Abstract
Introduction: The purpose of this study was to qualitatively explore the experiences of chronic dizziness diagnosis and management within the health care system. Methods: This qualitative phenomenological study used focus groups to interview a convenience sample of individuals with chronic dizziness (n = 13) and vestibular physical therapists (n = 15). Focus group data were systematically analyzed using a descriptive coding process. Results: Two major themes emerged from interviews with individuals with dizziness: (1.) complexities navigating the health system and (2.) loss of self-identity. Three major themes emerged from interviews with vestibular physical therapists: (1.) patients have a complex, multi-factorial presentation, (2.) importance of the multidisciplinary care team, and (3.) behavior influences outcomes. Individuals with chronic dizziness identified many challenges in effectively navigating the health system and receiving an effective diagnosis and management, including the patient–provider relationship, with negative impacts on quality of life. Vestibular physical therapist data concurred and validated these experiences. Conclusion: Given the complex, multi-factorial nature of dizziness, increased use of the biopsychosocial model in a multidisciplinary dizziness clinic may inform a more holistic approach for this patient population and improve future outcomes for individuals with chronic dizziness.
1. Introduction
Symptoms of dizziness are a common reason for seeking medical treatment, resulting in approximately 20.6 million ambulatory care visits in the United States between 2013 and 2015 [1]. Those who experience dizziness have been noted to have a high burden of disease, including decreased productivity and lost work time [2,3]. Chronic dizziness can last for months to years, and providing care for those with chronic dizziness presents a challenge for clinicians. Often, individuals with chronic dizziness have less favorable functional outcomes [4] and a lower quality of life [5]. Individuals with recurrent vestibular disorders are estimated to cost the health care system between USD 8000 and 11,000 more per year than those without dizziness, with much of this money being spent on diagnostic testing and imaging, highlighting the economic impact of this problem [6].
Dizziness may often become chronic in nature due to difficulty obtaining a clear diagnosis and implementing effective treatment, which can lead to functional and participation restrictions for those it impacts [7]. Etiologies of dizziness include both neurological and cardiovascular system involvement, making the differential diagnosis process complex. In a systematic review examining etiologies of dizziness, 13 of 14 studies included a category called “no specific diagnosis possible” and in 1 study, up to 80% of the cases were assigned to that category [8]. Individuals with postural orthostatic tachycardia syndrome (POTS), a type of autonomic disorder that leads to symptoms of light-headedness, saw an average of seven physicians prior to receiving a diagnosis [9]. Some types of dizziness that are vestibular in origin present with a clear pattern of symptoms that lead to easier diagnosis and treatment, such as benign paroxysmal positional vertigo. Other episodic disorders such as Meniere’s disease or vestibular migraine are more difficult to diagnose. One cross-sectional survey that examined the epidemiology of vestibular migraine reported that only 10% of individuals who met the description for vestibular migraine were diagnosed with this disorder and were more often provided with other diagnoses, highlighting the issue of a missed diagnosis or misdiagnosis [10]. This problem is further compounded by individuals often seeking care from a primary care physician first, who is often without specific neuro-otological expertise [11]. Lastly, patient management and diagnosis is also thought to be made more difficult by the large variety of individualized descriptions of dizziness [11]. For example, individuals will describe their dizziness using a myriad of symptoms, such as light-headedness, disequilibrium, or spinning.
Living with chronic dizziness is a burden for those that experience it, and the literature acknowledges the diagnostic challenges and the resulting functional implications that those with chronic dizziness experience [7]. However, little has been investigated about why these challenges exist and what could be changed to improve this. This study aims to investigate that gap using a qualitative lens. Qualitative research helps explore the nature of a phenomena and explore reasons behind why something is observed [12]. Results can be used to identify facilitators or barriers to receiving health care services.
Because experiences with dizziness diagnosis and management occur between patients and health care providers, exploring insights from both parties may better inform the complexities of this situation. Qualitative research involving both patient and provider experiences has been explored more robustly in the chronic pain population [13,14] but a large gap in the literature exists with regard to those who are chronically dizzy. Exploring the perspectives of both patients and health care providers is important as it will help to identify both common and unique challenges in holistically achieving successful functional outcomes for the chronically dizzy population. It may also aid in the development of tailored solutions to better address the problems faced by this population. This study aims to address that gap. The purpose of this study was to qualitatively explore the experiences of individuals with chronic dizziness and the health care providers for individuals with chronic dizziness during the diagnostic and management process in the outpatient ambulatory care sector of the health care system.
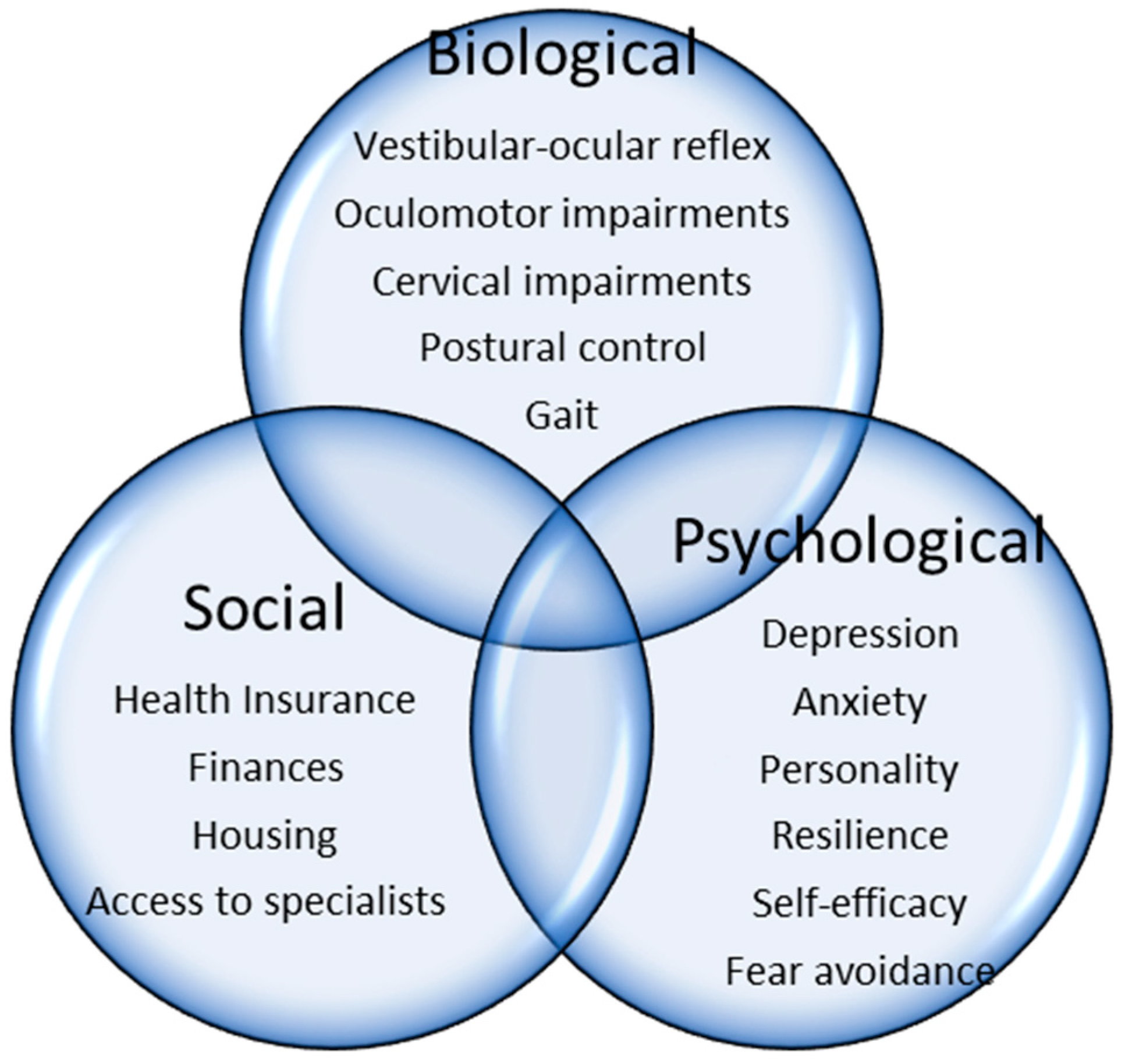
