Abstract
Background: This study aimed to identify clinical characteristics and classifications of nasal septal deviations associated with revision septoplasty. Methods: The cross-sectional study design included 652 patients undergoing septoplasty at a tertiary referral center. We classified patients according to Baumann’s validated septal deviation classification and assessed similarities and differences regarding septal pathologies and types of nasal septal deviations in both groups. Results: The sample comprised 600 primary surgery cases and 52 revision cases. In primary surgeries, type 1 septal deviations were most common (60.3%), followed by type 5 (10.5%) and type 3 (10.0%). In revision surgeries, type 1 deviations (36.5%) were most common, followed by type 3 (25.0%) and type 2 (17.3%). Group comparisons revealed that type 2 and type 3 septal deviations, high septal deviations, and septal perforations were significantly more frequent in revision cases. Common septal pathologies included an oblique septum (98.0%), ipsilateral septal crest (76.4%), contralateral turbinal hyperplasia (42.5%), and vomeral spur (39.9%). Conclusions: This study suggests that using validated classification systems for septal deviations, which combine various pathologies, can provide a more clinically relevant assessment and improve patient counseling and treatment.
1. Introduction
Surgical correction of nasal septal deviations, also known as septoplasty, is one of the most common surgeries performed on adults in otorhinolaryngology [1,2]. Although mostly successful, 1.1% to 4.4% of patients report ongoing nasal obstruction after primary surgery and require revision septoplasty [3,4,5,6]. Identifying risk factors for revision is vital to recognize those patients at risk, thus improving patient counseling, overall outcome, and quality of life, as well as reducing complications [7].
The success of septoplasty depends on careful preoperative planning. Therefore, a preoperative clinical examination of the nose and the nasal septum is essential to identify the main pathology and determine the surgical key steps. Although several authors previously suggested different classification systems for septal deviations to improve comparability between individual studies and facilitate future research regarding clinical outcomes, these are rarely used in everyday clinical practice [8]. Several authors utilized classification systems based on the shape or pattern of the septal deviation, such as the distinction between S-shaped and C-shaped deviations [9]. Meanwhile, others used the main septal pathology as a means of classification [10]. Baumann et al. developed a classification system based on the combination of leading and concomitant septal pathologies, allowing a comprehensive assessment of nasal septal deviations (Figure 1 [11]). It distinguishes six types of septal deviations: type 1 (septal crest and ipsilateral vomeral spur), type 2 (cartilaginous deviated nose), type 3 (high septal deviation), type 4 (caudally inclined septum, ipsilateral septal crest, and ipsilateral vomeral spur), type 5 (septal crest and contralateral vomeral spur), and type 6 (caudally inclined septum, contralateral septal crest, and contralateral vomeral spur) [11].
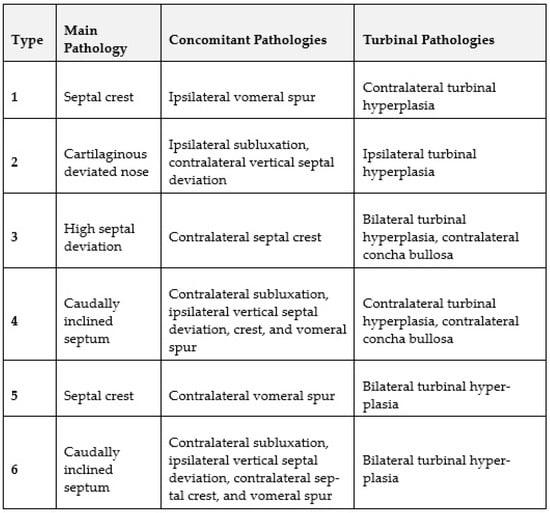
Figure 1.
Baumann Types of nasal septal deviations [11].
Previous studies have shown that the majority of persistent septal deviations after primary surgery are located in the middle (58%) and caudal (31%) septum [12]. Anatomical characteristics such as caudal or dorsal septal deflections were previously identified as potential risk factors for revision septoplasty, as their surgical correction tends to be more challenging [5,13,14]. Furthermore, nasal valve collapse was suggested to be associated with a higher need for revision septoplasty. At the same time, a history of face trauma and obstructive sleep apnea syndrome (OSAS) did not seem to affect the likelihood of revision [15].
Nevertheless, no previous studies compared anatomical differences based on Baumann’s classification for nasal septal deviations between primary and revision cases. Therefore, the aim of this study was to comprehensively evaluate similarities and differences in Baumann’s classification for nasal septal deviations in patients undergoing primary and revision septoplasty. The Figure 1 lists the main, concomitant and turbinal pathologies of each type of septal deviation.
