Impact of Dialysis Clinical Operating Conditions on Human Serum Protein-Mediated Inflammatory Biomarkers Released in Patients Using Polyarylethersulfone Membranes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials and Chemicals
2.2. Membrane Characterization
2.3. In Vitro FB Adsorption
2.4. Clinical Studies
2.4.1. Clinical Study of Inflammatory Biomarkers
2.4.2. In Vitro Incubation of PAES Membrane
3. Results
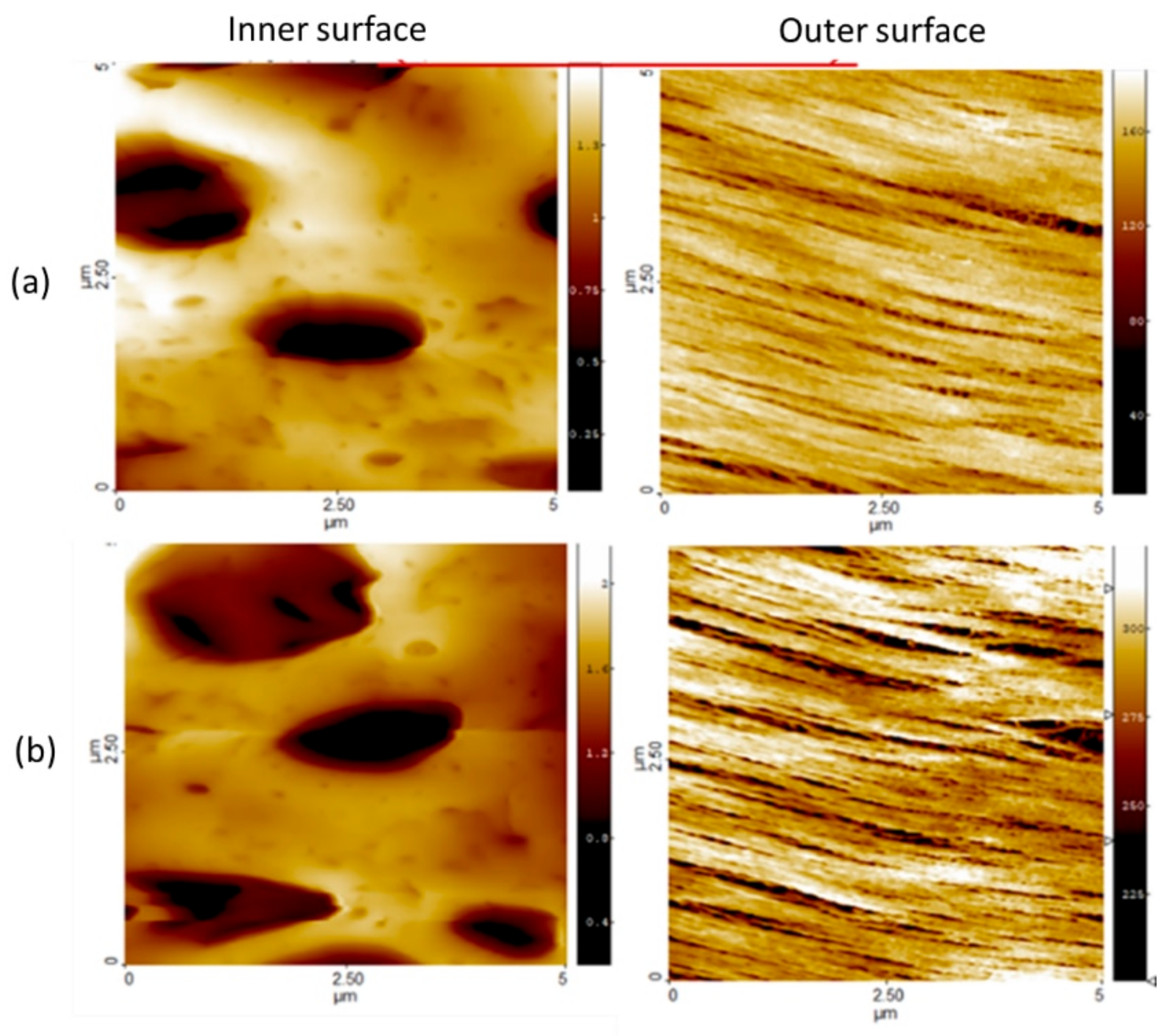
3.1. Membrane Morphology and Surface Charge
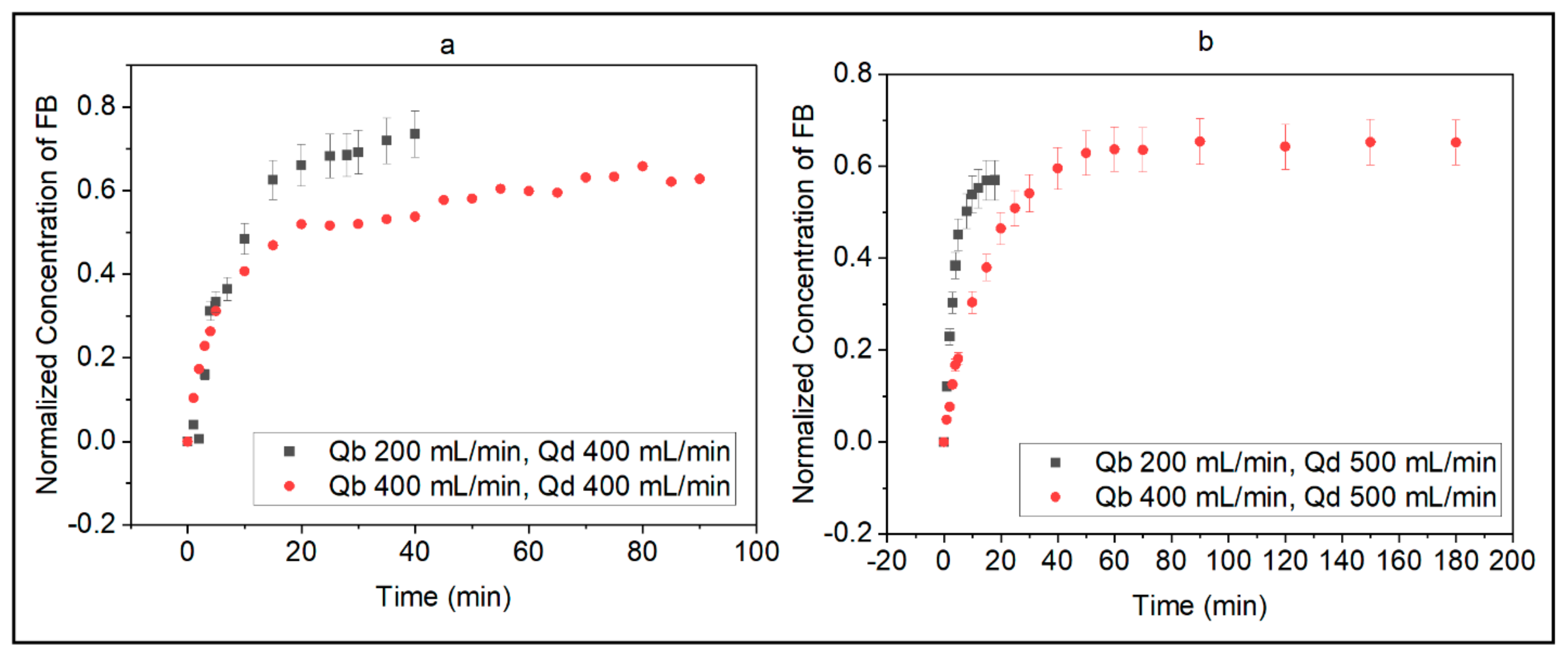
3.2. In Vitro Fibrinogen Adsorption
3.3. Clinical Study of Inflammatory Biomarkers
3.3.1. Influence of Hydrodynamic Conditions on the Release of Inflammatory Biomarkers
3.3.2. Levels of Inflammatory Biomarkers at Various Operating Conditions
Complement Activation Factors
Coagulation and Clotting Factor
Pro-Inflammatory and Pro-Thrombotic Factors
3.3.3. Inflammatory Responses in Male and Female Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bikbov, B.; Purcell, C.A.; Levey, A.S.; Smith, M.; Abdoli, A.; Abebe, M.; Adebayo, O.M.; Afarideh, M.; Agarwal, S.K.; Agudelo-Botero, M.; et al. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef] [Green Version]
- Joshi, P.K.; Rao, P.P. Global pulses scenario: Status and outlook. Ann. N. Y. Acad. Sci. 2016, 1392, 6–17. [Google Scholar] [CrossRef] [Green Version]
- Kooman, J.P.; van der Sande, F.M. COVID-19 in ESRD and Acute Kidney Injury. Blood Purif. 2020, 50, 610–620. [Google Scholar] [CrossRef]
- McAdams, M.; Ostrosky-Frid, M.; Rajora, N.; Hedayati, S.S. Effect of COVID-19 on Kidney Disease Incidence and Management. Kidney360 2020, 2, 141–153. [Google Scholar] [CrossRef]
- Urbani, A.; Sirolli, V.; Lupisella, S.; Levi-Mortera, S.; Pavone, B.; Pieroni, L.; Bonomini, M. Proteomic investigations on the effect of different membrane materials on blood protein adsorption during haemodialysis. Blood Transfus. 2012, 10, s101–s112. [Google Scholar] [CrossRef]
- Urbani, A.; Lupisella, S.; Sirolli, V.; Bucci, S.; Amoroso, L.; Pavone, B.; Pieroni, L.; Sacchetta, P.; Bonomini, M. Proteomic analysis of protein adsorption capacity of different haemodialysis membranes. Mol. BioSyst. 2012, 8, 1029–1039. [Google Scholar] [CrossRef]
