Chloramphenicol Loaded Sponges Based on PVA/Nanocellulose Nanocomposites for Topical Wound Delivery
Abstract
1. Introduction
2. Materials and Methods
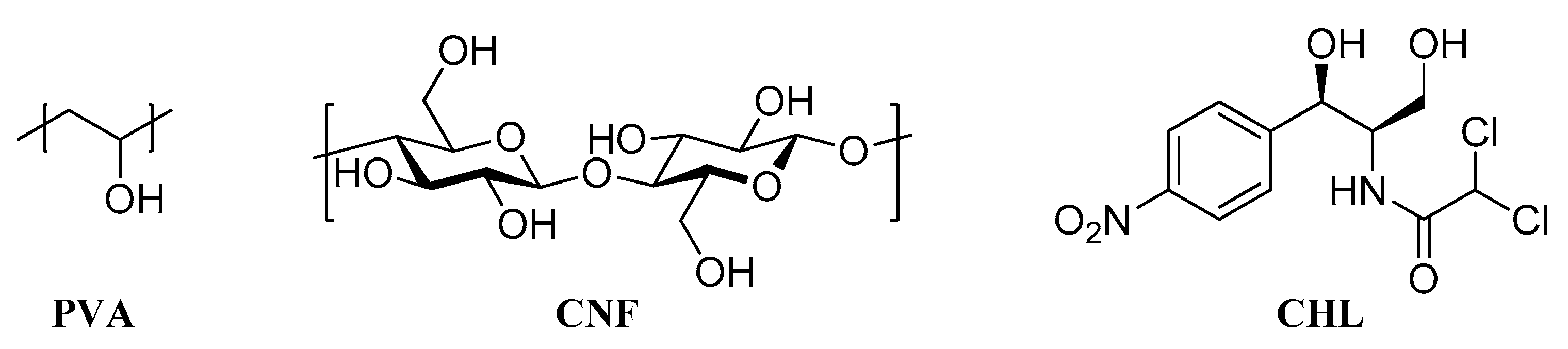
2.1. Materials
2.2. Preparation of PVA/CNF Sponges
2.3. Preparation of CHL Loaded Sponges
2.4. Characterization of the Prepared Sponges
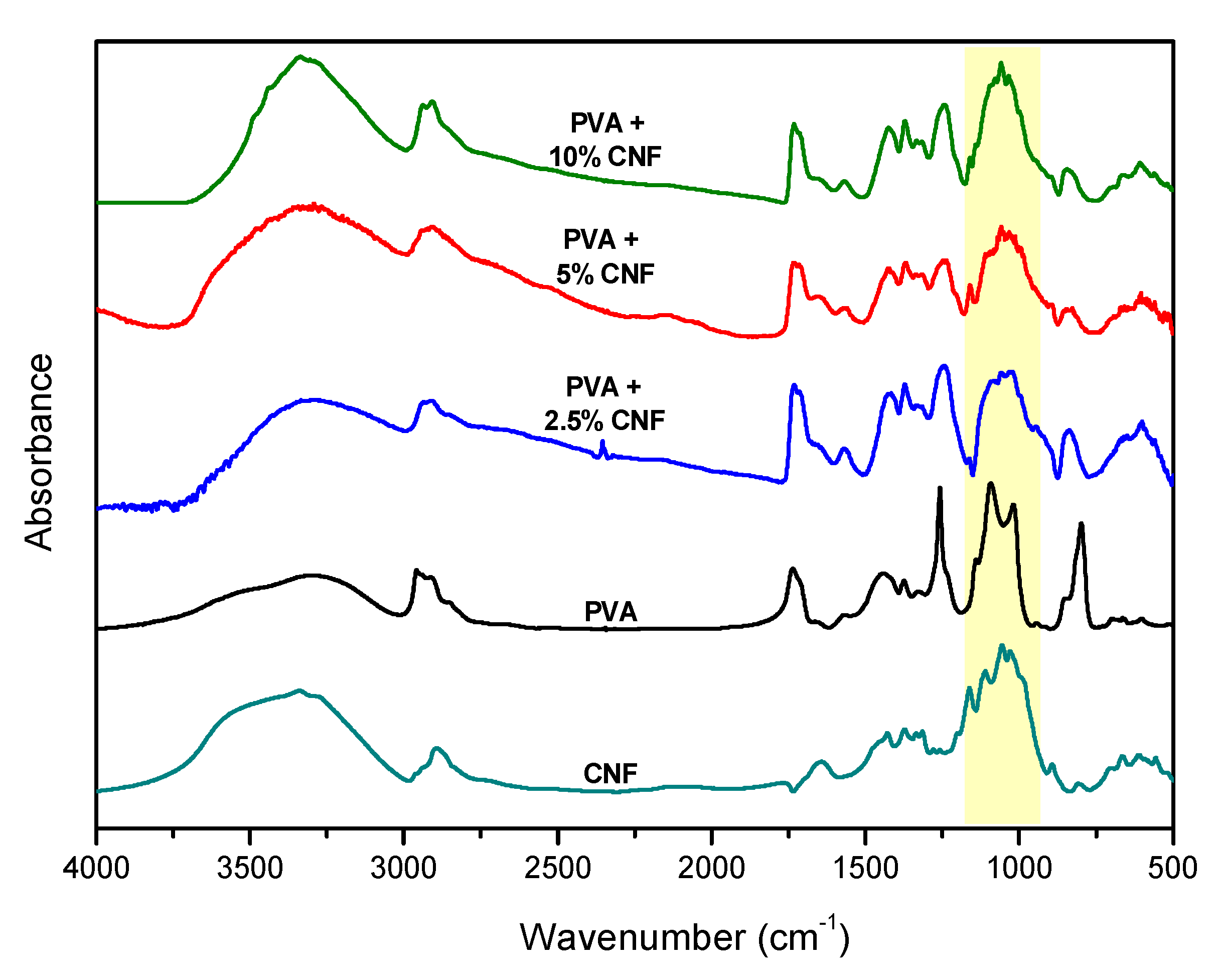
2.4.1. Fourier-Transformed Infrared Spectroscopy (FTIR)
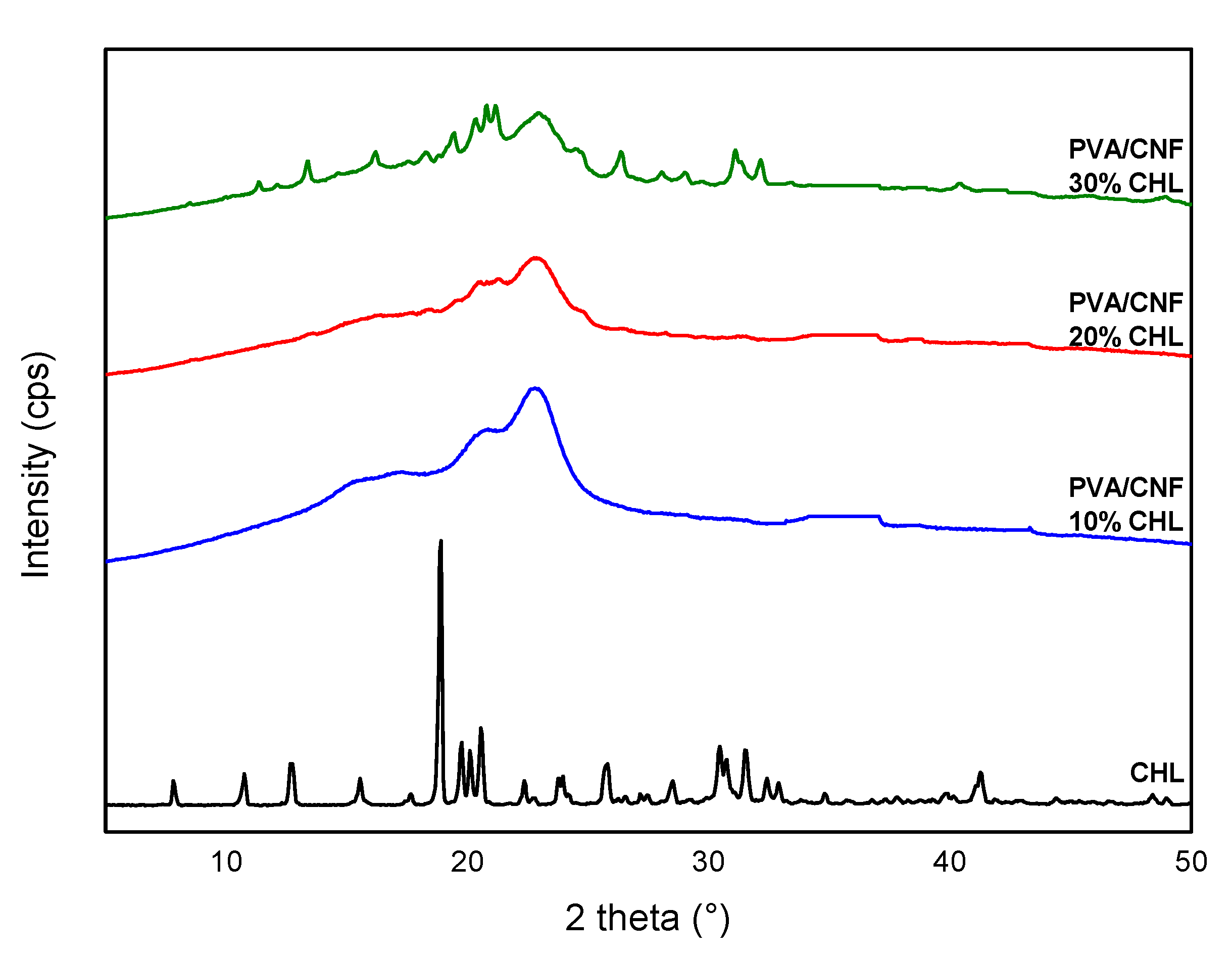
2.4.2. Wide Angle X-ray Scattering
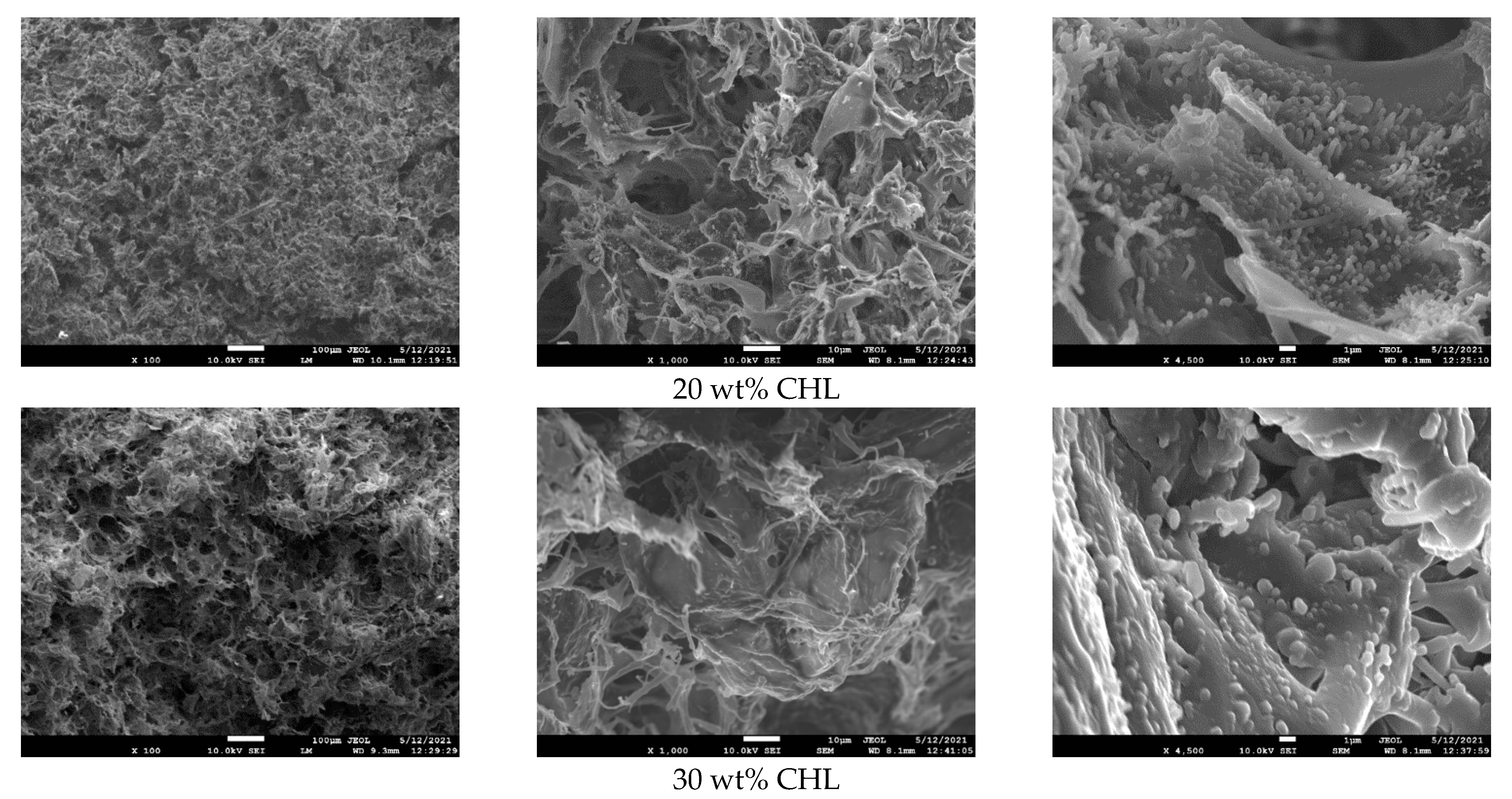
2.4.3. Microscopy
2.4.4. Mechanical Stress Properties
2.4.5. Thermogravimetric Analysis
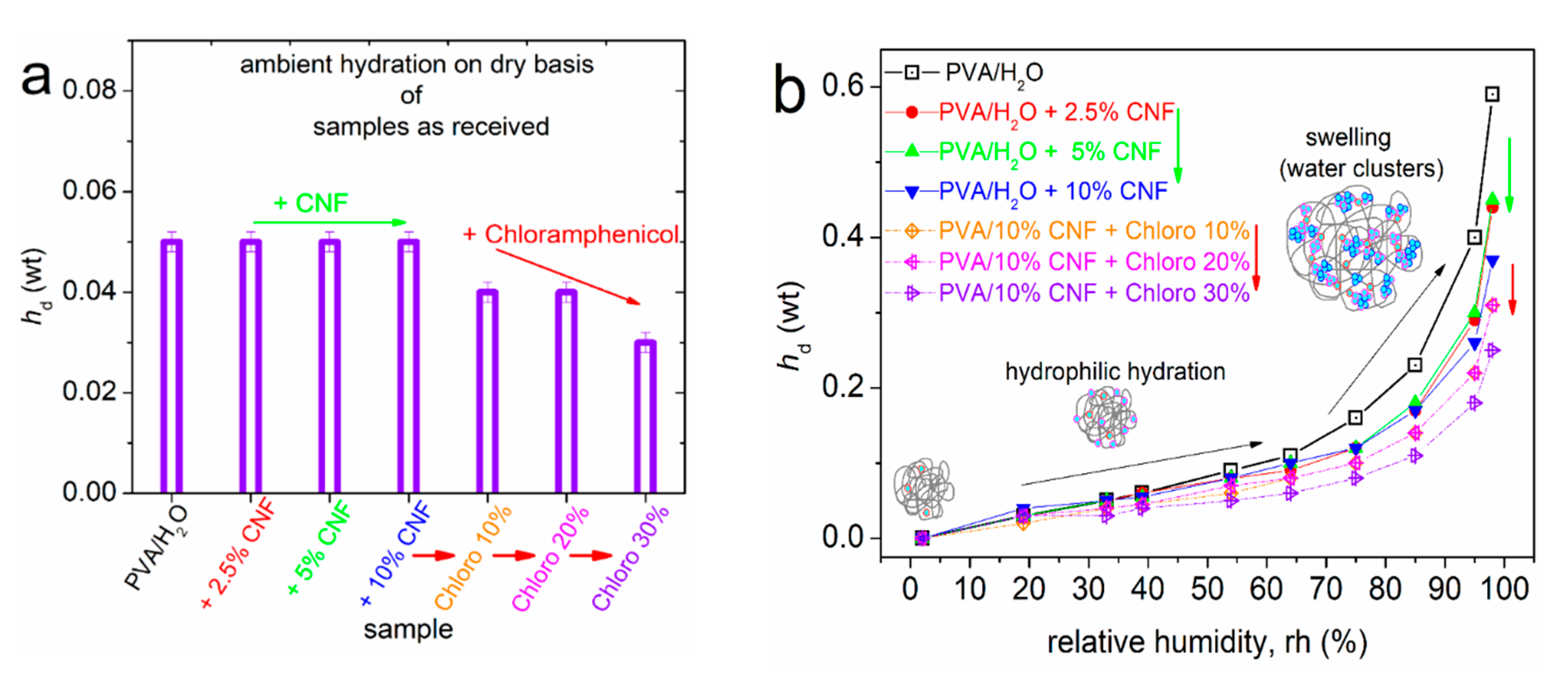
2.4.6. Equilibrium Water Sorption Isotherms (ESI)
2.4.7. In Vitro Dissolution Studies
3. Results and Discussion
3.1. Preparation and Characterization of PVA/CNF Sponges
3.2. Chloramphenicol Loaded PVA/CNF Sponges
3.3. Chloramphenicol Release
3.3.1. In Vitro Release
3.3.2. Modeling of the Release Kinetics
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kus, K.J.B.; Ruiz, E.S. Wound Dressings—A Practical Review. Curr. Dermatol. Rep. 2020, 9, 298–308. [Google Scholar] [CrossRef]
- Hawthorne, B.; Simmons, J.K.; Stuart, B.; Tung, R.; Zamierowski, D.S.; Mellott, A.J. Enhancing wound healing dressing development through interdisciplinary collaboration. J. Biomed. Mater. Res. Part B Appl. Biomater. 2021. (early view). [Google Scholar] [CrossRef]
- Michailidou, G.; Christodoulou, E.; Nanaki, S.; Barmpalexis, P.; Karavas, E.; Vergkizi-Nikolakaki, S.; Bikiaris, D.N. Super-hydrophilic and high strength polymeric foam dressings of modified chitosan blends for topical wound delivery of chloramphenicol. Carbohydr. Polym. 2019, 208, 1–13. [Google Scholar] [CrossRef]
- Jiang, L.; Loo, S.C.J. Intelligent Nanoparticle-Based Dressings for Bacterial Wound Infections. ACS Appl. Bio Mater. 2021, 4, 3849–3862. [Google Scholar] [CrossRef]
- Bal-Öztürk, A.; Özkahraman, B.; Özbaş, Z.; Yaşayan, G.; Tamahkar, E.; Alarçin, E. Advancements and future directions in the antibacterial wound dressings—A review. J. Biomed. Mater. Res. Part B Appl. Biomater. 2021, 109, 703–716. [Google Scholar] [CrossRef]
