Comparative In Vitro Analysis of Mechanical Properties in Three High-Viscosity Bulk-Fill Composite Resins
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Materials
- Group A (Filtek™ One Bulk Fill Restorative)—3M ESPE, St. Paul, MN, USA; Shade: A2; Lot: 11575350; Exp.: 05/2027.
- Group B (Tetric® N-Ceram Bulk Fill)—Ivoclar Vivadent, Schaan, Liechtenstein; Shade: IVB; Lot: Z07115; Exp.: 05/2028.
- Group C (Opus™ Bulk Fill APS)—FGM, Joinville, Brazil; Shade: A2; Lot: 051224; Exp.: 12/2026. The following commercially available BFCRs were tested:
Chemical Composition of the Materials Evaluated
2.3. Specimen Preparation
2.4. Three-Point Bending Test
- Flexural strength (FS, MPa):
- Flexural modulus (EM, GPa):
- Maximum displacement (δmax, mm):
- Maximum strain (εmax, %):
2.5. Bias Control and Blinding
2.6. Sample Size Calculation
2.7. Statistical Analysis
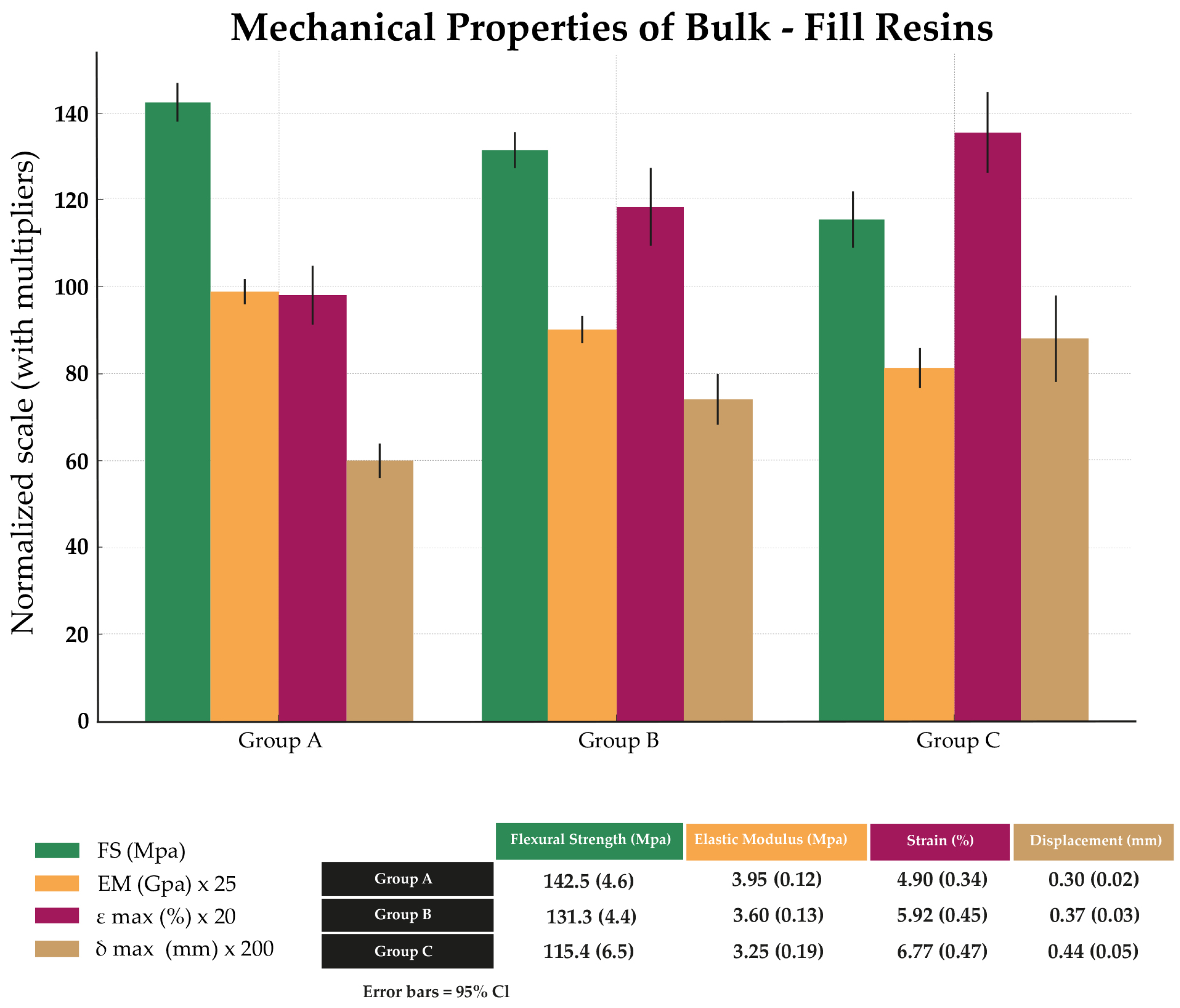
3. Results
3.1. Assessment of Normality and Homogeneity of Variances
Verification of the Homogeneity of Variances Assumption
3.2. Comparison of Mechanical Properties by ANOVA
3.3. Multivariate and Correlational Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ANOVA | Analysis of variance |
| AUDMA | Aromatic urethane dimethacrylate |
| BFCRs | Bulk-fill composite resins |
| CI | Confidence interval |
| 95% CI | 95% confidence interval |
| DTS | Diametral tensile strength |
| EM | Elastic modulus |
| F | Test statistic (ANOVA/Levene) |
| FS | Flexural strength |
| GPa | Gigapascal |
| HSD | Honestly significant difference (Tukey) |
| ISO | International Organization for Standardization |
| MANOVA | Multivariate analysis of variance |
| Kn | Kilonewton |
| J/cm2 | |
| W/cm2 | |
| LED | light-emitting diode |
| H2 | |
| MPa | Megapascal |
| p | p-value |
| ρ | Spearman correlation coefficient |
| W | Shapiro–Wilk statistic |
| Λ | Wilks’ lambda |
| η2 | Partial eta-squared |
| ε | Strain |
| δ | Displacement |
| δmax | Maximum displacement |
| εmax | Maximum strain |
References
- Bonsor, S.J. Resin-Based Composite Materials: A Science Update. Dent. Update 2019, 46, 304–312. [Google Scholar] [CrossRef]
- Antoniac, I.V. (Ed.) Handbook of Bioceramics and Biocomposites; Springer: Cham, Switzerland, 2016. [Google Scholar] [CrossRef]
- Wang, K.; Peng, Q.; Yao, J.; Wang, Z. Accurate Assessment of the Three-Dimensional Shrinkage Stress Evolution for Photopolymerized Dental Filling Materials: Mechano-Chemo-Thermo-Coupled Finite Element Modeling and Experimental Validation. Dent. Mater. 2025, 41, 319–330. [Google Scholar] [CrossRef]
- Guan, X.; Zhu, T.; Zhang, D. Development in Polymerization Shrinkage Control of Dental Light-Cured Resin Composites: A Literature Review. J. Adhes. Sci. Technol. 2023, 37, 602–623. [Google Scholar] [CrossRef]