Individuals with chronic dizziness often experience complex psychosocial interactions around their diagnostic and management process [15]. Because the literature acknowledges that attention to personal and contextual factors is fundamental to effective health care outcomes [16], George Engel’s biopsychosocial model may be helpful to use as a conceptual framework [17]. The biopsychosocial model emphasizes the integration and importance of the biomedical aspects of care with the psychological and social dimensions of care [17]. It stresses the bidirectional and reciprocal impacts of these constructs, the importance of the patient–provider relationship to maximize outcomes, and the need for a multidisciplinary care team to holistically address all patient needs [18]. The model is widely adopted and utilized with the chronic pain population, as it emphasizes the importance of chronic pain as an individualized and dynamic experience of the interaction between biomedical, psychological, and social factors [19]. This model may be useful to understand patient experiences and outcomes in the chronically dizzy population as well. The biopsychosocial model will be used in the current study to highlight the role that social and psychological aspects of care have on the biomedical disorder of chronic dizziness, explore the impact of the patient–provider relationship, and investigate the utility of the multidisciplinary care team. A conceptual model of the biopsychosocial model applied to chronic dizziness is provided (Figure 1).
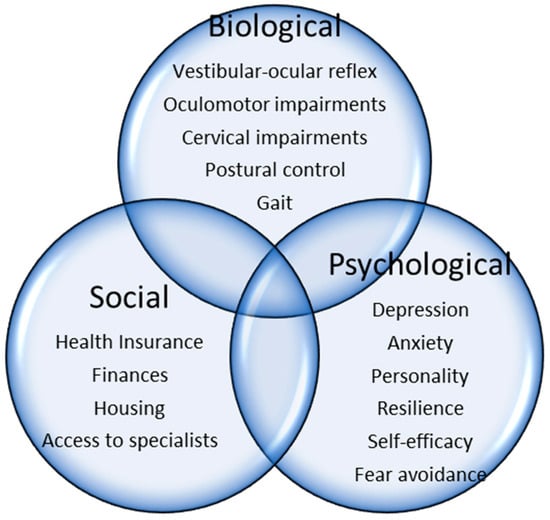
Figure 1.
Biopsychosocial model of chronic dizziness.
2. Materials and Methods
This qualitative study used a phenomenological approach. Phenomenology is an approach that looks to gather information about an individual’s lived experiences within a phenomenon and how they feel about it. Phenomenology describes these experiences from the point of view of the participants and from a dual lens of the researcher’s interpretation of the participants’ experience [20]. While phenomenology typically involves 1:1 interviews, and not focus group interviews, [21] the researchers opted to use focus group interviews to generate rich discussions and diverse viewpoints, thereby providing deeper insights into the phenomenon as well as to open up new perspectives [22]. However, to ensure that participants were able to share their nuanced experience of the phenomenon under study, focus groups were limited to no more than 5 participants.
Virtual focus groups of 3–5 persons were conducted using a semi-structured interview protocol (Appendix A and Appendix B). Protocols were developed based on prior semi-structured interviews of individuals with chronic dizziness [23] and physical therapist experiences managing other chronic conditions [24]. Vestibular physical therapists and individuals with chronic dizziness participated separately in the focus groups. Datasets were treated as separate and analyzed separately. The Mass General Brigham Institutional Review Board approved the study prior to data collection (Protocol # 2022P003392). All participants provided verbal informed consent prior to beginning the interview.
A convenience sample of 13 individuals with chronic dizziness and 15 physical therapists with vestibular expertise participated in the study. The inclusion criteria for individuals with chronic dizziness included the following: >18 years of age and experiencing dizziness of greater than 3 months of duration since chronic dizziness is defined by a 3-month duration in recent clinical practice guidelines [25]. Specific vestibular diagnostic criteria were not required to participate and therefore there were no exclusion criteria. Individuals with dizziness were recruited regionally and nationally via online recruitment tools. Participants known to the first author from clinical care of dizziness were also formally recruited using IRB-approved flyers and fact sheets. Vestibular physical therapists were recruited nationally via the American Physical Therapy Association’s Vestibular Special Interest Group Research Collaboration list as well as locally via convenience sampling and snowball sampling.
One researcher (EC) conducted all interviews virtually on Zoom. Interviews were in English and lasted approximately 45–60 min. Focus groups were conducted separately for individuals with chronic dizziness and the physical therapists, and four focus group interviews were conducted for both groups. During the interview process, the questions were refined using field notes generated based on the participants’ responses. Data collection proceeded until data saturation was achieved; when no new data were collected, redundancy was achieved [26]. Data were audio-recorded and then transcribed using otter.ai. All transcripts were read, deidentified, and checked for accuracy prior to analysis.
Transcripts were coded using NVivo 2020 [27], a software for qualitative analysis. Focus group data were systematically analyzed using a descriptive coding process [28]. During the first cycle coding, researchers independently performed line-by-line coding on one focus group transcript with individuals with dizziness, chunking data into descriptive codes. After this initial coding, both researchers discussed the codes to reach consensus. This process resulted in an initial code book. During second cycle coding, the primary author (EC) then used the initial code book to code the remaining transcripts while allowing for emergent coding. When needed, new codes were added during the analysis of the remaining transcripts. The coding results were discussed, and the researchers identified themes and subthemes based on coding frequencies both within and across interviews. The themes were reviewed and refined to name and define their conceptual meaning. This process was then repeated for the interview data from the physical therapist participants.
Researcher triangulation, where researchers coded data separately and then met multiple times to achieve consensus, was utilized to increase trustworthiness of results. Thick descriptions were also used to increase the confirmability [29]. The codes and themes developed are shared in Appendix C.
