Abstract
Chronic insomnia (insomnia disorder—ID) afflicts up to 10% of the adult population, increases with age and affects more women than men. ID is associated with significant daytime impairments and an increased risk for developing major somatic and mental disorders, especially depression and anxiety disorders. Almost all insomnia models assume persistent hyperarousal on cognitive, emotional, cortical and physiological levels as a central pathophysiological component. The marked discrepancy between only minor objective alterations in polysomnographic parameters of sleep continuity and the profound subjective impairment in patients with insomnia is still puzzling. We and others have proposed that alterations in the microstructure of sleep, especially in REM sleep (REM sleep instability), may explain this discrepancy and be at the core of the experience of fragmented and poor sleep in ID. The REM sleep instability concept is based on evidence showing REM time to be related to subjective wake time in insomnia as well as increased micro- and macro-arousals during REM sleep in insomnia patients compared to good-sleeper controls. Our own work showed that ID patients awoken from REM sleep more frequently reported the perception of having been awake than good sleepers as well as having had more negative ideations. The continuous measurement of event-related potentials throughout the whole night demonstrated reduced P2 amplitudes specifically during phasic REM sleep in insomnia, which points to a mismatch negativity in ID reflecting automatic change detection in the auditory system and a concomitant orienting response. REM sleep represents the most highly aroused brain state during sleep and thus might be particularly prone to fragmentation in individuals with persistent hyperarousal, resulting in a more conscious-like wake experience reflecting pre-sleep concerns of patients with ID, i.e., worries about poor sleep and its consequences, thus leading to the subjective over-estimation of nocturnal waking time and the experience of disrupted and non-restorative sleep. Chronic REM sleep instability might also lead to a dysfunction in a ventral emotional neural network, including limbic and paralimbic areas activated during REM sleep. Along with a postulated weakened functioning in a dorsal executive neural network, including frontal and prefrontal areas, this might contribute to emotional and cognitive alterations and an elevated risk of developing depression and anxiety.
1. Introduction
Aetiological and pathophysiological ideas, hypotheses, concepts and theories about insomnia (as a diagnosis: insomnia disorder = ID) in adults have been suggested not just recently, but may have a longer history. The concept of “hyperarousal” has a long-standing history in the academic work on insomnia. This article will provide an overview of current thoughts and theories of insomnia in general and its underlying origins. In doing so, we will draw extensively on both our own recent work and that of others [1,2,3,4,5,6,7,8,9,10], so that certain similarities and overlap to this are not entirely avoidable. We will then link the hyperarousal concept with a more specific hypothesis, “REM sleep instability”, which ascribes a central role to the phenomenon of fragmented REM sleep concerning the pathophysiology of ID [9,11,12,13,14].
2. Aetiological and Pathophysiological Aspects of Insomnia
Recent literature on insomnia has specified behavioural, neurobiological and cognitive–emotional insomnia models in detail, thus emphasizing the close relationship between insomnia and psychopathology (for a summary, see Figure 1) [1,2,3,4,5,6,7,8,9,10].
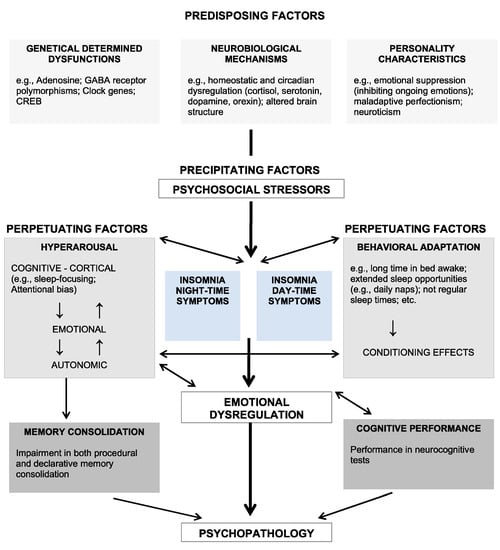
Figure 1.
Comprehensive insomnia model (see text; taken from Riemann et al. [5]).
The basic structure of the model shown in Figure 1 is adopted from the so-called 3P model of insomnia that was formulated by Spielman and colleagues [15]. The 3 P’s stand for Predisposing, Precipitating and Perpetuating factors. This model has been very influential for the insomnia field, as it constitutes an ideal basis for the different areas relevant for insomnia theories. Our line of argumentation will closely follow the structure outlined in this model.
2.1. Predisposing Factors
A wide range of relevant biological and psychological predisposing factors for ID have been identified. Biological factors include neurobiological mechanisms of sleep regulation as well as growing knowledge in the field of (epi-)genetics. Psychological factors refer to well-researched premorbid characteristics regarding cognition, emotion regulation and personality.
2.1.1. Genetics
Family and twin studies confirm that genetic and epigenetic factors play a role in the aetiology of insomnia [16,17]. GWAS (genome-wide association studies) indicate a marked polygenicity involving more than 500 genes [18]. Common heritable factors were documented for insomnia and restless legs (e.g., BTB domain containing 9 (BTBD9) and protein tyrosine phosphatase receptor type D (PTPRD) genes), certain psychiatric traits related to mood regulation (e.g., glycogen synthase kinase-3β (GSK3B) gene) and metabolic dysfunction [17,18,19,20]. These studies indicated that vulnerability/predisposition to insomnia does not stem directly from circuits playing a role in sleep regulation. Rather, brain tissues (e.g., anterior cingulate cortex) and cell types expressing risk genes for insomnia seem to be mainly part of circuitries being involved in the regulation of emotion [9].
