, D.; Rivas, M.A.; Lim, A.S.P.; Ollila, H.M.; Tripathy, S.J. Association of accelerometer-derived sleep measures with lifetime psychiatric diagnoses: A cross-sectional study of 89,205 participants from the UK Biobank. PLoS Med. 2021, 18, e1003782. [Google Scholar] [CrossRef]
- Yuan, H.; Plekhanova, T.; Walmsley, R.; Reynolds, A.; Maddison, K.; Bucan, M.; Gehrman, P.; Rowlands, A.; Ray, D.; Bennett, D.; et al. Self-supervised learning of accelerometer data provides new insights for sleep and its association with mortality. medRxiv 2023. [Google Scholar] [CrossRef]
- Gjerstad, D.M.; Puertas, J.; Goncalves, M.; Mihaicuta, S.; Dogas, Z.; Grote, L. Reimbursement of Sleep Procedures across Europe. Executive Committee, Assembly of National Sleep Societies, European Sleep Research Society. 2019. Available online: https://esrs.eu/wp-content/uploads/2019/01/Reimbursement_of_Sleep_Procedures_across_Europe_latest_version_june2014.pdf (accessed on 5 March 2024).
- Chiao, W.; Durr, M.L. Trends in sleep studies performed for Medicare beneficiaries. Laryngoscope 2017, 127, 2891–2896. [Google Scholar] [CrossRef]
- Fietze, I.; Laharnar, N.; Bargiotas, P.; Basoglu, O.K.; Dogas, Z.; Drummond, M.; Fanfulla, F.; Gislason, T.; Gouveris, H.; Grote, L.; et al. Management of obstructive sleep apnea in Europe—A 10-year follow-up. Sleep Med. 2022, 97, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Schindler, K.A.; Nef, T.; Baud, M.O.; Tzovara, A.; Yilmaz, G.; Tinkhauser, G.; Gerber, S.M.; Gnarra, O.; Warncke, J.D.; Schütz, N.; et al. NeuroTec Sitem-Insel Bern: Closing the Last Mile in Neurology. Clin. Transl. Neurosci. 2021, 5, 13. [Google Scholar] [CrossRef]
- Cronlein, T.; Geisler, P.; Langguth, B.; Eichhammer, P.; Jara, C.; Pieh, C.; Zulley, J.; Hajak, G. Polysomnography reveals unexpectedly high rates of organic sleep disorders in patients with prediagnosed primary insomnia. Sleep Breath. Schlaf Atm. 2012, 16, 1097–1103. [Google Scholar] [CrossRef] [PubMed]
- Luta, X.; Bagnoud, C.; Lambiris, M.; Decollogny, A.; Eggli, Y.; Le Pogam, M.-A.; Marques-Vidal, P.; Marti, J. Patterns of benzodiazepine prescription among older adults in Switzerland: A cross-sectional analysis of claims data. BMJ Open 2020, 10, e031156. [Google Scholar] [CrossRef] [PubMed]
- Schmid, D.; Duss, S.B.; Hertenstein, E.; Nissen, C.; Schneider, C.L.; Urech, A.; Vorster, A.; Berger, T. SLEEPexpert+: Blending Internet-Based Cognitive Behavioral Therapy for Insomnia with In-Person Psychotherapy; A Feasibility Study in Routine Care. Clin. Transl. Neurosci. 2023, 7, 27. [Google Scholar] [CrossRef]
- Duss, S.B.; Bauer-Gambelli, S.A.; Bernasconi, C.; Dekkers, M.P.; Gorban-Peric, C.; Kuen, D.; Seiler, A.; Oberholzer, M.; Alexiev, F.; Lippert, J.; et al. Frequency and evolution of sleep-wake disturbances after ischemic stroke: A 2-year prospective study of 437 patients. Sleep Med. 2022, 101, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Duss, S.B.; Bernasconi, C.; Steck, A.; Brill, A.; Manconi, M.; Dekkers, M.; Schmidt, M.H.; Bassetti, C.L.A. Multiple sleep-wake disturbances after stroke predict an increased risk of cardio-cerebrovascular events or death: A prospective cohort study. Eur. J. Neurol. 2023, 30, 1696–1705. [Google Scholar] [CrossRef]
- Tüzün, M.; Kallweit, U.; Seidel, S.; Endrich, O.; Trelle, S.; Leone, M.A.; Bruni, O.; Dodel, R.; Fiorillo, A.; Holmerová, I.; et al. The Burden of Insomnia and Excessive Daytime Sleepiness: Switzerland’s pilot study preliminary results. In Proceedings of the ePoster Session at the 10th EAN Congress, Helsinki, Finland, 29 June–2 July 2024. [Google Scholar]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duss, S.B.; Vorster, A.P.A.; Urech, A.; Schmitt, W.J.; Beck, J.; Hilt, D.; Gnarra, O.; van der Meer, J.; Tüzün, M.; Berger, T.; et al. The Swiss Sleep House Bern—A New Approach to Sleep Medicine. Clin. Transl. Neurosci. 2024, 8, 14. https://doi.org/10.3390/ctn8010014
Duss SB, Vorster APA, Urech A, Schmitt WJ, Beck J, Hilt D, Gnarra O, van der Meer J, Tüzün M, Berger T, et al. The Swiss Sleep House Bern—A New Approach to Sleep Medicine. Clinical and Translational Neuroscience. 2024; 8(1):14. https://doi.org/10.3390/ctn8010014
Chicago/Turabian StyleDuss, Simone B., Albrecht P. A. Vorster, Antoine Urech, Wolfgang J. Schmitt, Jonas Beck, Daniella Hilt, Oriella Gnarra, Julia van der Meer, Marina Tüzün, Thomas Berger, and et al. 2024. "The Swiss Sleep House Bern—A New Approach to Sleep Medicine" Clinical and Translational Neuroscience 8, no. 1: 14. https://doi.org/10.3390/ctn8010014
APA StyleDuss, S. B., Vorster, A. P. A., Urech, A., Schmitt, W. J., Beck, J., Hilt, D., Gnarra, O., van der Meer, J., Tüzün, M., Berger, T., Schäfer, C., Brill, A.-K., Schmidt, M. H., Schindler, K. A., & Bassetti, C. L. A. (2024). The Swiss Sleep House Bern—A New Approach to Sleep Medicine. Clinical and Translational Neuroscience, 8(1), 14. https://doi.org/10.3390/ctn8010014