- Asadi, N.; Pazoki-Toroudi, H.; Del Bakhshayesh, A.R.; Akbarzadeh, A.; Davaran, S.; Annabi, N. Multifunctional hydrogels for wound healing: Special focus on biomacromolecular based hydrogels. Int. J. Biol. Macromol. 2021, 170, 728–750. [Google Scholar] [CrossRef]
- Szczeblinska, J.; Fijalkowski, K.; Kohn, J.; El Fray, M. Antibiotic loaded microspheres as antimicrobial delivery systems for medical applications. Mater. Sci. Eng. C 2017, 77, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Terzopoulou, Z.; Michopoulou, A.; Palamidi, A.; Koliakou, E.; Bikiaris, D. Preparation and Evaluation of Collagen-Based Patches as Curcumin Carriers. Polymers 2020, 12, 2393. [Google Scholar] [CrossRef] [PubMed]
- Nanaki, S.G.; Andrianidou, S.; Barmpalexis, P.; Christodoulou, E.; Bikiaris, D.N. Leflunomide Loaded Chitosan Nanoparticles for the Preparation of Aliphatic Polyester Based Skin Patches. Polymers 2021, 13, 1539. [Google Scholar] [CrossRef]
- Siafaka, P.I.; Zisi, A.P.; Exindari, M.K.; Karantas, I.D.; Bikiaris, D.N. Porous dressings of modified chitosan with poly(2-hydroxyethyl acrylate) for topical wound delivery of levofloxacin. Carbohydr. Polym. 2016, 143, 90–99. [Google Scholar] [CrossRef] [PubMed]
- Ghalei, S.; Asadi, H.; Ghalei, B. Zein nanoparticle-embedded electrospun PVA nanofibers as wound dressing for topical delivery of anti-inflammatory diclofenac. J. Appl. Polym. Sci. 2018, 135, 46643. [Google Scholar] [CrossRef]
- Koumentakou, I.; Terzopoulou, Z.; Michopoulou, A.; Kalafatakis, I.; Theodorakis, K.; Tzetzis, D.; Bikiaris, D. Chitosan dressings containing inorganic additives and levofloxacin as potential wound care products with enhanced hemostatic properties. Int. J. Biol. Macromol. 2020, 162, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Balla, E.; Daniilidis, V.; Karlioti, G.; Kalamas, T.; Stefanidou, M.; Bikiaris, N.D.; Vlachopoulos, A.; Koumentakou, I.; Bikiaris, D.N. Poly(lactic Acid): A Versatile Biobased Polymer for the Future with Multifunctional Properties—From Monomer Synthesis, Polymerization Techniques and Molecular Weight Increase to PLA Applications. Polymers 2021, 13, 1822. [Google Scholar] [CrossRef] [PubMed]
- Mansur, H.S.; Sadahira, C.M.; Souza, A.N.; Mansur, A.A.P. FTIR spectroscopy characterization of poly(vinyl alcohol) hydrogel with different hydrolysis degree and chemically crosslinked with glutaraldehyde. Mater. Sci. Eng. C 2008, 28, 539–548. [Google Scholar] [CrossRef]