3. Results
3.1. Themes of Individuals with Chronic Dizziness
The 13 participants with chronic dizziness were predominantly female (92%) and had variable self-reported etiologies of dizziness (Table 1). The qualitative analysis for participants with chronic dizziness revealed two themes: (1.) complexities navigating the health system and (2.) loss of self-identity.

Table 1.
Demographics of participants with chronic dizziness.
3.1.1. Complexities Navigating the Health System
Individuals with chronic dizziness reported significant difficulties navigating the health system and achieving a successful outcome. These difficulties were multi-factorial in nature and involved both interactions with medical providers as well as health insurance limitations. Consistent with the idea that dizziness involves complicated differential diagnosis, individuals reported undergoing many types of diagnostic tests and seeing many different medical providers, sometimes without successfully receiving a diagnosis or learning about the etiology of their dizziness. Participants reported that a lack of a clear diagnostic label as well as the chronicity of their dizziness symptoms negatively impacted their relationship with their health care providers. One commented: “The one thing for me sometimes I do feel like I’m overlooked a bit or, like not treated the same, because I’ve gone back to PT several times… like I don’t get as deep a dive” (Participant 5). Another participant reported similar experiences: “I do feel like physicians kind of throw their hands in the air—especially my primary care physician, because she’s the epicenter, and I need referrals from her” (Participant 6).
Participants reported feeling varying levels of support from health care practitioners and at times noted feelings of dismissal and a power dynamic. The most common experience of dismissal for participants was that they were told ongoing symptoms of dizziness were primarily related to mental health problems. “It was a long time of people just, really doctors just saying, there’s nothing wrong with you. It’s anxiety and depression, which is very, very frustrating, very upsetting” (Participant 5). Participants reported experiencing a range of emotions in situations when a medical hierarchy emerged, as highlighted by Participant 1 in this quote, “I know I stopped seeing the PM&R (Physical medicine and rehabilitation) doctor after my initial concussion because I felt like he was talking down to me and I felt like I was crying every single time I went there”.
Participants shared a perception of varying levels of diagnostic and technical skill among their health care providers. This perception appeared to vary based on areas of the country in which individuals lived and their proximity to urban areas with easier access to academic medical centers with specialists. Participants were grateful for those providers with specific neuro-otological and vestibular expertise who were perceived to provide effective interventions.
I finally went back to the doctor who spun me around in the chair and all that stuff. And she was like ‘Your symptoms sound like PPPD.’ She goes ‘There’s nothing you can test for, but I bet that’s what you have’. And she put me on Zoloft and it helped tremendously. Tremendously (Participant 11).
Participants noted that along with challenging provider interactions, limitations in health insurance created stress and financial hardship. Participants also noted that the quality of providers and duration of care varied based on health insurance, which made managing their chronic dizziness more difficult.
So, and then you get this huge bill for the hospital fee on top of their office visit without any results or no ongoing contact… and that was very frustrating. And then insurance, just incredibly frustrated with the health care system in general in terms of how illness and long-term care needs are met or not met is really the point here. Especially when you don’t fit neatly into a category (Participant 4).
3.1.2. Loss of Self-Identity
Many participants identified how having chronic dizziness led to loss of self-identity due to difficulty performing everyday functional activities and participating in their societal roles. Driving and performing shopping tasks in visually stimulating environments were consistently identified as challenging for many participants. Many individuals reported making modifications to their everyday functional tasks so that they could still complete them, often moving more slowly and cautiously. The need to think and plan before moving instead of responding in an unconstrained way was felt to be tiresome and limiting. One commented, “I can’t bend over and pick things up without planning it, thinking about it ahead of time. You know, I can’t be spontaneous. I can’t ride a bike; I can’t run you know…” (Participant 4). Participants reported that these adjustments were a shift from their previous identity, and that change in self-identity was an additional challenge beyond the functional modifications themselves.
Lack of participation in social roles such as employment, schooling, and social engagements due to chronic dizziness was identified as particularly detrimental as these were essential elements of participant identity. Participants also noted how chronic dizziness was limiting in achieving or maintaining health and wellness goals such as weight loss or fitness.
Mechanisms that acted as catalysts for lack of participation were probed and the unpredictability of dizziness symptoms emerged consistently.
And for me, that’s the most frustrating piece of the whole puzzle that’s yet to be solved. And I can’t predict when it’s going to happen. I don’t know how to stop it. And then when it happens, I really don’t know how to make it better. I just sort of deal with it until it goes way (Participant 6).
Participants identified that because symptoms of chronic dizziness vacillated, and it was difficult to always identify causal factors, this led to concerns that symptoms may come on suddenly while they were out in public, which could be a potentially frightening or embarrassing experience. Some participants noted that these concerns led to more social isolation as they avoided activities that they feared would bring on dizziness. Participants also noted that because it was often difficult to obtain a clear diagnosis for their symptoms, this led to further self-isolation, as it was difficult to explain their symptoms to others when they themselves did not understand the origin of their dizziness.
And then I didn’t really go out because the dizziness made me feel so sick. I go out with my husband because he knew about it. But with friends and stuff even though you can’t really explain it either because you can’t see it. Or like, you know, how bad can it be? Because you’re still talking normal, look normal, but you’re dying inside, right? People can’t see it. So, you can’t really explain it. So then when it starts happening, you don’t know what to talk about. It’s just easier to avoid the whole situation (Participant 11).
3.2. Themes of Vestibular Physical Therapists
The 15 physical therapist participants were predominantly female (93%), were all practicing in an outpatient setting, and reported variable durations of time in clinical practice ranging from 4 to 35 years (Table 2). The qualitative analysis of physical therapist participants revealed three themes: (1) patients have a complex, multi-factorial presentation, (2) importance of the multidisciplinary care team, and (3) behavior influences outcomes.

Table 2.
Demographics of physical therapist participants.
3.2.1. Complex, Multi-Factorial Presentation
Physical therapist participants described that those with chronic dizziness often had multiple diagnoses involving many body systems and underlying contextual factors that impacted their dizziness. Many physical therapists discussed the importance of carefully assessing multiple body systems, including the cervical spine, the cardiopulmonary system, and the oculomotor system to best meet the patient’s needs and address all underlying impairments.
I always assess the neck a lot as well… because of dizziness with head motion they are fearful to move their heads. I’m always doing not just vestibular but also talking to them about moving their head, about orthopedics. I feel like for some of the people I see they have a secondary cervicogenic dizziness and secondary weakness in their upper back. So, I’m trying to be holistic in how I look at the patient (Participant 3).
Acknowledging the importance of psychosocial factors and the role of mental health was noted as critical for patient success. Physical therapist participants appreciated the complex interconnectedness between anxiety and dizziness. One commented: “the overlap of whether the dizziness is increasing people’s anxiety, or whether they already had premorbid anxiety, if that’s a factor in their persisting symptoms, and they aren’t getting it addressed, then that can be a barrier to PT” (Participant 12). Many participants felt confident initiating this conversation with their patients and used a variety of approaches to do this, including discussing the relevant medical literature, referring to counseling services, or assistance finding a mental health provider.