2.1.2. Neurobiologically Relevant Sleep Mechanisms
A review on the neurobiology of insomnia needs to encompass major neuroanatomic and neurophysiological mechanisms of sleep regulation, especially with regard to well-described homeostatic and biological time-keeping factors [21]. From a sleep–neurobiological perspective, insomnia can be associated with an imbalance between mechanisms governing wakefulness and arousal, and sleep-inducing mechanisms.
The flip-flop switch model of sleep–wake regulation [22] postulates regular mutual inhibitory processes between wake and sleep promoting neuronal cell groups. Activation of one cell group firstly inhibits the other, and after a certain time, inhibits its own activation, allowing switches between sleeping and waking. Wakefulness involves a network of hypothalamic cell groups (including orexinergic neurons in the lateral hypothalamus [23]), the brainstem and the basal forebrain. These activate the thalamus and cerebral cortex structures, which include cell groups of the ARAS (ascending reticular activating system). During sleep, the VLPO (ventrolateral preoptic nucleus) is disinhibited and blocks wake/arousal-promoting neurons in the hypothalamus and brainstem through GABA (gamma-amino-butyric acid). The VLPO obtains afferent input from the main monoaminergic systems (including cell groups in the raphe nuclei and locus coeruleus, containing dopamine) and is inhibited by norepinephrine and serotonin. In addition, GABAergic neurons in the ventrolateral periaqueductal gray region are thought to play an important role in gating REM sleep [24].
From this perspective, a relative increased activity in the wake-promoting system, a decrease in the sleep system’s activity or a combination of both factors simultaneously could be at the core of insomnia [23].
2.1.3. Sleep Reactivity, Emotion and Personality
Psychological factors that are involved in both sleep regulation and predisposition to insomnia arise from the areas of emotion and personality. Although this is sometimes neglected, it is widely known that sleep initiation is hampered with any sort of internal/external threat. Numerous observations indicate that these factors play a central role in the predisposition to insomnia [9]. For example, empirical work points to sleep reactivity [25,26], i.e., the premorbid tendency to experience disrupted sleep as a reaction to stressful life events, as a significant risk factor for insomnia. A range of other traits, often closely associated with the regulation of emotions, seem to be linked with insomnia. Perfectionism, neuroticism, a stable tendency to internalize problems as well as an increased sensitivity to anxiety symptoms have to be mentioned here [27,28]. These characteristics could be coupled with heightened baseline levels of arousal and/or the increased tendency to respond to relevant stressors with signs of (hyper-) arousal. In this vein, perfectionism might increase arousal when faced with a night of insomnia by promoting the subjective perception of a personal failure not being able to sleep [28].
3. Precipitating Factors
In everyday life, acute bouts of insomnia are usually triggered with relevant stressors like significant life events. This type of event is often coupled with negative emotional valence and relates to a threat of security to family, health or the areas of work, school or other aspects of living. Precipitating factors may include environmental factors such as heat or noise, either in the form of a single significant event or an accumulation of many minor stressors, or in a prolonged form as chronic stressors [29]. Needless to say, not everyone reacting with insomnia to acute stressors will develop chronic insomnia. Probably in the majority of cases, the insomnia disappears after the stressor has passed or has successfully been coped with. Possessing certain predisposing traits, however, will lead more easily to the emergence and establishing of vicious psychoneurobiological circles that pave the path to the chronification of insomnia symptoms. The increase in hypothalamic–pituitary–adrenal (HPA) axis activity due to acute stress can directly impair sleep [30], while this stress response may be solidified with personality and emotional factors and maladaptive behaviours like prolonged bedtimes and frequent clock-watching (see Perpetuating Factors).
4. Perpetuating Factors
4.1. Cognitive Factors
Cognitive factors play an important role in the perpetuation of insomnia [31,32], including dysfunctional and/or incorrect beliefs about sleep requirements and consequences of not being able to sleep, as well as meta-cognitive beliefs about the process of worrying itself and/or appropriate ways to cope with it [33,34], including dysfunctional regulation of the ensuing emotions [35]. This often leads to excessive worrying, negative expectations and negative emotional tone during the pre-sleep period. This is associated with sleep disturbances, the extent of which in turn seems to depend on the content of cognitive activity. In this regard, it has been demonstrated that only sleep-related cognitive activity (e.g., “When I sleep poorly on one night I know that it will interfere with my work performance on the next day.” [36]) but not general cognitive arousal is associated with polysomnographically determined sleep disturbances [37].
It has been suggested that, possibly as a result of negative expectations and emotions, selective attentional processes further reinforce dysfunctional cognitions in insomnia. The attentional system of patients with insomnia was found to be especially sensitive to sleep-related stimuli (attentional bias) [38]. Such attentional bias may provoke an increased sleep effort that interferes with the automaticity of sleep, and further reinforces the experience of insomnia [31].
4.2. Behavioural Factors
To make up for their perceived sleep loss, a majority of insomnia patients tend to adopt dysfunctional behaviours. Bedtimes will be prolonged, more daytime napping will take place and alcohol consumption might be increased to facilitate sleep. In general, sleep–wake schedules will become more irregular. Nevertheless, any of these self-help strategies are dysfunctional as they perpetuate insomnia symptoms by reducing sleep pressure and/or further weakening the conditioned association between the bed environment and sleep (see the classical work by Bootzin [39]).