- Katopodis, K.; Kapourani, A.; Vardaka, E.; Karagianni, A.; Chorianopoulou, C.; Kontogiannopoulos, K.N.; Bikiaris, D.N.; Kachrimanis, K.; Barmpalexis, P. Partially hydrolyzed polyvinyl alcohol for fusion-based pharmaceutical formulation processes: Evaluation of suitable plasticizers. Int. J. Pharm. 2020, 578, 119121. [Google Scholar] [CrossRef]
- Michailidou, G.; Ainali, N.M.; Xanthopoulou, E.; Nanaki, S.; Kostoglou, M.; Koukaras, E.N.; Bikiaris, D.N. Effect of Poly(vinyl alcohol) on Nanoencapsulation of Budesonide in Chitosan Nanoparticles via Ionic Gelation and Its Improved Bioavailability. Polymers 2020, 12, 1101. [Google Scholar] [CrossRef]
- Feldman, D. Poly(vinyl alcohol) nanocomposites: Recent contributions to engineering and medicine. AIMS Mater. Sci. 2021, 8, 119–129. [Google Scholar] [CrossRef]
- Palamidi, A.; Kapourani, A.; Christodoulou, E.; Klonos, P.A.; Kontogiannopoulos, K.N.; Kyritsis, A.; Bikiaris, D.N.; Barmpalexis, P. Low Molecular Weight Oligomers of Poly(alkylene succinate) Polyesters as Plasticizers in Poly(vinyl alcohol) Based Pharmaceutical Applications. Polymers 2021, 13, 146. [Google Scholar] [CrossRef]
- Trucillo, P.; Di Maio, E. Classification and Production of Polymeric Foams among the Systems for Wound Treatment. Polymers 2021, 13, 1608. [Google Scholar] [CrossRef]
- Lee, S.-Y.; Mohan, D.J.; Kang, I.-A.; Doh, G.-H.; Lee, S.; Han, S.O. Nanocellulose reinforced PVA composite films: Effects of acid treatment and filler loading. Fibers Polym. 2009, 10, 77–82. [Google Scholar] [CrossRef]
- Abitbol, T.; Rivkin, A.; Cao, Y.; Nevo, Y.; Abraham, E.; Ben-Shalom, T.; Lapidot, S.; Shoseyov, O. Nanocellulose, a tiny fiber with huge applications. Curr. Opin. Biotechnol. 2016, 39, 76–88. [Google Scholar] [CrossRef] [PubMed]
- Seddiqi, H.; Oliaei, E.; Honarkar, H.; Jin, J.; Geonzon, L.C.; Bacabac, R.G.; Klein-Nulend, J. Cellulose and its derivatives: Towards biomedical applications. Cellulose 2021, 28, 1893–1931. [Google Scholar] [CrossRef]
- Moritz, S.; Wiegand, C.; Wesarg, F.; Hessler, N.; Müller, F.A.; Kralisch, D.; Hipler, U.-C.; Fischer, D. Active wound dressings based on bacterial nanocellulose as drug delivery system for octenidine. Int. J. Pharm. 2014, 471, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Lin, N.; Dufresne, A. Nanocellulose in biomedicine: Current status and future prospect. Eur. Polym. J. 2014, 59, 302–325. [Google Scholar] [CrossRef]