Participants felt uniquely positioned to identify and address the complex, multi-factorial nature of chronic dizziness due to their higher frequency and duration of interactions with patients. The increased time spent one-on-one with patients provided an opportunity for rapport and trust building, allowing patients to share more subtle symptoms that prompted participants to examine other previously overlooked body systems that may be contributing to chronic dizziness. The rapport and trust developed was perceived to allow patients to share emotions that suggested the need for mental health support.
We’ve developed such a relationship with patients because we spend more time with them, I think than most health care providers. And once that relationship’s there and that trust is there, they start to talk. And so then you start to realize, oh, there’s a history here, or there’s a background of PTSD… And that could be why we’re in this chronic dizziness stage (Participant 4).
3.2.2. Importance of the Multidisciplinary Care Team
Physical therapist participants emphasized the importance of the multidisciplinary care team to obtain successful outcomes for individuals with dizziness due to their complex nature. Those participants that found physicians and mental health providers they could routinely collaborate with and refer to felt that this improved the quality of care they could offer patients. Participants reported that the ability to rule in or rule out a diagnosis with confidence based on medical information and provide appropriate patient education was crucial to achieve patient buy-in and functional improvements. One participant noted: “And about three years ago, our area finally got a really good ENT. And that’s kind of been a barrier breaker for us” (Participant 4).
Interprofessional communication barriers, as well as long wait lists to access specialists, both medical and mental health, were consistently highlighted as problems. Physical therapists noted that they often referred to multiple types of providers: optometry, otolaryngology, cardiology, and behavioral health. They reported that it is stressful and time-consuming to find the right specialist and to facilitate these referrals. Physical therapists expressed desire for a timely, coordinated, interdisciplinary approach to care for individuals with chronic dizziness. Physical therapists emphasized how important obtaining timely medical information was for informing the physical therapy plan of care.
The optometrist and our otolaryngologist, the waiting list is between six months to a year. And so they’re getting the vestibular [test] batteries done with the audiologist first and then they’re making the referrals to PT, which is awesome. But sometimes they haven’t even met with the doctors yet to talk about their diagnosis, which can be really challenging to put that on me, as well (Participant 11).
Physical therapists also expressed concern that the long wait lists perpetuated delays in diagnosis and referral to physical therapy, which can cause dizziness to reach the chronic stage instead of allowing it to be addressed acutely, which may help limit functional and participation restrictions.
3.2.3. Behavior Influences Outcomes
Physical therapist participants identified that in individuals with chronic dizziness, maladaptive behavior may influence patients’ abilities to achieve successful functional and participation outcomes, highlighting the influence of psychosocial factors, such as mental health and personality traits. Physical therapists identified specific challenges with both hypervigilance and fear avoidance of dizziness symptoms that limited functional abilities. Physical therapists noted the importance of utilizing a habituation approach for intervention with those with chronic dizziness and gradual reintroduction to activities that may provoke dizziness. They noted the conflict that this evoked with the fear-avoidant behaviors of patients. Physical therapists spoke about the difficulty of trying to decrease vigilance on symptoms of dizziness while finding an appropriate level of challenge and maintaining the patient trust and comfort during treatment sessions:
And so being able to try and figure out what’s appropriate for them to do, or what they’re actually experiencing without focusing 100% on how high is your dizziness now? How much? …I think is one of the harder pieces too (Participant 13).
Physical therapists emphasized focusing on reintroduction to life roles and repetition of activities to address fear-avoidance behavior and empower patients. They discussed using positive reinforcement strategies during sessions and practicing functional goal setting to help individuals recognize small successes and improve self-efficacy in their ability to manage dizziness symptoms. “I try and celebrate their smallest achievement; I try to make a big deal about it. I think boosting that inner confidence in them, it plays a key role” (Participant 10).
4. Discussion
This is the first manuscript to explore both patient and provider experiences within the diagnosis and management of chronic dizziness. Both our physical therapist participants and participants with chronic dizziness were mostly female. While this may be impactful on results, physical therapy is a predominantly female occupation [30] and many etiologies of chronic dizziness have a higher prevalence among females [10,31,32]. Therefore, the results obtained resemble what might be expected in the target population based on the similarity in personal characteristics.
The most salient themes in these data included challenges navigating the health care system for those with chronic dizziness, the complex and multi-factorial nature of chronic dizziness requiring a multidisciplinary team, a loss of self-identity, and behavior influencing outcomes. Data collected during these focus groups were consistent with two prior qualitative studies that explored the lived experiences of individuals with persistent postural perceptual dizziness (PPPD), a specific type of chronic dizziness. Most specifically, themes of lack of validation and dismissal from health care providers and loss of self-identity were identified in both studies [15,33]. The findings in this study concur with the prior studies and highlight that these experiences are not unique to PPPD, and instead suggest common themes for many individuals with many types of vestibular diagnoses experiencing chronic dizziness.
4.1. Complexities Navigating the Health System
Our data confirm the complexity and challenge of the dizziness differential diagnosis process and the negative impact this can have on individuals with chronic dizziness. Individuals with dizziness described experiences of undergoing many medical tests, seeing many medical providers, and when their symptoms could not be diagnosed, experiencing not only concern about the uncertainty of their own condition but also some experienced dismissal and lack of validation from providers. The literature concurs with this finding, noting that individuals with chronic dizziness rate their physician’s empathy concerning their complaints significantly lower than individuals with acute dizziness [34].
This above-described diagnostic challenge can be characterized as epistemic injustice, which explores a power differential between the privilege of biomedical expertise over the patient’s lived experience [35]. In this situation, the medical provider has the power to pronounce what is real or not real and therefore they act as a gatekeeper [35]. When individuals cannot self-validate their symptoms, they often self-stigmatize [36]. This can have a negative impact on both psychological and physical health and damage trust in the health care system and the opportunity for therapeutic alliance for the individual involved. A therapeutic alliance involving a genuine, committed relationship between a patient and their health care provider is critical and has been associated with improved clinical outcomes [37]. The biopsychosocial model also highlights the importance of the patient–provider relationship as critical to successful patient outcomes [18]. Epistemic humility, whereby medical professionals listen to the lived experiences of their patients and acknowledge the limits of their expertise, is offered as a solution to maximize health outcomes of those with chronic conditions [38].