2. Materials and Methods
This retrospective, cross-sectional, single-center study was approved by the Ethics Committee of the Medical University of Vienna (approval number: 1737/2020) and conducted at the Department of Otorhinolaryngology at the Medical University of Vienna. We included all patients undergoing septoplasty at the Medical University of Vienna (General Hospital of Vienna) between 1 January 2010 and 31 December 2015 and retrieved data regarding demographics, septal pathologies, and surgical procedures from the hospital’s patient record database. All patients were classified as primary surgeries (i.e., the patient had not undergone septoplasty previously) or revision surgeries (i.e., the patient reported one or more previous septoplasties either at our center or at another hospital).
Demographics included age at the time of surgery (years), gender (female/male), smoking status (yes/no), physician-diagnosed diabetes (yes/no), physician-diagnosed OSAS (yes/no), previous nose/face trauma (yes/no), and the number of previous septoplasties (absolute number).
Concerning septal pathologies, we classified all patients according to Baumann’s classification of septal deviations [11] as types 1–6 (using documented information from surgery and thorough preoperative physical examination. The definitions of all six types of septal deviations and their main, concomitant and turbinal pathologies are listed in Figure 1 [11]. Furthermore, we obtained the following information regarding the patients’ septal pathologies: subluxation (yes/no), oblique septum (yes/no), septal spur (yes/no), high septal deviation (yes/no), ipsilateral septal crest (yes/no), contralateral septal crest (yes/no), ipsilateral concha bullosa (yes/no), contralateral concha bullosa (yes/no), vomeral spur (yes/no), septal perforation (yes/no), ipsilateral turbinal hyperplasia (yes/no), contralateral turbinal hyperplasia (yes/no), bilateral turbinal hyperplasia (yes/no), absent turbinal hyperplasia (yes/no), nasal alar collapse (yes/no).
We used the IBM software SPSS (Version 25.0 for Mac Os, IBM Corp., Armonk, NY, USA) and Microsoft Excel (Redmond, WA, USA, 2016 16.0.5465.1000 MSO 16.0.5465.1000 32-Bit) for all statistical analyses. We assumed normal distribution based on histograms. The data was listed in tables for all patients and separately for primary and revision surgery cases. Continuous variables were presented as mean ± standard deviation (SD). Categorical variables were presented as absolute numbers (percentages).
We performed mean comparisons for continuous variables using an unpaired two-tailed t-test. Furthermore, the chi-squared test (χ2-test) and Fisher’s exact test were applied for group comparisons of categorical binary variables. The level of significance was set at 0.05.
3. Results
3.1. Demographics
Six hundred and fifty-two patients with a mean age of 34.6 years (standard deviation, SD = 12.7) underwent septoplasty at the Medical University of Vienna throughout the study period and were included in this study (Table 1).

Table 1.
Study participants’ demographical characteristics. Continuous variables are presented as mean ± SD (standard deviation), and categorial variables as absolute numbers (percentage).
The study population comprised 182 (27.9%) women and 470 (72.1%) men. Out of all 652 cases, 600 (92.0%) surgeries were classified as primary surgeries (i.e., the patient had not undergone septoplasty previously), and 52 (8.0%) surgeries were revision cases (i.e., the patient reported one or more previous septoplasties) with a mean of 1.1 (SD = 0.4) previous surgeries. Out of the whole cohort, 138 (21.2%) patients were smokers, four (0.6%) patients presented physician-diagnosed diabetes, 25 (3.8%) had been diagnosed with OSAS, and 127 (19.5%) of the study participants reported a previous nose or face trauma. Using unpaired two-tailed t-test, χ2-test, and Fisher’s exact test, no significant demographic differences between primary and revision surgery patients could be detected (Table 1).
3.2. Rates of Baumann Types of Septal Deviations
The majority of patients exhibited Baumann type 1 septal deviation (58.4%, Table 2). In the group of primary surgeries, type 1 was the most common septal deviation type (60.3%) followed by type 5 (10.5%), type 3 (10.0%), type 4 (8.3%), type 2 (7.5%), and type 6 (3.3%). Among revision patients, type 1 (36.5%) was followed by type 3 (25.0), type 2 (17.3%), type 4 (15.4%), type 5 (5.8%), and type 6 (0.0%).

Table 2.
Absolute numbers (and percentages) of different types of septal pathologies, i.e., classification of septal deviations (type 1–6) according to Baumann, subluxation (yes/no), oblique septum (yes/no), septal spur (yes/no), high septal deviation (yes/no), ipsilateral septal crest (yes/no), contralateral septal crest (yes/no), ipsilateral concha bullosa (yes/no), contralateral concha bullosa (yes/no), vomeral spur (yes/no), septal perforation (yes/no), ipsilateral turbinal hyperplasia (yes/no), contralateral turbinal hyperplasia (yes/no), bilateral turbinal hyperplasia, absent turbinal hyperplasia (yes/no), and nasal alar collapse as absolute number (percentages).