- Medarametla, R.; Govula, K.; Anumula, L.; Chinni, S.; Yendluri, P.K. Clinical Evaluation of Two Different Nanohybrid Composite Restorations Using FDI Criteria—A Randomized Clinical Trial. J. Interdiscip. Dent. 2024, 14, 41–50. [Google Scholar] [CrossRef]
- Vasconcelos-Monteiro, R.; Cavalcanti-Taguchi, C.M.; Gondo-Machado, R.; Batalha-Silva, S.; Karina-Bernardon, J.; Monteiro-Junior, S. Bulk-Fill Composite Restorations: Step-by-Step Description of Clinical Restorative Techniques—Case Reports. Odovtos Int. J. Dent. Sci. 2019, 21, 23–31. [Google Scholar] [CrossRef]
- Skrinjaric, T.; Gorseta, K.; Bagaric, J.; Bucevic Sojcic, P.; Stojanovic, J.; Marks, L.A.M. Comparison of Microhardness and Depth of Cure of Six Bulk-Fill Resin Composites. J. Compos. Sci. 2025, 9, 418. [Google Scholar] [CrossRef]
- Cabadağ, Ö.G.; Misilli, T.; Gönülol, N. A Current Overview of Bulk-Fill Composites. Selcuk Dent. J. 2021, 8, 220–228. [Google Scholar] [CrossRef]
- Grandon, F.; Muster, M.; Wendler, M. Solving Color Irregularities with a Bioactive Bulk-Fill Restorative System: Case Report and 24-Months Follow-Up. J. Oral Res. 2020, 9, 430–436. [Google Scholar] [CrossRef]
- Rizzante, F.A.P.; Mondelli, R.F.L.; Furuse, A.Y.; Borges, A.F.S.; Mendonça, G.; Ishikiriama, S.K. Shrinkage Stress and Elastic Modulus Assessment of Bulk-Fill Composites. J. Appl. Oral Sci. 2019, 27, e20180132. [Google Scholar] [CrossRef]
- Arafa, N.; Sherief, D.I.; Elmalawanya, L.M.; Nassif, M.S. Performance of RAFT-Based and Conventional Bulk-Fill Composites Cured with Conventional and High-Irradiance Photocuring: A Comparative Study. BMC Oral Health 2025, 25, 714. [Google Scholar] [CrossRef]
- Tauböck, T.T.; Jäger, F.; Attin, T. Polymerization Shrinkage and Shrinkage Force Kinetics of High- and Low-Viscosity Dimethacrylate- and Ormocer-Based Bulk-Fill Resin Composites. Odontology 2019, 107, 103–110. [Google Scholar] [CrossRef]
- Rosa de Lacerda, L.; Bossardi, M.; Silveira Mitterhofer, W.J.; Galbiatti de Carvalho, F.; Carlo, H.L.; Piva, E.; Münchow, E.A. New Generation Bulk-Fill Resin Composites: Effects on Mechanical Strength and Fracture Reliability. J. Mech. Behav. Biomed. Mater. 2019, 96, 214–218. [Google Scholar] [CrossRef]
- Shibasaki, S.; Takamizawa, T.; Nojiri, K.; Imai, A.; Tsujimoto, A.; Endo, H.; Suzuki, S.; Suda, S.; Barkmeier, W.W.; Latta, M.A.; et al. Polymerization Behavior and Mechanical Properties of High-Viscosity Bulk-Fill and Low-Shrinkage Resin Composites. Oper. Dent. 2017, 42, E177–E187. [Google Scholar] [CrossRef]