4.2. A Complex and Multi-Factorial Presentation and Importance of the Multidisciplinary Care Team
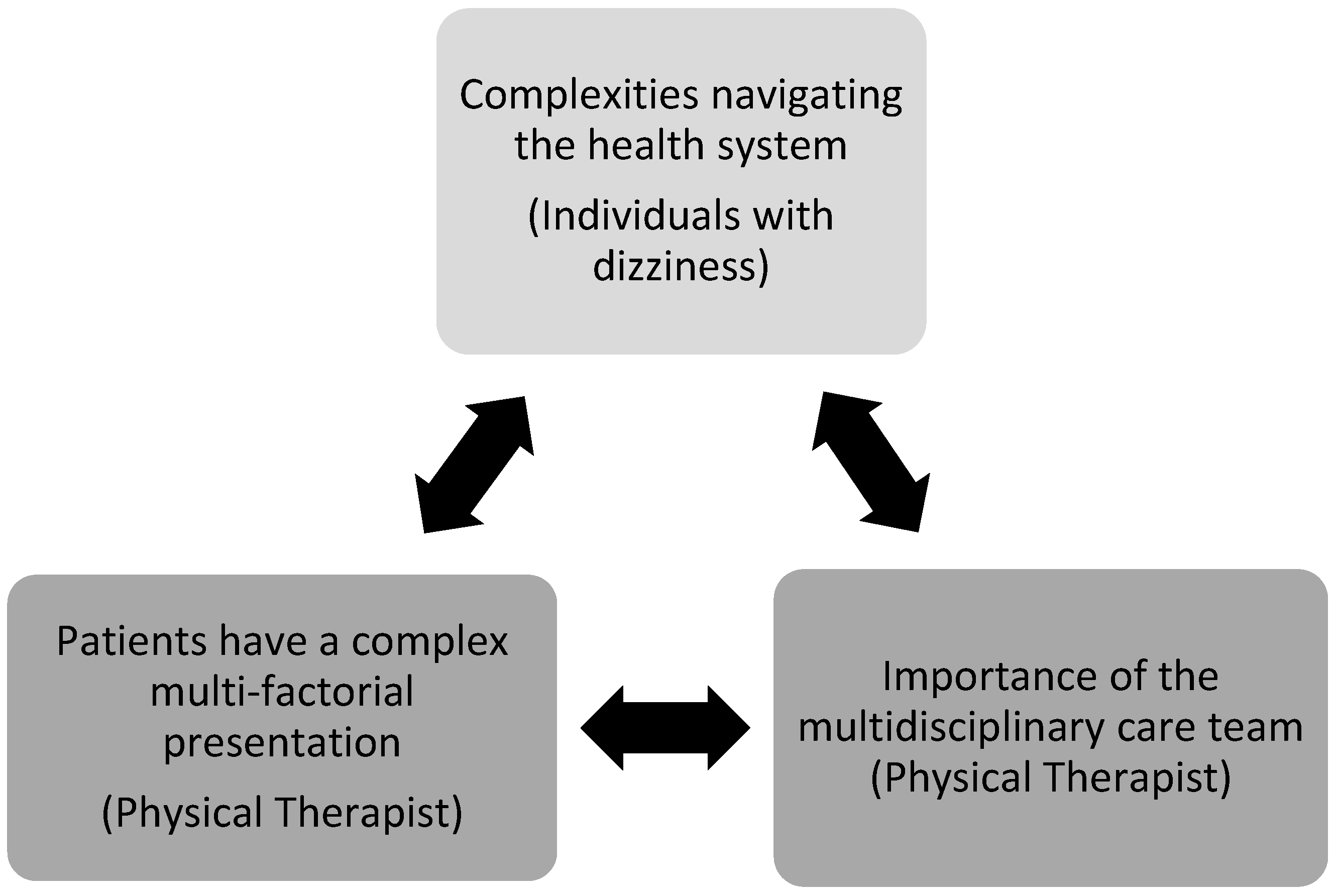
Our data from physical therapist participants about the importance of the multidisciplinary care team and the acknowledgement of the complexity of this patient population validate and help explain the feelings of frustration individuals with dizziness experienced navigating and finding answers within the health care system. These health system challenges are interconnected themes (Figure 2).
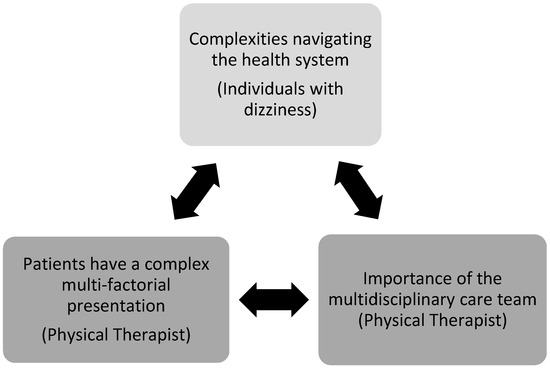
Figure 2.
Interconnectedness of health system challenges.
Physical therapist focus group data highlight the importance of utilizing a biopsychosocial approach to maximize outcomes for those with chronic dizziness, citing the impact of psychological factors such as mental health and social constructs, such as access to appropriate specialist care to improve outcomes. Physical therapist participants further utilized the biopsychosocial model by acknowledging the complex role that mental health plays in those with chronic dizziness, that it may be a pre-disposing factor to the development of chronic dizziness or it may be a perpetuating factor that continues to drive chronic dizziness [39].
The biopsychosocial model acknowledges the importance of a multidisciplinary care team to holistically address the patient’s needs. A multidisciplinary care clinic to provide a comprehensive evaluation of those with chronic dizziness, similar to those with chronic pain, may be a helpful solution for this patient population. A care team comprised of neuro-otology, neuro-optometry, psychology or psychiatry, occupational therapy, and physical therapy could help to expedite care for these individuals and save health care dollars by improving the ease of referrals and communication. Multidisciplinary clinics have been shown to be effective to decrease health care utilization and health care costs in other patient populations [40,41] as well as improve patient outcomes [42]. Multidisciplinary clinics have less frequently been explored in the literature for those with chronic dizziness. One study did report on the benefit of incorporating mental health services into a multidisciplinary clinic for those with chronic dizziness and noted improved disability [43]. A multidisciplinary clinic for those with chronic dizziness shows promise and warrants further exploration. Barriers to multidisciplinary clinics often include logistical problems such as scheduling, implementation cost, and concerns regarding a hierarchy on the health care team [44]. However, as health care moves towards the idea of value-based care, where reimbursement is tied to the results delivered, the idea of a multidisciplinary clinic where patients can receive holistic treatment to maximize outcomes is a prominent and important idea.
4.3. Loss of Self-Identity
Our data confirmed that individuals with dizziness had decreased ability to participate in social roles such as work or relationships with friends and family and this was closely tied to loss of self-identity. Our focus group data suggested lack of participation was tied to concerns about the timing, intensity, and unpredictability of dizziness and this in turn led to avoiding activities that might cause dizziness, or fear-avoidance behavior. The other literature has identified that fear-avoidance behavior can be related to constructs of catastrophic thinking about the causes and consequences of dizziness [45]; however, this did not emerge during these focus groups. Lack of participation in social roles was also related to challenges in the diagnostic process, as it was difficult to explain to others what their dizziness problem was when they did not know themselves.
4.4. Behavior Influences Outcomes
Physical therapist focus group data identified that behavior involving hypervigilance on dizziness and fear avoidance influenced treatment management and functional outcomes in those with dizziness. These physical therapist reports are consistent with reports from focus groups from individuals with chronic dizziness, who noted tending to avoid activities that may provoke dizziness, sometimes even to the point of isolating themselves socially. These data also highlight the interconnectedness of the themes collected between individuals with dizziness and vestibular physical therapists and suggest the need for and importance of a multidisciplinary care team.