- Tong, W.Y.; bin Abdullah, A.Y.K.; binti Rozman, N.A.S.; bin Wahid, M.I.A.; Hossain, M.S.; Ring, L.C.; Lazim, Y.; Tan, W.-N. Antimicrobial wound dressing film utilizing cellulose nanocrystal as drug delivery system for curcumin. Cellulose 2018, 25, 631–638. [Google Scholar] [CrossRef]
- Liu, X.; Yang, K.; Chang, M.; Wang, X.; Ren, J. Fabrication of cellulose nanocrystal reinforced nanocomposite hydrogel with self-healing properties. Carbohydr. Polym. 2020, 240, 116289. [Google Scholar] [CrossRef]
- Lu, C.; Wang, C.; Zhang, D.; Wang, J.; Yong, Q.; Chu, F. Ultra-strong hydroxypropyl cellulose/polyvinyl alcohol composite hydrogel by combination of triple-network and mechanical training. Int. J. Biol. Macromol. 2021, 184, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Forti, E.S.; El Awad Azrak, S.M.; Ng, X.Y.; Cho, W.; Schueneman, G.T.; Moon, R.J.; Fox, D.M.; Youngblood, J.P. Mechanical enhancement of cellulose nanofibril (CNF) films through the addition of water-soluble polymers. Cellulose 2021, 28, 6449–6465. [Google Scholar] [CrossRef]
- Song, S.; Liu, Z.; Abubaker, M.A.; Ding, L.; Zhang, J.; Yang, S.; Fan, Z. Antibacterial polyvinyl alcohol/bacterial cellulose/nano-silver hydrogels that effectively promote wound healing. Mater. Sci. Eng. C 2021, 126, 112171. [Google Scholar] [CrossRef]
- Zimmermann, T.; Pöhler, E.; Schwaller, P. Mechanical and Morphological Properties of Cellulose Fibril Reinforced Nanocomposites. Adv. Eng. Mater. 2005, 7, 1156–1161. [Google Scholar] [CrossRef]
- Sabu, T.; Raghvendra, K.M.; Abdullah, M.A. (Eds.) Sustainable Polymer Composites and Nanocomposites; Springer: Cham, Switzerland, 2019; ISBN 978-3-030-05398-7. [Google Scholar]
- Todoran, N.; Ciurba, A.; Rédai, E.; Ion, V.; Lazăr, L.; Sipos, E. Limitations when use chloramphenicol-bcyclodextrins complexes in ophtalmic solutions buffered with boric acid/borax system. Acta Med. Marisiensis 2014, 60, 269–274. [Google Scholar] [CrossRef][Green Version]