- Cidreira Boaro, L.C.; Pereira Lopes, D.; de Souza, A.S.C.; Lie Nakano, E.; Ayala Perez, M.D.; Pfeifer, C.S.; Gonçalves, F. Clinical Performance and Chemical-Physical Properties of Bulk-Fill Composites Resin—A Systematic Review and Meta-Analysis. Dent. Mater. 2019, 35, e249–e264. [Google Scholar] [CrossRef]
- Abdulmajeed, A.A.; Donovan, T.; Cook, R.; Sulaiman, T.A. Effect of Preheating and Fatiguing on Mechanical Properties of Bulk-Fill and Conventional Composite Resin. Oper. Dent. 2020, 45, 387–395. [Google Scholar] [CrossRef]
- Alavi, F.N.; Ghavami-Lahiji, M.; Habibi, P. Mechanical Performance of a Conventional Resin Composite and Its Bulk-Fill Restorative Counterpart after Long-Term Accelerated Aging. Dent. Med. Probl. 2023, 60, 641–647. [Google Scholar] [CrossRef]
- Tornabene, F.; Hussein, H.A.; Masoud, H.; Saeed, M. Effect of Shade and Light-Curing Intensity on Bulk-Fill Composite: Heat Generation and Chemo-Mechanical Properties (In Vitro Study). J. Compos. Sci. 2024, 8, 237. [Google Scholar] [CrossRef]
- Harahap, S.A.; Eriwati, Y.L.; Triaminingsih, S. Effects of Extended Curing Time on the Diametral Tensile Strength, Degree of Conversion, and Monomer Release of Bulk-Fill Composite Resins. J. Phys. Conf. Ser. 2018, 1073, 052007. [Google Scholar] [CrossRef]
- Comba, A.; Scotti, N.; Maravić, T.; Mazzoni, A.; Carossa, M.; Breschi, L.; Cadenaro, M. Vickers Hardness and Shrinkage Stress Evaluation of Low and High Viscosity Bulk-Fill Resin Composite. Polymers 2020, 12, 1477. [Google Scholar] [CrossRef]
- Zhang, H.; Zhang, M.-L.; Qiu, L.-H.; Yu, J.-T.; Zhan, F.-L. Comparison of Wear Resistance and Flexural Strength of Three Kinds of Bulk-Fill Composite Resins. Shanghai Kou Qiang Yi Xue 2016, 25, 292–295. [Google Scholar]
- Ilie, N.; Bucuta, S.; Draenert, M. Bulk-Fill Resin-Based Composites: An In Vitro Assessment of Their Mechanical Performance. Oper. Dent. 2013, 38, 618–625. [Google Scholar] [CrossRef]
- Foscarini, A.V.; Barros, L.S.; Turssi, C.P.; França, F.M.G.; Basting, R.T.; Vieira, W.F. Flexural Strength of Conventional or Bulk-Fill Resin Composite Repaired with High- or Low-Viscosity Restorative Materials. Oper. Dent. 2023, 48, 677–688. [Google Scholar] [CrossRef]
- Perdigão, J.; Duarte, S.; Gomes, G. Direct Resin-Based Composite Restorations—Clinical Challenges. J. Adhes. Sci. Technol. 2009, 23, 1201–1214. [Google Scholar] [CrossRef]
- Dudea, D.; Alb, C.; Culic, B.; Alb, F. Performance of Dental Composites in Restorative Dentistry. In Handbook of Bioceramics and Biocomposites; Antoniac, I.V., Ed.; Springer: Cham, Switzerland, 2016; pp. 1075–1114. [Google Scholar] [CrossRef]
- Li, W.; Wang, K.; Wang, Z.; Li, B. Optimal Resin Monomer Ratios for Light-Cured Dental Resins. Heliyon 2022, 8, e10554. [Google Scholar] [CrossRef] [PubMed]