- Hakim, R.M. Clinical implications of hemodialysis membrane biocompatibility. Kidney Int. 1993, 44, 484–494. [Google Scholar] [CrossRef] [Green Version]
- Westphalen, H.; Abdelrasoul, A.; Shoker, A. Protein adsorption phenomena in hemodialysis membranes: Mechanisms, influences of clinical practices, modeling, and challenges. Colloid Interface Sci. Commun. 2020, 40, 100348. [Google Scholar] [CrossRef]
- Cozzolino, M.; Mangano, M.; Stucchi, A.; Ciceri, P.; Conte, F.; Galassi, A. Cardiovascular disease in dialysis patients. Nephrol. Dial. Transplant. 2018, 33, iii28–iii34. [Google Scholar] [CrossRef]
- Meijers, B.K.I.; De Loor, H.; Bammens, B.; Verbeke, K.; Vanrenterghem, Y.; Evenepoel, P. p-Cresyl Sulfate and Indoxyl Sulfate in Hemodialysis Patients. Clin. J. Am. Soc. Nephrol. 2009, 4, 1932–1938. [Google Scholar] [CrossRef] [Green Version]
- Burmeister, J.E.; Mosmann, C.B.; Costa, V.B.; Saraiva, R.T.; Grandi, R.R.; Bastos, J.P.; Gonçalves, L.F.; Rosito, G.A. Prevalence of Cardiovascular Risk Factors in Hemodialysis Patients—The CORDIAL Study. Arq. Bras. Cardiol. 2014, 102, 473–480. [Google Scholar] [CrossRef] [PubMed]
- Gatta, A.; Verardo, A.; Bolognesi, M. Hypoalbuminemia. Intern. Emerg. Med. 2012, 7, S193–S199. [Google Scholar] [CrossRef]
- Kirschbaum, B. Hypotransferrinemia of Chronically Hemodialyzed Patients. Artif. Organs 1999, 23, 1047–1054. [Google Scholar] [CrossRef]
- Koga, Y.; Fujieda, H.; Meguro, H.; Ueno, Y.; Aoki, T.; Miwa, K.; Kainoh, M. Biocompatibility of Polysulfone Hemodialysis Membranes and Its Mechanisms: Involvement of Fibrinogen and Its Integrin Receptors in Activation of Platelets and Neutrophils. Artif. Organs 2018, 42, E246–E258. [Google Scholar] [CrossRef]
- Abdelrasoul, A.; Shoker, A. Influence of Hydration Shell of Hemodialysis Clinical Membranes on Surrogate Biomarkers Activation in Uremic Serum of Dialysis Patients. Biomed. Eng. Adv. 2022. [Google Scholar] [CrossRef]
- Nazari, S.; Abdelrasoul, A. Surface Zwitterionization of HemodialysisMembranesfor Hemocompatibility Enhancement and Protein-mediated anti-adhesion: A Critical Review. Biomed. Eng. Adv. 2022, 3, 100026. [Google Scholar] [CrossRef]
- Mollahosseini, A.; Abdelrasoul, A.; Shoker, A. Advances in Membrane Technologies; IntechOpen: Rijeka, Croatia, 2020. [Google Scholar] [CrossRef] [Green Version]