- Karava, A.; Lazaridou, M.; Nanaki, S.; Michailidou, G.; Christodoulou, E.; Kostoglou, M.; Iatrou, H.; Bikiaris, D.N. Chitosan Derivatives with Mucoadhesive and Antimicrobial Properties for Simultaneous Nanoencapsulation and Extended Ocular Release Formulations of Dexamethasone and Chloramphenicol Drugs. Pharmaceutics 2020, 12, 594. [Google Scholar] [CrossRef] [PubMed]
- Rihawy, M.S.; Alzier, A.; Allaf, A.W. Investigation of chloramphenicol release from PVA/CMC/HEA hydrogel using ion beam analysis, UV and FTIR techniques. Appl. Radiat. Isot. 2019, 153, 108806. [Google Scholar] [CrossRef] [PubMed]
- Pissis, P.; Kyritsis, A. Hydration studies in polymer hydrogels. J. Polym. Sci. Part B Polym. Phys. 2013, 51, 159–175. [Google Scholar] [CrossRef]
- Klonos, P.; Pissis, P.; Kyritsis, A. Effects of Hydration/Dehydration on Interfacial Polymer Fraction and Dynamics in Nanocomposites Based on Metal–Oxides and Physically Adsorbed Polymer. J. Phys. Chem. C 2017, 121, 19428–19441. [Google Scholar] [CrossRef]
- Greenspan, L. Humidity fixed points of binary saturated aqueous solutions. J. Res. Natl. Bur. Stand. Sect. A Phys. Chem. 1977, 81A, 89. [Google Scholar] [CrossRef]
- Wang, Z.; Zhao, S.; Hong, L.; Huang, J. Preparation and Properties of Silver-Based Cellulose/Polyvinyl Alcohol Antibacterial Materials. J. Inorg. Organomet. Polym. Mater. 2020, 30, 4382–4393. [Google Scholar] [CrossRef]
- Garside, P.; Wyeth, P. Identification of Cellulosic Fibres by FTIR Spectroscopy—Thread and Single Fibre Analysis by Attenuated Total Reflectance. Stud. Conserv. 2003, 48, 269–275. [Google Scholar] [CrossRef]
- Yang, Y.P.; Zhang, Y.; Lang, Y.X.; Yu, M.H. Structural ATR-IR analysis of cellulose fibers prepared from a NaOH complex aqueous solution. IOP Conf. Ser. Mater. Sci. Eng. 2017, 213, 012039. [Google Scholar] [CrossRef]
- Jayaramudu, T.; Ko, H.-U.; Kim, H.C.; Kim, J.W.; Muthoka, R.M.; Kim, J. Electroactive Hydrogels Made with Polyvinyl Alcohol/Cellulose Nanocrystals. Materials 2018, 11, 1615. [Google Scholar] [CrossRef]
- Ching, Y.C.; Rahman, A.; Ching, K.Y.; Sukiman, N.L.; Chuah, C.H. Preparation and characterization of polyvinyl alcohol-based composite reinforced with nanocellulose and nanosilica. BioResources 2015, 10, 3364–3377. [Google Scholar] [CrossRef]
- Gong, J.; Li, J.; Xu, J.; Xiang, Z.; Mo, L. Research on cellulose nanocrystals produced from cellulose sources with various polymorphs. RSC Adv. 2017, 7, 33486–33493. [Google Scholar] [CrossRef]