The biopsychosocial model acknowledges the importance of patient behavior such as fear avoidance and self-efficacy on treatment adherence and patient outcomes. Physical therapists incorporated treatment management techniques to address these behaviors, including habituation and gradual reintroduction and repetition of functional tasks that provoked dizziness, similar to graded exposure techniques that are utilized in the chronic pain population [46]. When patients can confront and increasingly perform the tasks they previously feared, this may help to improve self-efficacy and a sense of empowerment to manage their dizziness. Additionally, therapists reported using motivational interviewing techniques [47] such as shared functional goal setting as well as increased positive reinforcement when goals were met to increase patient empowerment and self-management.
We recognize there may have been bias in the sample of individuals with chronic dizziness who participated in these focus groups. Individuals who were frustrated with the care they received within the health care system may have been more willing to speak up about these experiences compared to individuals who felt they received appropriate care to abate or minimize their symptoms. Therefore, it is difficult to know if the viewpoints expressed in these focus groups are transferable to all individuals with chronic dizziness.
These focus groups purposively sampled only physical therapists who worked with individuals with chronic dizziness as a first step to understand the experiences of both the patient and the health care provider working with chronic dizziness. Repeating this study with a multidisciplinary team may improve and deepen the understanding of these experiences and further inform future practice.
5. Conclusions
Although the literature acknowledges the diagnostic challenges and resulting functional implications that those with chronic dizziness experience, little has been investigated about why these challenges exist and what could be changed to improve this. This study investigated that gap. Our focus group participants with chronic dizziness confirmed difficulties receiving an effective diagnosis and management plan to address their symptoms of chronic dizziness. They noted frustrating experiences undergoing multiple tests with multiple medical providers without a clear outcome and effective plan of care. This points to the need for early referrals to appropriate specialists to manage dizziness. Providers may also benefit from embracing epistemic humility, listening to the lived experiences of their patients, and acknowledging the limits of their expertise. Physical therapist focus group participants concurred with the idea that the diagnostic and management process to address chronic dizziness needs improvement and warrants change. Physical therapists noted the medical and psychosocial complexities of this patient population and that no one provider could operate successfully in a silo, even when the diagnostic management process was effective. To achieve successful outcomes for individuals with dizziness, a multidisciplinary care team is essential to address the patient’s needs holistically. A multidisciplinary clinic for individuals with chronic dizziness could offer a solution to mitigate this problem. A multidisciplinary chronic dizziness clinic with neuro-otological expertise could offer a more efficient medical diagnosis with ensuing timely communication and referrals to mental health and rehabilitation providers. This may expediate individuals in returning to participating in meaningful life activities and result in improved patient outcomes and quality of life, while saving health care dollars. Future research is needed to explore the benefits and feasibility of this idea.
Author Contributions
E.C. contributed to the project conceptualization, methodology, analysis, and writing, reviewing, and editing the manuscript. K.S. contributed to project data analysis, writing, reviewing, and editing the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Mass General Brigham Institutional Review Board prior to data collection (Protocol # 2022P003392). Approval was received 23 January 2023.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
This dataset is not available due to privacy and ethical restrictions.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
- Individuals with Chronic Dizziness Focus Group Interview Questions
- 1.
- Please tell me how your dizziness started.
- 2.
- Please tell me how it is living with dizziness today.
- 3.
- How is your every-day life affected by your dizziness symptoms?
- 4.
- How was your life situation before your dizziness started? And now?
- 5.
- How would your life be like today without dizziness?
- 6.
- Please tell me about a dizziness episode. What happened? What did you do?
- 7.
- Please tell me about your contact with health care due to your dizziness?
- 8.
- Are there other ways the health care system could help you more with your dizziness?
Appendix B
- Physical Therapist Focus Group Interview Questions
- Please tell me about your background providing physical therapy to individuals with chronic dizziness
- Please tell me how you feel about treating patients with chronic dizziness.
- Follow up: Do you find any particular aspects of managing these patients difficult?
- How would you describe the usual type of approach you take with patients with chronic dizziness?
- Do you often consult other providers when working with individuals with dizziness?
- When you see a patient for the first time, do you ever think to yourself, “they’ll recover or they won’t recover?”
- Follow up: How can you tell or what makes you say this?
Appendix C

Table A1.
Themes, codes, and excerpts.
Table A1.
Themes, codes, and excerpts.
| Individuals with Chronic Dizziness | ||
| Theme | Code | Excerpt |
| Complexities navigating the health system | Dismissal/power dynamic | It was a long time of people just, really doctors saying, there’s nothing wrong with you. It’s anxiety and depression, which is very, very frustrating, very upsetting. (Focus group 2, participant 5) |
| Many different medical providers | For me, I saw a ton of different specialties… I saw PT, I saw OT, I saw speech, I saw PM&R, I saw neurology, I saw primary care. I saw neuro-optometry. (Focus group 1, participant 1) | |
| Inconclusive medical work-up | I went to do a lot of testing for my dizziness. But they never really found what the cause of it was. (Focus group 4, participant 12) | |
| Ineffective treatment | I did do physical therapy, it didn’t work for me. I went for a couple months. They told me that there was nothing more that they could do for me. I agreed. (Focus group 1, participant 2) | |
| Health insurance limitations | So, and then you get this huge bill for the hospital fee on top of their office visit without any results or no ongoing contact… and that was very frustrating. And then insurance, just incredibly frustrated with the health care system in general in terms of how illness and long-term care needs are met or not met is really the point here. Especially when you don’t fit neatly into a category (Focus group 1, participant 4) | |
| Loss of self-identity | Functional limitations | Sometimes I can’t even run to (grocery store) and pick up a couple things because walking through the aisles and scanning, you know, where the ketchup is will be really uncomfortable for me (Focus group 2, participant 6) |
| Participation restrictions | So I can’t teach. I can do my own work for very short periods of time, but it’s a big interruption. You know I was supposed to have an exhibition, and I had to cancel it… My career is interrupted. (Focus group 3, participant 10) | |
| Unpredictability of dizziness | And just out of the blue, it would hit me, you know? It will just happen (Focus group 2, participant 7) | |
| Vestibular Physical Therapists | ||