- Vicente, T.; Balzer, P.S. Study of Acrylic Resins Modified by Different Particle Sizes for Application in Odontology Area. Matéria 2018, 23, 12210. [Google Scholar] [CrossRef]
- ISO 4049:2019; Dentistry—Polymer-Based Restorative Materials. 5th ed. International Organization for Standardization (ISO): Geneva, Switzerland, 2019.
- Yap, A.U.; Eweis, A.H.; Yahya, N.A. Dynamic and Static Flexural Appraisal of Resin-Based Composites: Comparison of the ISO and Mini-flexural Tests. Oper. Dent. 2018, 43, E223–E231. [Google Scholar] [CrossRef]
- Cilingir, A.; Özsoy, A.; Mert-Eren, M.; Behram, Ö.; Dikmen, B.; Özcan, M. Mechanical Properties of Bulk-Fill versus Nanohybrid Composites: Effect of Layer Thickness and Application Protocols. Braz. Dent. Sci. 2019, 22, 234–242. [Google Scholar] [CrossRef]
- Hirokane, E.; Takamizawa, T.; Tamura, T.; Shibasaki, S.; Tsujimoto, A.; Barkmeier, W.W.; Latta, M.A.; Miyazaki, M. Handling and Mechanical Properties of Low-Viscosity Bulk-Fill Resin Composites. Oper. Dent. 2021, 46, E185–E198. [Google Scholar] [CrossRef] [PubMed]
- di Lauro, A.E.; Ciaramella, S.; Tribst, J.P.M.; Aliberti, A.; Ausiello, P. Comparison of Bulk Polymeric Resin Composite and Hybrid Glass Ionomer Cement in Adhesive Class I Dental Restorations: A 3D Finite Element Analysis. Polymers 2024, 16, 2525. [Google Scholar] [CrossRef]
- Shah, M.B.; Ferracane, J.L.; Kruzic, J.J. R-curve behavior and micromechanisms of fracture in resin based dental restorative composites. J. Mech. Behav. Biomed. Mater. 2009, 2, 502–511. [Google Scholar] [CrossRef]
- Botrel, B.; Condi, M.; Turssi, C.; Gomes-França, F.; Vieira-Junior, W.; Basting, R. Propiedades físicas y mecánicas de compuestos de resina de relleno masivo sometidos a polimerización adicional para su uso en restauraciones semidirectas. Odontol. Oper. 2025, 50, 44–58. [Google Scholar]
- Bastianini, M.E.; do Prado, R.L.; Marsicano, J.A.; Santos, M.C.; dos Santos, M.R.M.; João, S.A.R.O.; Catelan, A.; Pizi, E.C. Influence of Preheating on Elastic Modulus, Flexural and Cohesive Strength of Bulk-Fill Composites. Rev. Matéria 2020, 25, e-12854. [Google Scholar]
- Ferreira, A.F.E.; Silva, I.M.; Dietrich, L.; de Assis Costa, M.D.M.; de Oliveira Andrade, C.M.; da Mota Martins, V. Effect of Low Temperature and Room Temperature on the Depth of Cure of Bulk-Fill Composite Resins. Biosci. J. 2023, 39, e3906. [Google Scholar] [CrossRef]
- Sadananda, V.; Bhat, G.; Hegde, M. Comparative Evaluation of Flexural and Compressive Strengths of Bulk-Fill Composites. Int. J. Adv. Sci. Technol. Res. 2017, 1, 122–131. [Google Scholar]
- Van Ende, A.; De Munck, J.; Lise, D.P.; Van Meerbeek, B. Bulk-Fill Composites: A Review of the Current Literature. J. Adhes. Dent. 2017, 19, 95–109. [Google Scholar] [PubMed][Green Version]