- Aguayo, M.G.; Fernández Pérez, A.; Reyes, G.; Oviedo, C.; Gacitúa, W.; Gonzalez, R.; Uyarte, O. Isolation and Characterization of Cellulose Nanocrystals from Rejected Fibers Originated in the Kraft Pulping Process. Polymers 2018, 10, 1145. [Google Scholar] [CrossRef]
- Bary, E.M.A.; Fekri, A.; Soliman, Y.A.; Harmal, A.N. Novel superabsorbent membranes made of PVA and Ziziphus spina-christi cellulose for agricultural and horticultural applications. New J. Chem. 2017, 41, 9688–9700. [Google Scholar] [CrossRef]
- Ashby, M.F.; Medalist, R.F.M. The mechanical properties of cellular solids. Metall. Trans. A 1983, 14, 1755–1769. [Google Scholar] [CrossRef]
- Song, T.; Tanpichai, S.; Oksman, K. Cross-linked polyvinyl alcohol (PVA) foams reinforced with cellulose nanocrystals (CNCs). Cellulose 2016, 23, 1925–1938. [Google Scholar] [CrossRef]
- Zuorro, A.; Fidaleo, M.; Lavecchia, R. Solubility enhancement and antibacterial activity of chloramphenicol included in modified β-cyclodextrins. Bull. Korean Chem. Soc. 2010, 31, 3460–3462. [Google Scholar] [CrossRef][Green Version]
- Ainali, N.M.; Xanthopoulou, E.; Michailidou, G.; Zamboulis, A.; Bikiaris, D.N. Microencapsulation of Fluticasone Propionate and Salmeterol Xinafoate in Modified Chitosan Microparticles for Release Optimization. Molecules 2020, 25, 3888. [Google Scholar] [CrossRef]
- Stathopoulos, A.; Klonos, P.; Kyritsis, A.; Pissis, P.; Christodoulides, C.; Hernández, J.C.R.; Pradas, M.M.; Ribelles, J.L.G. Water sorption and polymer dynamics in hybrid poly(2-hydroxyethyl-co-ethyl acrylate)/silica hydrogels. Eur. Polym. J. 2010, 46, 101–111. [Google Scholar] [CrossRef]
- Abdollahi, M.; Alboofetileh, M.; Behrooz, R.; Rezaei, M.; Miraki, R. Reducing water sensitivity of alginate bio-nanocomposite film using cellulose nanoparticles. Int. J. Biol. Macromol. 2013, 54, 166–173. [Google Scholar] [CrossRef]
- Gomaa, M.M.; Hugenschmidt, C.; Dickmann, M.; Abdel-Hady, E.E.; Mohamed, H.F.M.; Abdel-Hamed, M.O. Crosslinked PVA/SSA proton exchange membranes: Correlation between physiochemical properties and free volume determined by positron annihilation spectroscopy. Phys. Chem. Chem. Phys. 2018, 20, 28287–28299. [Google Scholar] [CrossRef]