4.3. Hyperarousal
The above-mentioned factors are intertwined with the pathophysiological concept of hyperarousal (HYA). HYA manifests as increased levels of arousal in physiological, cognitive/emotional and cortical arousal domains. HYA is considered a stable trait characteristic of individuals prone to developing insomnia, as well as a pathophysiologically central state following disease onset, occurring throughout the entire 24-h cycle [2,4,5,6,7] and not just during the night. Nevertheless, HYA is a broad and heterogeneous construct, and it is likely that patients suffering from insomnia exhibit different HYA foci, with some being physiologically highly aroused and others showing more intense cognitive/cortical arousal [7,40,41]. Furthermore, arousal levels are unlikely to be constant throughout the day. For example, conditioned arousal responses in the bedtime environment [8] and sleep effort [31] could lead to particularly high levels of arousal before bedtime and during the night.
Markers of hyperarousal include increased autonomic activity (heart rate, heart rate variability, etc.) and HPA axis overactivity, which is expressed in an increased output of cortisol during the day and night [30]. On a neurotransmitter level, an overactive orexin system might be critically involved, especially in emotional components of hyperarousal [23].
Neuroimaging research on insomnia indicates hyperactivity of cortico-limbic net-works relative to sleep-promoting networks [4]. Signs of central nervous system (CNS) hyperarousal in insomnia further include an increase in fast-frequency EEG activity (e.g., in the sigma, beta and gamma bands) during sleep (see, for example, Feige et al. [11]). In addition, as predicted with the hyperarousal model, there is also evidence of increased arousal in the wake EEG [42].
4.4. REM Sleep Instability
A well-replicated finding in patients with insomnia is an increase in micro-arousals during sleep. Regarding this, an important role for a disturbance of REM sleep (either termed REM sleep instability or restless REM sleep) has been postulated [3,6] regarding the pathophysiology of insomnia and, in particular, for the altered perception of sleep and the inability to down-regulate hyperarousal. For the first time, this was highlighted in 2008 by Feige et al. [14]: in this study, 100 good-sleeper controls and 100 patients with ID were investigated for two nights in a drug-free state with routine polysomnography in a sleep laboratory. The analysis of night 2 (termed baseline), besides looking at routine parameters of sleep continuity, sleep architecture and REM sleep, included scoring of micro-arousals during all stages of sleep (for an example, see Figure 2).
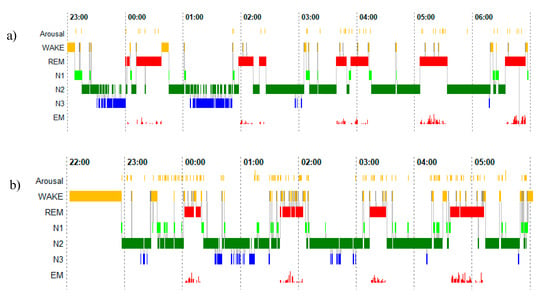
Figure 2.
Polysomnographic profiles of a good sleeper (upper panel) (a) and a patient with insomnia (lower panel) (b). The y-axis displays arousal (micro-arousals), wake and sleep stages (REM, stage N1, N2 and N3) as well as eye movements. The x-axis is the time axis.
When relating subjective wake time to a linear model of the times spent in all PSG sleep stages including wake, only REM sleep time contributed to subjective wake time in addition to PSG wake time, indicating that the amount of REM sleep in insomnia predicts an overestimation of nocturnal wake times. Additionally, the density of micro-arousals was found to be increased relative to good sleepers in REM but not in N2 sleep. Furthermore, the percentage of REM sleep was lower in ID than in good sleepers. These three observations led us to assume that REM sleep quality was modified in ID.
To obtain more direct evidence for this hypothesis, a next study with four nights in the laboratory investigated NREM (stage N2) and REM sleep awakenings in nights 3 and 4 in subgroups of 27 good sleepers and 27 patients with ID [12]. All subjects were awoken three times out of N2 and three times out of REM sleep (not including the first sleep cycle) either in night 3 or 4 according to a counterbalanced design. The main outcome parameter was the judgement of the acute state when awoken, i.e., sleeping vs. being awake. Although more awake judgments were found for both groups when awoken from N2 than from REM sleep, insomnia patients reported having been awake more frequently than good sleepers after REM but not after N2 awakenings [12]. It was found that REM sleep spectral power was related to this increased perceived wakefulness (in particular, lower delta, theta and alpha power in the minute prior to the REM awakenings) [43]. Additionally, mood ratings performed after the awakenings revealed a progressive worsening of mood in insomnia after REM sleep awakenings, which did not occur in stage N2 awakenings nor in good sleepers. These results are only partially consistent with the findings of a previous smaller awakening study by Mercer and colleagues [44]. In this study, insomnia patients had a higher probability of wake judgments when awakened from either N2 or REM sleep. For both groups, a higher probability of awake judgments was observed when awakened from N2 sleep. They suggested that this difference was due to the more wake-like content of N2 mentation, which makes it more difficult to distinguish between sleep and wakefulness. In this context, it may be an important pathophysiological mechanism in insomnia that due to pre-sleep cognitive arousal and the known continuity between waking mental activity and dreaming [45], REM sleep mentation becomes more realistic and thought-like too, which may contribute to the more pronounced misperception of REM sleep noted by Feige et al. [3,12].
In a next step, Feige et al. [13] looked at the continuous measurement of event-related potentials (ERP; more than 10 000 stimuli per night) over the course of the night in 50 good sleepers and 50 patients with ID. In contrast to good sleepers, patients with ID exhibited reduced P2 amplitudes in phasic REM sleep exclusively, but not in any other sleep state. A further topographical analysis showed that this was most likely due to increased mismatch negativity in ID, mirroring increased automated change detection in the auditory system and a concomitant orienting response [13]. The assumption was made that especially phasic REM sleep could be prone to sensory afferences in ID, thus contributing to the perception of being awake instead of sleeping/dreaming. These series of experiments emphasize the important role of REM sleep and its instability in insomnia. In an ongoing study, we are now investigating the impact of two bedtime stories (confrontation—a story about insomnia and its consequences vs. distraction—a very funny story without any insomnia-related content) on PSG recorded sleep and event-related potentials in ID.