- Marović, D.; Par, M.; Macan, M.; Klarić, N.; Plazonić, I.; Tarle, Z. Aging-Dependent Changes in Mechanical Properties of the New Generation of Bulk-Fill Composites. Materials 2022, 15, 902. [Google Scholar] [CrossRef]
- Par, M.; Plančak, L.; Ratkovski, L.; Tauböck, T.T.; Marović, D.; Attin, T.; Tarle, Z. Improved Flexural Properties of Experimental Resin Composites Functionalized with a Customized Low-Sodium Bioactive Glass. Polymers 2022, 14, 4289. [Google Scholar] [CrossRef]
- Grazioli, G.; Cuevas-Suárez, C.E.; Nakanishi, L.; Francia, A.; de Moraes, R.R. Physicochemical Characterization of Two Bulk-Fill Composites at Different Depths. Restor. Dent. Endod. 2021, 46, e29. [Google Scholar] [CrossRef]
- Bekele, A.; Wadee, M.A.; Phillips, A.T.M. Enhancing Energy Absorption through Sequential Instabilities in Mechanical Metamaterials. R. Soc. Open Sci. 2023, 10, 230677. [Google Scholar] [CrossRef]
- Ferracane, J.L.; Palin, W.M. Effects of Particulate Filler Systems on the Properties and Performance of Dental Polymer Composites. In Non-Metallic Biomaterials for Tooth Repair and Replacement; Woodhead Publishing: Cambridge, UK, 2013; pp. 294–335. [Google Scholar]
- Sulca Gonzales, E.L.; López-Flores, A.I. Flexural Strength of Conventional Flowable, Bulk-Fill Flowable and Highly Filled Flowable Resin Composites: In Vitro Study. Rev. Cient. Odontol. 2023, 11, e161. [Google Scholar] [CrossRef]
- Osiewicz, M.A.; Werner, A.; Roeters, F.J.M.; Kleverlaan, C.J. Wear of Bulk-Fill Resin Composites. Dent. Mater. 2022, 38, 549–553. [Google Scholar] [CrossRef]
- Thadathil Varghese, J.; Babaei, B.; Farrar, P.; Prentice, L.; Prusty, B.G. Influence of Thermal and Thermomechanical Stimuli on a Molar Tooth Treated with Resin-Based Restorative Dental Composites. Dent. Mater. 2022, 38, 811–823. [Google Scholar] [CrossRef]
- Lizymol, P.P. X-ray Microcomputed Tomography (µCT) Studies of a New Low Shrinkage Visible-Light Cure Dental Composite (Ormo 48): Effects of Thermal Cycling on Physical Properties. Trends Biomater. Artif. Organs 2022, 36, 16–21. [Google Scholar]
- Alshali, R.Z.; Salim, N.A.; Satterthwaite, J.D.; Silikas, N. Long-Term Sorption and Solubility of Bulk-Fill and Conventional Resin Composites in Water and Artificial Saliva. J. Dent. 2015, 43, 1511–1518. [Google Scholar] [CrossRef] [PubMed]
- Misilli, T.; Gönülol, N. Water Sorption and Solubility of Bulk-Fill Composites Polymerized with a Third-Generation LED Light-Curing Unit. Braz. Oral Res. 2017, 31, e67. [Google Scholar] [CrossRef]
- Alkattan, R.; Banerji, S.; Deb, S. Damage and Fatigue Failure of Conventional and Bulk-Filled Resin Composites. Open J. Stomatol. 2022, 12, 62–76. [Google Scholar] [CrossRef]