- Frunza, M.; Lisa, G.; Popa, M.I.; Miron, N.D.; Nistor, D.I. Thermogravimetric analysis of layered double hydroxides with chloramphenicol and salicylate in the interlayer space. J. Therm. Anal. Calorim. 2008, 93, 373–379. [Google Scholar] [CrossRef]
- Macêdo, R.O.; Aragão, C.F.S.; do Nascimento, T.G.; Macêdo, A.M.C. Application of Thermogravimetry in the Quality Control of Chloramphenicol Tablets. J. Therm. Anal. Calorim. 1999, 56, 1323–1327. [Google Scholar] [CrossRef]
- Grassi, M.; Grassi, G. Application of mathematical modeling in sustained release delivery systems. Expert Opin. Drug Deliv. 2014, 11, 1299–1321. [Google Scholar] [CrossRef]
- Pappa, C.; Nanaki, S.; Giliopoulos, D.; Triantafyllidis, K.; Kostoglou, M.; Avgeropoulos, A.; Bikiaris, D. Nanostructured Composites of Sodium Montmorillonite Clay and PEO Used in Dissolution Improvement of Aprepitant Drug by Melt Mixing. Appl. Sci. 2018, 8, 786. [Google Scholar] [CrossRef]
- Hattori, Y.; Haruna, Y.; Otsuka, M. Dissolution process analysis using model-free Noyes–Whitney integral equation. Colloids Surf. B Biointerfaces 2013, 102, 227–231. [Google Scholar] [CrossRef]
- Setapa, A.; Ahmad, N.; Mohd Mahali, S.; Mohd Amin, M.C. Mathematical Model for Estimating Parameters of Swelling Drug Delivery Devices in a Two-Phase Release. Polymers 2020, 12, 2921. [Google Scholar] [CrossRef]
- Lazaridou, M.; Nanaki, S.; Zamboulis, A.; Papoulia, C.; Chrissafis, K.; Klonos, P.A.; Kyritsis, A.; Vergkizi-Nikolakaki, S.; Kostoglou, M.; Bikiaris, D.N. Super absorbent chitosan-based hydrogel sponges as carriers for caspofungin antifungal drug. Int. J. Pharm. 2021, 606, 120925. [Google Scholar] [CrossRef]
- Crank, J. The Mathematics of Diffusion, 2nd ed.; Oxford University Press: New York, NY, USA, 1979. [Google Scholar]










| No | Sample | hd,amb (wt) | hd,rh2 (wt) | hd,rh19 (wt) | hd,rh33 (wt) | hd,rh39 (wt) | hd,rh54 (wt) | hd,rh64 (wt) | hd,rh75 (wt) | hd,rh85 (wt) | hd,rh95 (wt) | hd,rh98 (wt) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | PVA/H2O 0% CNF | 0.05 | 0 | 0.03 | 0.05 | 0.06 | 0.09 | 0.11 | 0.16 | 0.23 | 0.40 | 0.59 |
| 2 | PVA/H2O 2.5% CNF | 0.05 | 0 | 0.03 | 0.05 | 0.06 | 0.08 | 0.09 | 0.12 | 0.17 | 0.29 | 0.44 |
| 3 | PVA/H2O 5% CNF | 0.05 | 0 | 0.03 | 0.05 | 0.06 | 0.08 | 0.10 | 0.12 | 0.18 | 0.30 | 0.45 |
| 4 | PVA/H2O 10% CNF | 0.05 | 0 | 0.04 | 0.05 | 0.06 | 0.08 | 0.10 | 0.12 | 0.17 | 0.26 | 0.37 |