Wassing et al. [46,47,48,49] conducted experiments to further elucidate the underlying mechanisms and showed that REM sleep disturbances hamper the nocturnal adaptation of limbic circuits (as a response to shameful experiences). As a consequence, difficulties in resolving distress may occur, which may be a crucial component of the development and maintenance of hyperarousal as well as the risk to develop other mental disorders. This relationship was confirmed with other studies [50,51]. Interestingly, unperturbed REM sleep is accompanied with the prolonged silence of the locus coeruleus (LC), which in turn is coupled to a decrease in cerebral norepinephrine [52].
REM sleep is supposed to serve the limbic reactivation of emotional memory traces. Van Someren [9] postulated that increased levels of norepinephrine during restless REM sleep could disrupt synaptic plasticity processes underlying the adaptation of neuronal engrams that represent distress, and possibly even result in further sensitization. It has also been suggested that low norepinephrine during REM sleep is central to the restoration of norepinephrinergic tone and to allow for low tonic and high phasic LC activity during wakefulness [53]. In the same publication, it is also hypothesized that undisturbed REM sleep over the course of the night, because of the silence of the LC, allows for the integration of emotional memories and helps to balance the emotional equilibrium of the individual.
On a neurobiological level, a role for orexin in these REM sleep disturbances is suggested with the fact that a new generation of pharmacological treatments for insomnia that block orexin-1 and orexin-2 receptors have been shown to promote REM sleep [54].
Given these theoretical considerations backed with first experimental data, REM sleep perturbations in ID might also be interpreted as a major pathway to develop significant psychopathology over the chronic course of the disorder.
5. Insomnia, Hyperarousal and REM Sleep Instability: A Major Pathway to Develop Psychopathology
Instability of REM sleep appears to be closely related to emotional perpetuating factors, thus constituting an important pathway for a subsequent development of depressive and anxiety disorders. Impairments of sleep continuity indeed occur in most mental disorders [55] and insomnia-related problems in children have been associated with problems in socio-emotional development [56]. In adults, it has been shown that insomnia is a predictor of sustained emotional distress and of both anxiety disorders and depression [57,58]. Experimental studies have further demonstrated that insomnia patients compared to those with good sleep report more negative emotions [59,60]. Psychophysiological studies have also demonstrated that patients with insomnia show an emotional bias to sleep-related stimuli with negative valence [61,62]. These data are consistent with the perspective that sleep is a fundamental psychophysiological process owning a key role in the regulation of stress and emotion [63,64].
In an overview paper [1], we outlined in more detail the relationships especially between sleep, insomnia and depressive disorders. Thus, insomnia qualifies as a transdiagnostic factor for psychopathology in general, and especially for mood disorders. The relations between insomnia and depression are bi-directional. Insomnia is a significant predictor of depressive disorders and depressive disorders are frequently accompanied with insomnia symptoms. Insomnia treatment may be even conceived of as a helpful strategy to prevent mood disorders. As discussed in the previous sections, insomnia-related disturbances of REM sleep appear to be an important pathway for the link between insomnia and mental illness. Because REM sleep is the most highly aroused brain state during sleep, it is likely to be particularly susceptible to disturbances due to hyperarousal, suggesting an important link between the concepts of REM sleep instability and hyperarousal in insomnia. Insomnia, hyperarousal and REM sleep instability might in the long run destabilize synaptic plasticity and thereby increase the vulnerability for depressive disorders.
6. Perspectives for the Future
In recent decades, significant progress has been achieved in the understanding of insomnia. Nevertheless, many open questions still remain. In the following, we will outline promising avenues for future research concerning the aetiology and pathophysiology of insomnia.
The fact that all important diagnostic systems (DSM-5, ICD-11 and ICSD-3-TR) are currently in agreement on insomnia disorder [65,66,67] as the main diagnostic entity carries huge potential to achieve greater comparability of insomnia research from different parts of the world. Aggregating data from different insomnia centres could also be beneficial to overcome the issues of small sample sizes and a poor replicability of findings. In addition to the use of consistent diagnostic criteria, this would require the application of standard methods and paradigms across different laboratories.
In spite of the overarching category of ID, the presence of different insomnia sub-types should not be overlooked. In this regard, adopting a data-driven approach to delineate and characterize such subtypes appears to be reasonable [68]. This could be enhanced by adding relevant questionnaires and physiological data.
Given the high costs and artificial character of sleep laboratory settings, a need is evident to develop home-based EEG measures that are easy to use and allow for repeated CNS-based measurements in the patients’ natural environment, thereby going beyond classical actigraphy [69]. This would enable more fine-grained studies on the dynamics of features that reflect sleep drive and characteristics of REM sleep both over the long-term and in the context of treatments.
Since the concept of hyperarousal plays a central role in almost all insomnia models, the development of a hyperarousal test should be considered. At best, this could be performed during the day. Considering that the general tendency to hyperarousal can be regarded as a central predisposing factor, such a test could also help to evaluate an individual’s risk for the development of chronic insomnia. In addition, data from a corresponding test could be used to relate them to (epi-)genetic data and help to refine the clinical diagnosis and personalize therapy by identifying specific hyperarousal profiles.
To examine which sleep characteristics govern the decrease in distress overnight (from full adaptation to maladaptive sensitization), it seems necessary to conduct repeated measurements of hyperarousal from evening to morning [47,49].