- Basheer, R.R.; Hasanain, F.A.; Abuelenain, D.A. Evaluating Flexure Properties, Hardness, Roughness and Microleakage of High-Strength Injectable Dental Composite: An In Vitro Study. BMC Oral Health 2024, 24, 546. [Google Scholar] [CrossRef] [PubMed]
- Tayebi, G.; Omidian, S.; Abtahi, S.; Ranjbar Hassani, A.; Sherafatmand, Y. Investigation of Mechanical Properties, Shade, and Water Sorption/Solubility of Commercial Composite Resins. Front. Dent. 2024, 21, 43. [Google Scholar] [CrossRef]
- Zhang, A.; Ye, N.; Aregawi, W.; Zhang, L.; Salah, M.; VanHeel, B.; Chew, H.P.; Fok, A.S.L. A Review of Mechano-Biochemical Models for Testing Composite Restorations. J. Dent. Res. 2021, 100, 1030–1038. [Google Scholar] [CrossRef]
- Alshabib, A.; Silikas, N.; Algamaiah, H.; Alayad, A.S.; Alawaji, R.; Almogbel, S.; Aldosari, A.; Alhotan, A. Effect of Fibres on Physico-Mechanical Properties of Bulk-Fill Resin Composites. Polymers 2023, 15, 3452. [Google Scholar] [CrossRef]
- Silikas, N.; Eliades, G.; Watts, D.C. Light Intensity Effects on Resin-Composite Degree of Conversion and Shrinkage Strain. Dent. Mater. 2000, 16, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Szczesio-Wlodarczyk, A.; Fronczek, M.; Ranoszek-Soliwoda, K.; Sokolowski, J.; Bociong, K. Evaluation of Selected Artificial Aging Protocols for Dental Composites, Including Fatigue and Fracture Tests. Appl. Sci. 2024, 14, 6964. [Google Scholar] [CrossRef]






| Material | Monomers (Matrix) | Type of Fillers (Particles) | Filler Content | Photoinitiators/ Technologies |
|---|---|---|---|---|
| Filtek™ One Bulk Fill Restorative (3 M, St. Paul, MN, USA) Shade: A2, Lot: 11575350, Exp.: 05/2027 | AUDMA (aromatic urethane dimethacrylate), AFM (addition–fragmentation monomer), diurethane-DMA, and 1,12-dodecane-DMA. | Silica (20 nm) and zirconia (4–11 nm) non-agglomerated nanoclusters of silica/zirconia; ytterbium trifluoride (radiopaque). | ~76.5 wt% (58.5 vol%) | Stress-relief resin system based on AFM; 3M’s “TRUE nanotechnology”. |
| Tetric® N-Ceram Bulk Fill (Ivoclar Vivadent, Schaan, Liechtenstein), Shade: IVB, Lot: Z07115, Exp.: 05/2028 | Dimethacrylates such as Bis-GMA, Bis-EMA, and UDMA. | Barium–aluminum silicate glass (0.4–0.7 μm), spherical oxide (~160 nm), ytterbium trifluoride (radiopaque), and “Isifillers” (pre-polymerized fillers acting as stress relievers). | Inorganic filler ~75–77 wt% (~53–55 vol%); “standard” filler loading ≥61 vol%. | Ivocerin® photoinitiator (germanium-based, high reactivity) + light sensitivity filter. |