| Theme | Code | Excerpt |
| Patients have a complex, multi-factorial presentation | Multiple body systems involved | I always assess the neck a lot as well… because of dizziness with head motion they are fearful to move their heads. So I’m trying to be holistic in how I look at the patient. (Focus group 1, participant 3) |
| Psychosocial factors influence care | They are coming to me asking why everyone thinks they’re crazy and they’re trying to prove to me that it’s not all in their head (Focus group 3, participant 9) | |
| Importance of the multidisciplinary care team | Facilitating referrals to other providers (medical and mental health) | It’s so hard when they’re having to go to so many different professionals with their concussion… You could be sending them to the optometrist, psychologist, to the athletic trainer, to the dietician (Focus group 2, participant 5) |
| Wait list/delayed access | The optometrist and our otolaryngologist, the waiting list is six months to a year. And so they’re getting the vestibular (test) batteries done with the audiologist first and then making referrals to PT… but sometimes they haven’t even met with the doctors yet to talk about their diagnosis, which can be really challenging (Focus group 3, participant 11) | |
| Behavior influences outcomes | Hypervigilance of dizzy symptoms | I certainly get away from symptom monitoring. Just a simple shift in how I’m asking how they’re doing. Sometimes I’ll just identify in the beginning, I know you have dizziness, I know what I’m going to ask you to do is going to make you more dizzy, tell me when we need a rest break (Focus group 4, participant 14) |
| Fear avoidance | A lot of people I’ve found are fearful to move their heads because of dizziness with head motion. They have a lot of fear avoidance behaviors (Focus group 1, participant 4) | |
| Functional training and habituation | Leading it more towards functional treatment, like functional activities or functional tasks, with less of a hyper focus on the vestibular piece (Focus group 4, participant 13) | |
References
- Dunlap, P.M.; Khoja, S.S.; Whitney, S.L.; Freburger, J.K. Assessment of health care utilization for dizziness in ambulatory care settings in the United States. Otol. Neurotol. 2019, 40, e918–e924. [Google Scholar] [CrossRef]
- Benecke, H.; Agus, S.; Kuessner, D.; Goodall, G.; Strupp, M. The burden and impact of vertigo: Findings from the REVERT patient registry. Front. Neurol. 2013, 4, 53647. [Google Scholar] [CrossRef]
- Neuhauser, H.K.; Radtke, A.; von Brevern, M.; Lezius, F.; Feldmann, M.; Lempert, T. Burden of Dizziness and Vertigo in the Community. Arch. Intern. Med. 2008, 168, 2118. [Google Scholar] [CrossRef]
- Whitney, S.L.; Sparto, P.J.; Furman, J.M. Vestibular rehabilitation and factors that can affect outcome. Semin. Neurol. 2020, 40, 165–172. [Google Scholar] [CrossRef]
- Steensnaes, M.H.; Knapstad, M.K.; Goplen, F.K.; Berge, J.E. Persistent Postural-Perceptual Dizziness (PPPD) and quality of life: A cross-sectional study. Eur. Arch. Otorhinolaryngol. 2023, 280, 5285–5292. [Google Scholar] [CrossRef]
- Jeong, S.S.; Simpson, K.N.; Johnson, J.M.; Rizk, H.G. Assessment of the Cost Burden of Episodic Recurrent Vestibular Vertigo in the US. JAMA Otolaryngol. Neck Surg. 2022, 148, 1103. [Google Scholar] [CrossRef]
- Mueller, M.; Strobl, R.; Jahn, K.; Linkohr, B.; Peters, A.; Grill, E. Burden of disability attributable to vertigo and dizziness in the aged: Results from the KORA-Age study. Eur. J. Public Health 2014, 24, 802–807. [Google Scholar] [CrossRef]
- Bösner, S.; Schwarm, S.; Grevenrath, P.; Schmidt, L.; Hörner, K.; Beidatsch, D.; Bergmann, M.; Viniol, A.; Becker, A.; Haasenritter, J. Prevalence, aetiologies and prognosis of the symptom dizziness in primary care—A systematic review. BMC Fam. Pract. 2018, 19, 33. [Google Scholar] [CrossRef]
- Shaw, B.H.; Stiles, L.E.; Bourne, K.; Green, E.A.; Shibao, C.A.; Okamoto, L.E.; Garland, E.M.; Gamboa, A.; Diedrich, A.; Raj, V.; et al. The face of postural tachycardia syndrome–insights from a large cross-sectional online community-based survey. J. Intern. Med. 2019, 286, 438–448. [Google Scholar] [CrossRef]
- Formeister, E.J.; Rizk, H.G.; Kohn, M.A.; Sharon, J.D. The Epidemiology of Vestibular Migraine: A Population-based Survey Study. Otol. Neurotol. 2018, 39, 1037–1044. [Google Scholar] [CrossRef]
- Newman-Toker, D.E.; Cannon, L.M.; Stofferahn, M.E.; Rothman, R.E.; Hsieh, Y.-H.; Zee, D.S. Imprecision in Patient Reports of Dizziness Symptom Quality: A Cross-sectional Study Conducted in an Acute Care Setting. Mayo Clin. Proc. 2007, 82, 1329–1340. [Google Scholar] [CrossRef]
- Busetto, L.; Wick, W.; Gumbinger, C. How to use and assess qualitative research methods. Neurol. Res. Pract. 2020, 2, 14. [Google Scholar] [CrossRef]
- Toye, F.; Seers, K.; Barker, K.L. Meta-ethnography to understand healthcare professionals’ experience of treating adults with chronic non-malignant pain. BMJ Open 2017, 7, e018411. [Google Scholar] [CrossRef]
- Toye, F.; Seers, K.; Hannink, E.; Barker, K. A mega-ethnography of eleven qualitative evidence syntheses exploring the experience of living with chronic non-malignant pain. BMC Med. Res. Methodol. 2017, 17, 116. [Google Scholar] [CrossRef]
- Gamble, R.; Sumner, P.; Wilson-Smith, K.; Derry-Sumner, H.; Rajenderkumar, D.; Powell, G. Using interpretative phenomenological analysis to probe the lived experiences of persistent postural-perceptual dizziness (PPPD). J. Vestib. Res. 2023, 33, 89–103. [Google Scholar] [CrossRef]
- Rathert, C.; Wyrwich, M.D.; Boren, S.A. Patient-Centered Care and Outcomes: A Systematic Review of the Literature. Med. Care Res. Rev. 2013, 70, 351–379. [Google Scholar] [CrossRef]
- Engel, G.L. The clinical application of the biopsychosocial model. Am. J. Psychiatry 1980, 137, 535–544. [Google Scholar] [CrossRef]
- Borrell-Carrió, F.; Suchman, A.L.; Epstein, R.M. The biopsychosocial model 25 years later: Principles, practice, and scientific inquiry. Ann. Fam. Med. 2004, 2, 576–582. [Google Scholar] [CrossRef]
- van Dijk, H.; Köke, A.J.A.; Elbers, S.; Mollema, J.; Smeets, R.J.E.M.; Wittink, H. Physiotherapists Using the Biopsychosocial Model for Chronic Pain: Barriers and Facilitators—A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 1634. [Google Scholar] [CrossRef]
- Polit, D.; Beck, C. Nursing Research: Generating and Assessing Evidence for Nursing Practice, 11th ed.; Wolters Kluwer: Alphen on the Rhine, The Netherlands, 2021. [Google Scholar]
- Lochmiller, C.R.; Lester, J.N. An Inroduction to Educational Research: Connecting Methods to Practice; Sage: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Bradbury-Jones, C.; Sambrook, S.; Irvine, F. The phenomenological focus group: An oxymoron? J. Adv. Nurs. 2009, 65, 663–671. [Google Scholar] [CrossRef]
- Olsson Möller, U.; Hansson, E.E.; Ekdahl, C.; Midlöv, P.; Jakobsson, U.; Kristensson, J. Fighting for control in an unpredictable life—A qualitative study of older persons’ experiences of living with chronic dizziness. BMC Geriatr. 2014, 14, 97. [Google Scholar] [CrossRef]
- Jeffrey, J.E.; Foster, N.E. A Qualitative Investigation of Physical Therapists’ Experiences and Feelings of Managing Patients with Nonspecific Low Back Pain. Phys. Ther. 2012, 92, 266–278. [Google Scholar] [CrossRef]
- Hall, C.D.; Herdman, S.J.; Whitney, S.L.; Anson, E.R.; Carender, W.J.; Hoppes, C.W.; Cass, S.P.; Christy, J.B.; Cohen, H.S.; Fife, T.D.; et al. Vestibular Rehabilitation for Peripheral Vestibular Hypofunction: An Updated Clinical Practice Guideline From the Academy of Neurologic Physical Therapy of the American Physical Therapy Association. J. Neurol. Phys. Ther. 2022, 46, 118–177. [Google Scholar] [CrossRef]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual. Quant. 2018, 52, 1893–1907. [Google Scholar] [CrossRef]
- Lumivero, NVivo. Available online: https://lumivero.com/products/nvivo/ (accessed on 8 August 2024).