Finally, we still require a deeper understanding of the psycho-neurobiological mechanisms of insomnia to evaluate the treatment effects of cognitive behavioural therapy for insomnia (CBT-I) beyond mere subjective measures and help develop complementary therapeutic approaches. In this context, dual orexin receptor antagonists have emerged as promising new pharmacological treatment strategies. However, the precise role of orexin in the pathophysiology of insomnia, particularly with regard to REM sleep disturbances, as well as the role of other neurotransmitters known to be involved in the regulation of sleep, such as acetylcholine and dopamine, requires further investigation.
Author Contributions
Conceptualization, D.R. and B.F.; writing—original draft preparation, D.R.; writing—review and editing, D.R., R.J.D., F.B., L.P. and B.F.; visualization, D.R., R.J.D. and B.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Riemann, D.; Krone, L.B.; Wulff, K.; Nissen, C. Sleep, Insomnia, and Depression. Neuropsychopharmacology 2020, 45, 74–89. [Google Scholar] [CrossRef] [PubMed]
- Riemann, D.; Spiegelhalder, K.; Feige, B.; Voderholzer, U.; Berger, M.; Perlis, M.; Nissen, C. The Hyperarousal Model of Insomnia: A Review of the Concept and Its Evidence. Sleep Med. Rev. 2010, 14, 19–31. [Google Scholar] [CrossRef]
- Riemann, D.; Spiegelhalder, K.; Nissen, C.; Hirscher, V.; Baglioni, C.; Feige, B. REM Sleep Instability—A New Pathway for Insomnia? Pharmacopsychiatry 2012, 45, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Riemann, D.; Nissen, C.; Palagini, L.; Otte, A.; Perlis, M.L.; Spiegelhalder, K. The Neurobiology, Investigation, and Treatment of Chronic Insomnia. Lancet Neurol. 2015, 14, 547–558. [Google Scholar] [CrossRef]
- Riemann, D.; Benz, F.; Dressle, R.J.; Espie, C.A.; Johann, A.F.; Blanken, T.F.; Leerssen, J.; Wassing, R.; Henry, A.L.; Kyle, S.D.; et al. Insomnia Disorder: State of the Science and Challenges for the Future. J. Sleep Res. 2022, 31, e13604. [Google Scholar] [CrossRef]
- Morin, C.M.; Drake, C.L.; Harvey, A.G.; Krystal, A.D.; Manber, R.; Riemann, D.; Spiegelhalder, K. Insomnia Disorder. Nat. Rev. Dis. Primers 2015, 1, 15026. [Google Scholar] [CrossRef] [PubMed]
- Dressle, R.J.; Riemann, D. Hyperarousal in Insomnia Disorder: Current Evidence and Potential Mechanisms. J. Sleep Res. 2023, e13928. [Google Scholar] [CrossRef] [PubMed]
- Perlis, M.L.; Giles, D.E.; Mendelson, W.B.; Bootzin, R.R.; Wyatt, J.K. Psychophysiological Insomnia: The Behavioural Model and a Neurocognitive Perspective. J. Sleep Res. 1997, 6, 179–188. [Google Scholar] [CrossRef]
- Van Someren, E.J.W. Brain Mechanisms of Insomnia: New Perspectives on Causes and Consequences. Physiol. Rev. 2021, 101, 995–1046. [Google Scholar] [CrossRef]
- Riemann, D.; Spiegelhalder, K.; Espie, C.; Pollmächer, T.; Léger, D.; Bassetti, C.; van Someren, E. Chronic Insomnia: Clinical and Research Challenges-an Agenda. Pharmacopsychiatry 2011, 44, 1–14. [Google Scholar] [CrossRef]
- Feige, B.; Baglioni, C.; Spiegelhalder, K.; Hirscher, V.; Nissen, C.; Riemann, D. The Microstructure of Sleep in Primary Insomnia: An Overview and Extension. Int. J. Psychophysiol. 2013, 89, 171–180. [Google Scholar] [CrossRef]
- Feige, B.; Nanovska, S.; Baglioni, C.; Bier, B.; Cabrera, L.; Diemers, S.; Quellmalz, M.; Siegel, M.; Xeni, I.; Szentkiralyi, A.; et al. Insomnia—Perchance a Dream? Results from a NREM/REM Sleep Awakening Study in Good Sleepers and Patients with Insomnia. Sleep 2018, 41, zsy032. [Google Scholar] [CrossRef] [PubMed]
- Feige, B.; Baglioni, C.; Boehm, P.; Heinrich, A.; Trumm, S.; Benz, F.; Nissen, C.; Domschke, K.; Frase, L.; Riemann, D. Event-Related Potentials in Insomnia Reflect Altered Perception of Sleep. Sleep 2021, 44, zsab137. [Google Scholar] [CrossRef] [PubMed]
- Feige, B.; Al-Shajlawi, A.; Nissen, C.; Voderholzer, U.; Hornyak, M.; Spiegelhalder, K.; Kloepfer, C.; Perlis, M.; Riemann, D. Does REM Sleep Contribute to Subjective Wake Time in Primary Insomnia? A Comparison of Polysomnographic and Subjective Sleep in 100 Patients. J. Sleep Res. 2008, 17, 180–190. [Google Scholar] [CrossRef]