- Mollahosseini, A.; Abdelrasoul, A.; Shoker, A. A critical review of recent advances in hemodialysis membranes hemocompatibility and guidelines for future development. Mater. Chem. Phys. 2020, 248, 122911. [Google Scholar] [CrossRef]
- Mollahosseini, A.; Abdelrasoul, A.; Shoker, A. Latest advances in zwitterionic structures modified dialysis membranes. Mater. Today Chem. 2020, 15, 100227. [Google Scholar] [CrossRef]
- Merle, N.S.; Noé, R.; Halbwachs-Mecarelli, L.; Fremeaux-Bacchi, V.; Roumenina, L.T. Complement System Part II: Role in Immunity. Front. Immunol. 2015, 6, 257. [Google Scholar] [CrossRef] [Green Version]
- Tetta, C.; Roy, T.; Gatti, E.; Cerutti, S. The rise of hemodialysis machines: New technologies in minimizing cardiovascular complications. Expert Rev. Cardiovasc. Ther. 2011, 9, 155–164. [Google Scholar] [CrossRef]
- Adams, R.L.C.; Bird, R.J. Review article: Coagulation cascade and therapeutics update: Relevance to nephrology. Part 1: Overview of coagulation, thrombophilias and history of anticoagulants. Nephrology 2009, 14, 462–470. [Google Scholar] [CrossRef] [PubMed]
- Oikonomopoulou, K.; Ricklin, D.; Ward, P.A.; Lambris, J.D. Interactions between coagulation and complement—Their role in inflammation. In Seminars in Immunopathology; Springer: Berlin/Heidelberg, Germany, 2012; Volume 34, pp. 151–165. [Google Scholar] [CrossRef] [Green Version]
- Westphalen, H.; Saadati, S.; Eduok, U.; Abdelrasoul, A.; Shoker, A.; Choi, P.; Doan, H.; Ein-Mozaffari, F. Case studies of clinical hemodialysis membranes: Influences of membrane morphology and biocompatibility on uremic blood-membrane interactions and inflammatory biomarkers. Sci. Rep. 2020, 10, 14808. [Google Scholar] [CrossRef] [PubMed]
- Westphalen, H.; Abdelrasoul, A.; Shoker, A.; Zhu, N. Assessment of hemodialysis clinical practices using polyaryl ether sulfone-polyvinylpyrrolidone (PAES: PVP) clinical membrane: Modeling of in vitro fibrinogen adsorption, in situ synchrotron-based imaging, and clinical inflammatory biomarkers investigations. Sep. Purif. Technol. 2021, 259, 118136. [Google Scholar] [CrossRef]