- Miles, M.B.; Huberman, A.M.; Saldana, J. Qualitative Data Analysis: A Methods Sourcebook, 3rd ed.; SAGE Publications Ltd.: Szeng de Oakes, CA, USA, 2014. [Google Scholar]
- Guba, E.G. Criteria for assessing the trustworthiness of naturalistic inquiries. Educ. Commun. Technol. J. 1981, 29, 75. [Google Scholar] [CrossRef]
- American Physical Therapy Association. A Physical Therapy Profile: Demographics of the Profession, 2021–2022. Available online: https://www.apta.org/apta-and-you/news-publications/reports/2023/physical-therapy-profile-demographics-profession-2021-22 (accessed on 15 July 2023).
- Kim, H.-J.; Lee, J.-O.; Choi, J.-Y.; Kim, J.-S. Etiologic distribution of dizziness and vertigo in a referral-based dizziness clinic in South Korea. J. Neurol. 2020, 267, 2252–2259. [Google Scholar] [CrossRef]
- Cha, Y. Mal de debarquement syndrome: New insights. Ann. N. Y. Acad. Sci. 2015, 1343, 63–68. [Google Scholar] [CrossRef]
- Sezier, A.E.I.; Saywell, N.; Terry, G.; Taylor, D.; Kayes, N. Working-age adults’ perspectives on living with persistent postural-perceptual dizziness: A qualitative exploratory study. BMJ Open. 2019, 9, e024326. [Google Scholar] [CrossRef]
- Sczepanek, J.; Wiese, B.; Hummers-Pradier, E.; Kruschinski, C. Newly diagnosed incident dizziness of older patients: A follow-up study in primary care. BMC Fam. Pract. 2011, 12, 58. [Google Scholar] [CrossRef]
- Sebring, J.C.H. Towards a sociological understanding of medical gaslighting in western health care. Sociol. Health Illn. 2021, 43, 1951–1964. [Google Scholar] [CrossRef]
- Armentor, J.L. Living with a Contested, Stigmatized Illness: Experiences of Managing Relationships among Women with Fibromyalgia. Qual. Health Res. 2017, 27, 462–473. [Google Scholar] [CrossRef]
- Miciak, M.; Mayan, M.; Brown, C.; Joyce, A.S.; Gross, D.P. The necessary conditions of engagement for the therapeutic relationship in physiotherapy: An interpretive description study. Arch. Physiother. 2018, 8, 3. [Google Scholar] [CrossRef]
- Buchman, D.Z.; Ho, A.; Goldberg, D.S. Investigating Trust, Expertise, and Epistemic Injustice in Chronic Pain. J. Bioethical Inq. 2017, 14, 31–42. [Google Scholar] [CrossRef]
- Saxena, A.; Paredes-Echeverri, S.; Michaelis, R.; Popkirov, S.; Perez, D.L. Using the Biopsychosocial Model to Guide Patient-Centered Neurological Treatments. Semin. Neurol. 2022, 42, 80–87. [Google Scholar] [CrossRef]
- Skinner, M.L.; Lee, S.K.; Collaco, J.M.; Lefton-Greif, M.A.; Hoch, J.; Au Yeung, K.J. Financial and Health Impacts of Multidisciplinary Aerodigestive Care. Otolaryngol. Neck Surg. 2016, 154, 1064–1067. [Google Scholar] [CrossRef]
- Rao, S.; Burch, M.; Fredwall, M.M.; Enciso, L.; Trott, K.; Patel, A.D.; Albert, D.V.F. Multidisciplinary Care for Pediatric Patients with Psychogenic Nonepileptic Seizures May Be Associated with Decreased Health Care Utilization. Neurol. Clin. Pract. 2023, 13, e200195. [Google Scholar] [CrossRef]
- Sunkara, P.R.; Islam, T.; Bose, A.; Rosenthal, G.E.; Chevli, P.; Jogu, H.; Tk, L.A.; Huang, C.-C.; Chaudhary, D.; Beekman, D.; et al. Impact of structured interdisciplinary bedside rounding on patient outcomes at a large academic health centre. BMJ Qual. Saf. 2020, 29, 569–575. [Google Scholar] [CrossRef]
- Gerretsen, P.; Shah, P.; Logotheti, A.; Attia, M.; Balakumar, T.; Sulway, S.; Ranalli, P.; Dillon, W.A.; Pothier, D.D.; Rutka, J.A. Interdisciplinary integration of nursing and psychiatry (INaP) improves dizziness-related disability. Laryngoscope 2020, 130, 1800–1804. [Google Scholar] [CrossRef]
- Korylchuk, N.; Pelykh, V.; Nemyrovych, Y.; Didyk, N.; Martsyniak, S. Challenges and Benefits of a Multidisciplinary Approach to Treatment in Clinical Medicine. J. Pioneer. Med. Sci. 2024, 13, 1–9. [Google Scholar] [CrossRef]
- Pothier, D.D.; Shah, P.; Quilty, L.; Ozzoude, M.; Dillon, W.A.; Rutka, J.A.; Gerretsen, P. Association between Catastrophizing and Dizziness-Related Disability Assessed with the Dizziness Catastrophizing Scale. JAMA Otolaryngol. Neck Surg. 2018, 144, 906. [Google Scholar] [CrossRef]
- George, M.S.; Taylor, J.J. Theoretical Basis for Transcranial Magnetic Stimulation. In A Clinical Guide to Transcranial Magnetic Stimulation; Holtzheimer, P.E., McDonald, W., Eds.; Oxford University Press: Oxford, UK, 2014; pp. 1–7. [Google Scholar] [CrossRef]
- Pignataro, R.M.; Huddleston, J. The Use of Motivational Interviewing in Physical Therapy Education and Practice: Empowering Patients Through Effective Self-Management. J. Phys. Ther. Educ. 2015, 29, 62–71. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).