- Spielman, A.J.; Caruso, L.S.; Glovinsky, P.B. A Behavioral Perspective on Insomnia Treatment. Psychiatr. Clin. N. Am. 1987, 10, 541–553. [Google Scholar] [CrossRef]
- Palagini, L.; Biber, K.; Riemann, D. The Genetics of Insomnia-Evidence for Epigenetic Mechanisms? Sleep Med. Rev. 2014, 18, 225–235. [Google Scholar] [CrossRef]
- Palagini, L.; Geoffroy, P.A.; Gehrman, P.R.; Miniati, M.; Gemignani, A.; Riemann, D. Potential Genetic and Epigenetic Mechanisms in Insomnia: A Systematic Review. J. Sleep. Res. 2023, e13868. [Google Scholar] [CrossRef]
- Watanabe, K.; Jansen, P.R.; Savage, J.E.; Nandakumar, P.; Wang, X.; 23andMe Research Team; Hinds, D.A.; Gelernter, J.; Levey, D.F.; Polimanti, R.; et al. Genome-Wide Meta-Analysis of Insomnia Prioritizes Genes Associated with Metabolic and Psychiatric Pathways. Nat. Genet. 2022, 54, 1125–1132. [Google Scholar] [CrossRef] [PubMed]
- Jansen, P.R.; Watanabe, K.; Stringer, S.; Skene, N.; Bryois, J.; Hammerschlag, A.R.; de Leeuw, C.A.; Benjamins, J.S.; Muñoz-Manchado, A.B.; Nagel, M.; et al. Genome-Wide Analysis of Insomnia in 1,331,010 Individuals Identifies New Risk Loci and Functional Pathways. Nat. Genet. 2019, 51, 394–403. [Google Scholar] [CrossRef]
- Lane, J.M.; Jones, S.E.; Dashti, H.S.; Wood, A.R.; Aragam, K.G.; van Hees, V.T.; Strand, L.B.; Winsvold, B.S.; Wang, H.; Bowden, J.; et al. Biological and Clinical Insights from Genetics of Insomnia Symptoms. Nat. Genet. 2019, 51, 387–393. [Google Scholar] [CrossRef]
- Borbély, A.A. A Two Process Model of Sleep Regulation. Hum. Neurobiol. 1982, 1, 195–204. [Google Scholar]
- Saper, C.B.; Scammell, T.E.; Lu, J. Hypothalamic Regulation of Sleep and Circadian Rhythms. Nature 2005, 437, 1257–1263. [Google Scholar] [CrossRef]
- Palagini, L.; Geoffroy, P.A.; Balestrieri, M.; Miniati, M.; Biggio, G.; Liguori, C.; Menicucci, D.; Ferini-Strambi, L.; Nobili, L.; Riemann, D.; et al. Current Models of Insomnia Disorder: A Theoretical Review on the Potential Role of the Orexinergic Pathway with Implications for Insomnia Treatment. J. Sleep Res. 2023, 32, e13825. [Google Scholar] [CrossRef] [PubMed]
- Weber, F.; Hoang Do, J.P.; Chung, S.; Beier, K.T.; Bikov, M.; Saffari Doost, M.; Dan, Y. Regulation of REM and Non-REM Sleep by Periaqueductal GABAergic Neurons. Nat. Commun. 2018, 9, 354. [Google Scholar] [CrossRef] [PubMed]
- Drake, C.; Pillai, V.; Roth, T. Stress and Sleep Reactivity: A Prospective Investigation of the Stress-Diathesis Model of Insomnia. Sleep 2014, 37, 1295–1304. [Google Scholar] [CrossRef]
- Reffi, A.N.; Kalmbach, D.A.; Cheng, P.; Drake, C.L. The Sleep Response to Stress: How Sleep Reactivity Can Help Us Prevent Insomnia and Promote Resilience to Trauma. J. Sleep Res. 2023, e13892. [Google Scholar] [CrossRef] [PubMed]
- Dekker, K.; Blanken, T.F.; Van Someren, E.J.W. Insomnia and Personality-a Network Approach. Brain Sci. 2017, 7, E28. [Google Scholar] [CrossRef]
- van de Laar, M.; Verbeek, I.; Pevernagie, D.; Aldenkamp, A.; Overeem, S. The Role of Personality Traits in Insomnia. Sleep Med. Rev. 2010, 14, 61–68. [Google Scholar] [CrossRef]
- Ellis, J.G.; Gehrman, P.; Espie, C.A.; Riemann, D.; Perlis, M.L. Acute Insomnia: Current Conceptualizations and Future Directions. Sleep Med. Rev. 2012, 16, 5–14. [Google Scholar] [CrossRef]
- Dressle, R.J.; Feige, B.; Spiegelhalder, K.; Schmucker, C.; Benz, F.; Mey, N.C.; Riemann, D. HPA Axis Activity in Patients with Chronic Insomnia: A Systematic Review and Meta-Analysis of Case-Control Studies. Sleep Med. Rev. 2022, 62, 101588. [Google Scholar] [CrossRef]
- Espie, C.A.; Broomfield, N.M.; MacMahon, K.M.A.; Macphee, L.M.; Taylor, L.M. The Attention–Intention–Effort Pathway in the Development of Psychophysiologic Insomnia: A Theoretical Review. Sleep Med. Rev. 2006, 10, 215–245. [Google Scholar] [CrossRef]
- Harvey, A.G. A Cognitive Model of Insomnia. Behav. Res. Ther. 2002, 40, 869–893. [Google Scholar] [CrossRef] [PubMed]
- Waine, J.; Broomfield, N.M.; Banham, S.; Espie, C.A. Metacognitive Beliefs in Primary Insomnia: Developing and Validating the Metacognitions Questionnaire—Insomnia (MCQ-I). J. Behav. Ther. Exp. Psychiatry 2009, 40, 15–23. [Google Scholar] [CrossRef]