| Opus™ Bulk Fill APS (FGM, Joinville, Brazil), Shade: A2, Lot: 051224, Exp.: 12/2026. | Urethane-based methacrylates (according to technical data sheets); high-viscosity bulk-fill formulation. | Organic–inorganic hybrid filler (average size ~79 vol% or 79 wt% for high viscosity; Flow version declares ~68 wt%). | ~79 wt% (high-viscosity version); Flow version ~68 wt%. | APS (Advanced polymerization system): a combination of photoinitiators for higher depth of cure; increments up to 5 mm. |
| Material | Variable | W (Statistic) | p-Value | Normality |
|---|---|---|---|---|
| Group A | FS (MPa) | 0.97 | 0.89 | Yes (p > 0.05) |
| EM (GPa) | 0.96 | 0.79 | Yes (p > 0.05) | |
| δmax (mm) | 0.97 | 0.87 | Yes (p > 0.05) | |
| εmax (%) | 0.96 | 0.81 | Yes (p > 0.05) | |
| Group B | FS (MPa) | 0.95 | 0.67 | Yes (p > 0.05) |
| EM (GPa) | 0.95 | 0.69 | Yes (p > 0.05) | |
| δmax (mm) | 0.97 | 0.92 | Yes (p > 0.05) | |
| εmax (%) | 0.94 | 0.61 | Yes (p > 0.05) | |
| Group C | FS (MPa) | 0.96 | 0.76 | Yes (p > 0.05) |
| EM (GPa) | 0.95 | 0.69 | Yes (p > 0.05) | |
| δmax (mm) | 0.96 | 0.77 | Yes (p > 0.05) | |
| εmax (%) | 0.92 | 0.23 | Yes (p > 0.05) |
| Variable | F Statistic | p-Value | Homogeneity of Variance |
|---|---|---|---|
| FS (MPa) | 0.34 | 0.71 | Yes (p > 0.05) |
| EM (GPa) | 0.02 | 0.98 | Yes (p > 0.05) |
| δmax (mm) | 1.64 | 0.22 | Yes (p > 0.05) |
| εmax (%) | 0.85 | 0.44 | Yes (p > 0.05) |
| Group1 | Group 2 | Mean diff | p-adj | Lower CI95% | Upper CI95% | Reject H0 |
|---|---|---|---|---|---|---|
| Group A | Group C | −14.74 | 0.000 | −19.71 | −9.78 | True |
| Group A | Group B | −15.84 | 0.000 | −20.80 | −10.87 | True |
| Group C | Group B | −1.09 | 0.849 | −6.06 | 3.87 | False |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santacruz, C.I.; Fajardo, J.I.; Paltán, C.A.; del Carmen Armas-Vega, A.; León, E.V. Comparative In Vitro Analysis of Mechanical Properties in Three High-Viscosity Bulk-Fill Composite Resins. J. Compos. Sci. 2025, 9, 623. https://doi.org/10.3390/jcs9110623
Santacruz CI, Fajardo JI, Paltán CA, del Carmen Armas-Vega A, León EV. Comparative In Vitro Analysis of Mechanical Properties in Three High-Viscosity Bulk-Fill Composite Resins. Journal of Composites Science. 2025; 9(11):623. https://doi.org/10.3390/jcs9110623
Chicago/Turabian StyleSantacruz, Carlos I., Jorge I. Fajardo, César A. Paltán, Ana del Carmen Armas-Vega, and Eleonor Vélez León. 2025. "Comparative In Vitro Analysis of Mechanical Properties in Three High-Viscosity Bulk-Fill Composite Resins" Journal of Composites Science 9, no. 11: 623. https://doi.org/10.3390/jcs9110623
APA StyleSantacruz, C. I., Fajardo, J. I., Paltán, C. A., del Carmen Armas-Vega, A., & León, E. V. (2025). Comparative In Vitro Analysis of Mechanical Properties in Three High-Viscosity Bulk-Fill Composite Resins. Journal of Composites Science, 9(11), 623. https://doi.org/10.3390/jcs9110623