- Saadati, S.; Westphalen, H.; Eduok, U.; Abdelrasoul, A.; Shoker, A.; Choi, P.; Doan, H.; Ein-Mozaffari, F.; Zhu, N. Biocompatibility enhancement of hemodialysis membranes using a novel zwitterionic copolymer: Experimental, in situ synchrotron imaging, molecular docking, and clinical inflammatory biomarkers investigations. Mater. Sci. Eng. C 2020, 117, 111301. [Google Scholar] [CrossRef]
- Tanaka, M.; Mochizuki, A. Effect of water structure on blood compatibility—Thermal analysis of water in poly(meth)acrylate. J. Biomed. Mater. Res. 2004, 68A, 684–695. [Google Scholar] [CrossRef]
- Abdelrasoul, A.; Westphalen, H.; Saadati, S.; Shoker, A. Hemodialysis biocompatibility mathematical models to predict the inflammatory biomarkers released in dialysis patients based on hemodialysis membrane characteristics and clinical practices. Sci. Rep. 2021, 11, 23080. [Google Scholar] [CrossRef]
- Eberst, M.E.; Berkowitz, L.R. Hemostasis in renal disease: Pathophysiology and management. Am. J. Med. 1994, 96, 168–179. [Google Scholar] [CrossRef]
- Cheung, A.K.; Levin, N.W.; Greene, T.; Agodoa, L.; Bailey, J.; Beck, G.; Clark, W.; Levey, A.S.; Leypoldt, J.K.; Ornt, D.B.; et al. Effects of High-Flux Hemodialysis on Clinical Outcomes: Results of the HEMO Study. J. Am. Soc. Nephrol. 2003, 14, 3251–3263. [Google Scholar] [CrossRef] [Green Version]
- Abdelrasoul, A.; Shoker, A. Induced hemocompatibility of polyethersulfone (PES) hemodialysis membrane using polyvinylpyrrolidone: Investigation on human serum fibrinogen adsorption and inflammatory biomarkers released. Chem. Eng. Res. Des. 2022, 177, 615–624. [Google Scholar] [CrossRef]
- Straub, R.H. The Complex Role of Estrogens in Inflammation. Endocr. Rev. 2007, 28, 521–574. [Google Scholar] [CrossRef] [Green Version]
- Abdelrasoul, A.; Shoker, A. Investigations on the Impact of Hemodialysis Clinical Practices on Human Plasma Proteins Loss and von Willebrand factor. Kidney Int. Rep. 2022, 7, S258. [Google Scholar] [CrossRef]
- Westphalen, H.; Kalugin, D.; Abdelrasoul, A. Structure, Function, and Adsorption of Highly Abundant Blood Proteins and its Critical Influence on Hemodialysis Patients: A critical Review. Biomed. Eng. Adv. 2021, 2, 100021. [Google Scholar] [CrossRef]