- Carney, C.E.; Edinger, J.D.; Morin, C.M.; Manber, R.; Rybarczyk, B.; Stepanski, E.J.; Wright, H.; Lack, L. Examining Maladaptive Beliefs about Sleep across Insomnia Patient Groups. J. Psychosom. Res. 2010, 68, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Baglioni, C.; Johann, A.F.; Benz, F.; Steinmetz, L.; Meneo, D.; Frase, L.; Kuhn, M.; Ohler, M.; Huart, S.; Speiser, N.; et al. Interactions between Insomnia, Sleep Duration and Emotional Processes: An Ecological Momentary Assessment of Longitudinal Influences Combining Self-report and Physiological Measures. J. Sleep Res. 2023, e14001. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.R.; Schneider, G.; Rasch, T.; Schürrmann, H.; Paterok, B.; Müller, T.; Becker-Carus, C. Fragebogen zur Erfassung Spezifischer Persönlichkeitseigenschaften Schlafgestörter II (FEPS II); Hogrefe: Göttingen, Germany, 1996. [Google Scholar]
- Spiegelhalder, K.; Regen, W.; Feige, B.; Hirscher, V.; Unbehaun, T.; Nissen, C.; Riemann, D.; Baglioni, C. Sleep-Related Arousal versus General Cognitive Arousal in Primary Insomnia. J. Clin. Sleep Med. 2012, 8, 431–437. [Google Scholar] [CrossRef]
- Harris, K.; Spiegelhalder, K.; Espie, C.A.; MacMahon, K.M.A.; Woods, H.C.; Kyle, S.D. Sleep-Related Attentional Bias in Insomnia: A State-of-the-Science Review. Clin. Psychol. Rev. 2015, 42, 16–27. [Google Scholar] [CrossRef]
- Bootzin, R.R.; Epstein, D.; Wood, J.M. Stimulus Control Instructions. In Case Studies in Insomnia; Hauri, P.J., Ed.; Critical Issues in Psychiatry; Springer US: Boston, MA, USA, 1991; pp. 19–28. ISBN 978-1-4757-9586-8. [Google Scholar]
- Dressle, R.J.; Riemann, D.; Spiegelhalder, K.; Frase, L.; Perlis, M.L.; Feige, B. On the Relationship between EEG Spectral Analysis and Pre-sleep Cognitive Arousal in Insomnia Disorder: Towards an Integrated Model of Cognitive and Cortical Arousal. J. Sleep Res. 2023, 32, e13861. [Google Scholar] [CrossRef]
- Vgontzas, A.N.; Fernandez-Mendoza, J.; Liao, D.; Bixler, E.O. Insomnia with Objective Short Sleep Duration: The Most Biologically Severe Phenotype of the Disorder. Sleep Med. Rev. 2013, 17, 241–254. [Google Scholar] [CrossRef]
- Colombo, M.A.; Ramautar, J.R.; Wei, Y.; Gomez-Herrero, G.; Stoffers, D.; Wassing, R.; Benjamins, J.S.; Tagliazucchi, E.; van der Werf, Y.D.; Cajochen, C.; et al. Wake High-Density Electroencephalographic Spatiospectral Signatures of Insomnia. Sleep 2016, 39, 1015–1027. [Google Scholar] [CrossRef]
- Benz, F.; Riemann, D.; Feige, B. Dreaming and Insomnia: Link between Physiological REM Parameters and Mentation Characteristics. Brain Sci. 2020, 10, 378. [Google Scholar] [CrossRef] [PubMed]
- Mercer, J.D.; Bootzin, R.R.; Lack, L.C. Insomniacs’ Perception of Wake Instead of Sleep. Sleep 2002, 25, 559–566. [Google Scholar] [CrossRef]
- Schredl, M. Continuity between Waking and Dreaming: A Proposal for a Mathematical Model. Sleep Hypn. 2003, 5, 26–39. [Google Scholar]
- Wassing, R.; Benjamins, J.S.; Dekker, K.; Moens, S.; Spiegelhalder, K.; Feige, B.; Riemann, D.; van der Sluis, S.; Van Der Werf, Y.D.; Talamini, L.M.; et al. Slow Dissolving of Emotional Distress Contributes to Hyperarousal. Proc. Natl. Acad. Sci. USA 2016, 113, 2538–2543. [Google Scholar] [CrossRef] [PubMed]
- Wassing, R.; Lakbila-Kamal, O.; Ramautar, J.R.; Stoffers, D.; Schalkwijk, F.; Van Someren, E.J.W. Restless REM Sleep Impedes Overnight Amygdala Adaptation. Curr. Biol. 2019, 29, 2351–2358.e4. [Google Scholar] [CrossRef]
- Wassing, R.; Schalkwijk, F.; Lakbila-Kamal, O.; Ramautar, J.R.; Stoffers, D.; Mutsaerts, H.J.M.M.; Talamini, L.M.; Van Someren, E.J.W. Haunted by the Past: Old Emotions Remain Salient in Insomnia Disorder. Brain 2019, 142, 1783–1796. [Google Scholar] [CrossRef]
- Wassing, R.; Benjamins, J.S.; Talamini, L.M.; Schalkwijk, F.; Van Someren, E.J.W. Overnight Worsening of Emotional Distress Indicates Maladaptive Sleep in Insomnia. Sleep 2019, 42, zsy268. [Google Scholar] [CrossRef] [PubMed]
- Halonen, R.; Kuula, L.; Makkonen, T.; Kauramäki, J.; Pesonen, A.-K. Self-Conscious Affect Is Modulated by Rapid Eye Movement Sleep but Not by Targeted Memory Reactivation-a Pilot Study. Front. Psychol. 2021, 12, 730924. [Google Scholar] [CrossRef]