| 5 | PVA 10% CNF + Chloro 10% | 0.04 | 0 | 0.02 | 0.04 | 0.05 | 0.06 | 0.08 | 0.10 | 0.14 | 0.22 | 0.31 |
| 6 | PVA 10% CNF + Chloro 20% | 0.04 | 0 | 0.03 | 0.04 | 0.05 | 0.07 | 0.08 | 0.10 | 0.14 | 0.22 | 0.31 |
| 7 | PVA 10% CNF + Chloro 30% | 0.03 | 0 | 0.03 | 0.03 | 0.04 | 0.05 | 0.06 | 0.08 | 0.11 | 0.18 | 0.25 |
| Sample | Drug Loading (%) | Entrapment Efficiency (%) |
|---|---|---|
| PVA/10% CNF + CHL 10 wt % | 9.81 ± 0.31 | 98.10 ± 1.09 |
| PVA/10% CNF + CHL 20 wt % | 18.76 ± 0.94 | 93.80 ± 1.84 |
| PVA/10% CNF + CHL 30 wt % | 26.81 ± 1.67 | 89.37 ± 2.03 |
| φ | D1 (m2/s) | D2 (m2/s) | |
|---|---|---|---|
| PVA/CNF + CHL 10 wt % | 0.35 | 1.17 × 10−7 | 1.73ˑ× 10−9 |
| PVA/CNF + CHL 20 wt % | 0.68 | 8.27ˑ× 10−8 | 6.48ˑ× 10−9 |
| PVA/CNF + CHL 30 wt % | 0.82 | 4.35ˑ× 10−8 | 7.56ˑ× 10−9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balla, E.D.; Bikiaris, N.D.; Nanaki, S.G.; Papoulia, C.; Chrissafis, K.; Klonos, P.A.; Kyritsis, A.; Kostoglou, M.; Zamboulis, A.; Papageorgiou, G.Z. Chloramphenicol Loaded Sponges Based on PVA/Nanocellulose Nanocomposites for Topical Wound Delivery. J. Compos. Sci. 2021, 5, 208. https://doi.org/10.3390/jcs5080208
Balla ED, Bikiaris ND, Nanaki SG, Papoulia C, Chrissafis K, Klonos PA, Kyritsis A, Kostoglou M, Zamboulis A, Papageorgiou GZ. Chloramphenicol Loaded Sponges Based on PVA/Nanocellulose Nanocomposites for Topical Wound Delivery. Journal of Composites Science. 2021; 5(8):208. https://doi.org/10.3390/jcs5080208
Chicago/Turabian StyleBalla, Evangelia D., Nikolaos D. Bikiaris, Stavroula G. Nanaki, Chrysanthi Papoulia, Konstantinos Chrissafis, Panagiotis A. Klonos, Apostolos Kyritsis, Margaritis Kostoglou, Alexandra Zamboulis, and George Z. Papageorgiou. 2021. "Chloramphenicol Loaded Sponges Based on PVA/Nanocellulose Nanocomposites for Topical Wound Delivery" Journal of Composites Science 5, no. 8: 208. https://doi.org/10.3390/jcs5080208
APA StyleBalla, E. D., Bikiaris, N. D., Nanaki, S. G., Papoulia, C., Chrissafis, K., Klonos, P. A., Kyritsis, A., Kostoglou, M., Zamboulis, A., & Papageorgiou, G. Z. (2021). Chloramphenicol Loaded Sponges Based on PVA/Nanocellulose Nanocomposites for Topical Wound Delivery. Journal of Composites Science, 5(8), 208. https://doi.org/10.3390/jcs5080208