- Eduok, U.; Westphalen, H.; Abdelrasoul, A.; Shoker, A. Influence of UV-irradiation intensity and exposure duration on the hemobiocompatibility enhancement of a novel synthesized phosphobetaine zwitterions polyether sulfone clinical hemodialysis membranes. J. Biomed. Mater. Res. Part B Appl. Biomater. 2022, 110, 573–586. [Google Scholar] [CrossRef]
- Saadati, S.; Eduok, U.; Westphalen, H.; Abdelrasoul, A.; Shoker, A.; Choi, P.; Doan, H.; Ein-Mozaffari, F.; Zhu, N. Assessment of Polyethersulfone and Polyacrylonitrile Hemodialysis Clinical Membranes: In situ Synchrotron-based Imaging of Human Serum Proteins Adsorption, Interaction Analyses, Molecular Docking and Clinical Inflammatory Biomarkers Investigations. Mater. Today Commun. 2021, 29, 102928. [Google Scholar] [CrossRef]
- Mollahosseini, A.; Argumeedi, S.; Abdelrasoul, A.; Shoker, A. A Case Study of Poly(aryl ether sulfone) Hemodialysis Membrane Interactions with Human Blood: Molecular Dynamics Simulation and Experimental Analyses. Comput. Methods Programs Biomed. 2020, 197, 105742. [Google Scholar] [CrossRef]
- Saadati, S.; Eduok, U.; Westphalen, H.; Abdelrasoul, A.; Shoker, A.; Choi, P.; Doan, H.; Ein-Mozaffari, F.; Zhu, N. In situ Synchrotron Imaging of Human Serum Proteins Interactions, Molecular Docking and Inflammatory Biomarkers of Hemocompatible Synthesized Zwitterionic Polymer Coated-Polyvinylidene Fluoride (PVDF) Dialysis Membranes. Surf. Interfaces 2021, 27, 101505. [Google Scholar] [CrossRef]
- Jones, L.A.; Kreem, S.; Shweash, M.; Paul, A.; Alexander, J.; Roberts, C.W. Differential Modulation of TLR3- and TLR4-Mediated Dendritic Cell Maturation and Function by Progesterone. J. Immunol. 2010, 185, 4525–4534. [Google Scholar] [CrossRef]
- Dunn, S.E.; Ousman, S.S.; Sobel, R.A.; Zuniga, L.; Baranzini, S.E.; Youssef, S.; Crowell, A.; Loh, J.; Oksenberg, J.; Steinman, L. Peroxisome proliferator–activated receptor (PPAR)α expression in T cells mediates gender differences in development of T cell–mediated autoimmunity. J. Exp. Med. 2007, 204, 321–330. [Google Scholar] [CrossRef] [Green Version]
- Carrero, J.J. Gender Differences in Chronic Kidney Disease: Underpinnings and Therapeutic Implications. Kidney Blood Press. Res. 2010, 33, 383–392. [Google Scholar] [CrossRef]







| Healthy Control | Hemodialysis Patients | ||||
|---|---|---|---|---|---|