- Pesonen, A.-K.; Gradisar, M.; Kuula, L.; Short, M.; Merikanto, I.; Tark, R.; Räikkönen, K.; Lahti, J. REM Sleep Fragmentation Associated with Depressive Symptoms and Genetic Risk for Depression in a Community-Based Sample of Adolescents. J. Affect. Disord. 2019, 245, 757–763. [Google Scholar] [CrossRef]
- Kjaerby, C.; Andersen, M.; Hauglund, N.; Untiet, V.; Dall, C.; Sigurdsson, B.; Ding, F.; Feng, J.; Li, Y.; Weikop, P.; et al. Memory-Enhancing Properties of Sleep Depend on the Oscillatory Amplitude of Norepinephrine. Nat. Neurosci. 2022, 25, 1059–1070. [Google Scholar] [CrossRef]
- Goldstein, A.N.; Walker, M.P. The Role of Sleep in Emotional Brain Function. Annu. Rev. Clin. Psychol. 2014, 10, 679–708. [Google Scholar] [CrossRef] [PubMed]
- Clark, J.; Brian, M.; Drummond, S.; Hoyer, D.; Jacobson, L. Effects of Orexin Receptor Antagonism on Human Sleep Architecture: A Systematic Review. Sleep Med. Rev. 2020, 53, 101332. [Google Scholar] [CrossRef] [PubMed]
- Baglioni, C.; Nanovska, S.; Regen, W.; Spiegelhalder, K.; Feige, B.; Nissen, C.; Reynolds, C.F.; Riemann, D. Sleep and Mental Disorders: A Meta-Analysis of Polysomnographic Research. Psychol. Bull. 2016, 142, 969–990. [Google Scholar] [CrossRef] [PubMed]
- Sadeh, A.; Tikotzky, L.; Kahn, M. Sleep in Infancy and Childhood: Implications for Emotional and Behavioral Difficulties in Adolescence and Beyond. Curr. Opin. Psychiatry 2014, 27, 453–459. [Google Scholar] [CrossRef]
- Baglioni, C.; Battagliese, G.; Feige, B.; Spiegelhalder, K.; Nissen, C.; Voderholzer, U.; Lombardo, C.; Riemann, D. Insomnia as a Predictor of Depression: A Meta-Analytic Evaluation of Longitudinal Epidemiological Studies. J. Affect. Disord. 2011, 135, 10–19. [Google Scholar] [CrossRef]
- Hertenstein, E.; Feige, B.; Gmeiner, T.; Kienzler, C.; Spiegelhalder, K.; Johann, A.; Jansson-Fröjmark, M.; Palagini, L.; Rücker, G.; Riemann, D.; et al. Insomnia as a Predictor of Mental Disorders: A Systematic Review and Meta-Analysis. Sleep Med. Rev. 2019, 43, 96–105. [Google Scholar] [CrossRef]
- McCrae, C.S.; McNamara, J.P.H.; Rowe, M.A.; Dzierzewski, J.M.; Dirk, J.; Marsiske, M.; Craggs, J.G. Sleep and Affect in Older Adults: Using Multilevel Modeling to Examine Daily Associations. J. Sleep Res. 2008, 17, 42–53. [Google Scholar] [CrossRef]
- Scott, B.A.; Judge, T.A. Insomnia, Emotions, and Job Satisfaction: A Multilevel Study. J. Manag. 2006, 32, 622–645. [Google Scholar] [CrossRef]
- Baglioni, C.; Spiegelhalder, K.; Regen, W.; Feige, B.; Nissen, C.; Lombardo, C.; Violani, C.; Hennig, J.; Riemann, D. Insomnia Disorder Is Associated with Increased Amygdala Reactivity to Insomnia-Related Stimuli. Sleep 2014, 37, 1907–1917. [Google Scholar] [CrossRef]
- Baglioni, C.; Lombardo, C.; Bux, E.; Hansen, S.; Salveta, C.; Biello, S.; Violani, C.; Espie, C.A. Psychophysiological Reactivity to Sleep-Related Emotional Stimuli in Primary Insomnia. Behav. Res. Ther. 2010, 48, 467–475. [Google Scholar] [CrossRef]
- Hagger, M.S. Sleep, Self-Regulation, Self-Control and Health. Stress Health 2010, 26, 181–185. [Google Scholar] [CrossRef]
- Palmer, C.A.; Alfano, C.A. Sleep and Emotion Regulation: An Organizing, Integrative Review. Sleep Med. Rev. 2017, 31, 6–16. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013; ISBN 978-0-89042-554-1. [Google Scholar]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 11th ed.; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- American Academy of Sleep. International Classification of Sleep Disorders, 3rd ed.; Text Revision (ICSD-3-TR); American Academy of Sleep Medicine: Darien, IL, USA, 2023. [Google Scholar]
- Blanken, T.F.; Benjamins, J.S.; Borsboom, D.; Vermunt, J.K.; Paquola, C.; Ramautar, J.; Dekker, K.; Stoffers, D.; Wassing, R.; Wei, Y.; et al. Insomnia Disorder Subtypes Derived from Life History and Traits of Affect and Personality. Lancet Psychiatry 2019, 6, 151–163. [Google Scholar] [CrossRef] [PubMed]
- Debener, S.; Emkes, R.; De Vos, M.; Bleichner, M. Unobtrusive Ambulatory EEG Using a Smartphone and Flexible Printed Electrodes around the Ear. Sci. Rep. 2015, 5, 16743. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).