| Variables | Values | N | % | N | % |
| Gender | Female | 1 | 50 | 5 | 41.66 |
| Male | 1 | 50 | 7 | 58.33 | |
| Age | <50 years | 0 | 0 | 5 | 41.66 |
| ≥50 years | 2 | 100 | 7 | 58.33 | |
| Race | Non-black | 2 | 100 | 12 | 100 |
| Black | 0 | 0 | 0 | 0 | |
| BMI a | <27 kg/m2 | 0 | 0 | 0 | 0 |
| ≥27 kg/m2 | 2 | 100 | 12 | 100 | |
| CAD b | Yes | 0 | 0 | 5 | 41.66 |
| NO | 2 | 100 | 7 | 58.33 | |
| Diabetes | Yes | 0 | 0 | 6 | 50.00 |
| No | 2 | 100 | 6 | 50.00 | |
| Hypertension | Yes | 1 | 50 | 10 | 83.33 |
| No | 1 | 50 | 2 | 16.66 | |
| PVD c | Yes | 0 | 0 | 4 | 33.33 |
| No | 2 | 100 | 8 | 66.67 | |
| ESRD duration | <1 year | NA | NA | 1 | 8.33 |
| 1–5 years | NA | NA | 10 | 83.34 | |
| >5 years | NA | NA | 1 | 8.33 | |
| Qb (mL/min) | Qd (mL/min) | BF Rate (mL/min) |
|---|---|---|
| 200 | 400 | 9.6 |
| 400 | 400 | 2.8 |
| 200 | 500 | 16.7 |
| 400 | 500 | 8.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Westphalen, H.; Saadati, S.; Bahig, J.; Doan, H.; Shoker, A.; Abdelrasoul, A. Impact of Dialysis Clinical Operating Conditions on Human Serum Protein-Mediated Inflammatory Biomarkers Released in Patients Using Polyarylethersulfone Membranes. J. Compos. Sci. 2022, 6, 226. https://doi.org/10.3390/jcs6080226
Westphalen H, Saadati S, Bahig J, Doan H, Shoker A, Abdelrasoul A. Impact of Dialysis Clinical Operating Conditions on Human Serum Protein-Mediated Inflammatory Biomarkers Released in Patients Using Polyarylethersulfone Membranes. Journal of Composites Science. 2022; 6(8):226. https://doi.org/10.3390/jcs6080226
Chicago/Turabian StyleWestphalen, Heloisa, Shaghayegh Saadati, Jumanah Bahig, Huu Doan, Ahmed Shoker, and Amira Abdelrasoul. 2022. "Impact of Dialysis Clinical Operating Conditions on Human Serum Protein-Mediated Inflammatory Biomarkers Released in Patients Using Polyarylethersulfone Membranes" Journal of Composites Science 6, no. 8: 226. https://doi.org/10.3390/jcs6080226
APA StyleWestphalen, H., Saadati, S., Bahig, J., Doan, H., Shoker, A., & Abdelrasoul, A. (2022). Impact of Dialysis Clinical Operating Conditions on Human Serum Protein-Mediated Inflammatory Biomarkers Released in Patients Using Polyarylethersulfone Membranes. Journal of Composites Science, 6(8), 226. https://doi.org/10.3390/jcs6080226