3.3. Rates of Individual Septal Pathologies
The most common septal pathology among all patients was an oblique septum (98.0%, Table 2). Ipsilateral septal crests were more common than contralateral septal crests and were found in 76.4% of all cases. Contralateral concha bullosa (8.7%) was identified more frequently than ipsilateral concha bullosa (5.7%). Contralateral turbinal hyperplasia (42.5%) was more common than ipsilateral turbinal hyperplasia (36.5%) and bilateral turbinal hyperplasia (30.1%), but not as common as absent turbinal hyperplasia (48.9%). Of all cases, 39.9% exhibited a vomeral spur, 22.2% a septal spur, 15.0% a high septal deviation, and 13.5% a septal subluxation. Septal perforations (2.3%) and nasal alar collapse (1.5%) were the least common pathologies.
3.4. Differences between Primary and Revision Surgery
Concerning the Baumann classification of septal deviations, patients undergoing primary septoplasty presented with Baumann type 1 septal deviations at significantly higher rates (60.3%, p-value = 0.001) than patients undergoing revision surgery (Table 2). However, Baumann type 2 (17.3%, p-value = 0.030) and type 3 (25.0%, p-value = 0.001) septal deviations were significantly more prevalent in patients undergoing revision surgery. Although Baumann type 4 septal deviations were found more often in revision patients (15.4%), it failed to reach significance (p-value = 0.121) in group comparison analysis. Baumann type 5 (10.5%) and type 6 septal deviations were more common among patients undergoing primary septoplasty but also failed to reach significance when assessed using group comparison.
χ2-test revealed that significantly more patients undergoing revision septoplasty presented high septal deviations (28.8%, p-value = 0.004) and septal perforations (9.6%, p-value = 0.004). Ipsilateral septum crests (78.5%, p-value < 0.001) and vomeral spurs (41.2%, p-value = 0.022) were more common in patients undergoing primary surgery.
3.5. Similarities between Primary and Revision Surgery
Among all patients included in this study and among primary and revision cases alike, the most common Baumann type of septal deviation was type 1 (58.4%), while the least common was type 6 (3.1%, Table 2). The rates of concha bullosa (i.e., ipsilateral and contralateral), turbinal hyperplasia (i.e., ipsilateral, contralateral, bilateral, and absent), and nasal alar collapse were similar in the primary and revision groups. Specifically, the rates of turbinal pathologies were relatively high in both groups, with contralateral turbinal hyperplasia as the most common subtype and rates of 43.1% in primary and 36.5% in revision patients (Table 2).
4. Discussion
Although septoplasty leads to symptom relief in most cases, up to 33% of patients report unsatisfactory results, and up to 4.4% of patients require revision surgery [3,16]. Revision septoplasty is associated with possible complications, additional costs, health risks, and a decreased quality of life [3,4,17]. Therefore, it is crucial to identify which factors and anatomical pathologies are associated with revision surgery to recognize septal deviation cases requiring special care, experience, and caution. This study found that Baumann type 2, type 3, and type 4 septal deviations were significantly associated with revision surgery. On the contrary, analyses with isolated anatomical findings of the nasal septum as predictive factors merely revealed an association between high septal deviations and revision septoplasty.
In this study, we classified 652 patients with septal deviations according to Baumann’s classification of septal deviations (types 1–6). The majority of patients (58.4%) were classified as Baumann type 1 septal deviation, followed by type 3 (11.2%), type 5 (10.1%), type 4 (8.9%), and type 2 (8.3%). The least common type was type 6, which was found in 3.1% of patients. These findings are comparable to the results Baumann et al. published when first describing their classification system. They analyzed septal deviations in 1088 patients and also identified type 1 (46%) as the most common form, followed by type 2 (23.1%), type 3 (13.1%), type 4 (9.3%), type 5 (4.7%), and finally type 6 (3.8%) as the least common form [11]. Although the order slightly differs from our study, the percentages of each type show a high amount of similarity. This might be explained by the cultural and geographic similarities between the patient populations of both studies.
The Baumann classification of septal deviations employs the combination of several different main and concomitant septal pathologies to distinguish six different types of septal deviations [11]. We opted for this classification system as it is a German classification system that is frequently used at our center and is among the most cited classifications for septal deviations on Google Scholar. However, other classification systems, such as the classification system by Mladina et al., using the main pathology, are also very significant tools for the assessment of septal deviation [10]. Other more straightforward classification systems use the shape and pattern of septal deviations and distinguish S-shaped and C-shaped septal deviations [9] or the severity of septal deviations [8]. Although the more basic classification systems are easier to apply in everyday clinical practice, they are not as comprehensive as other classifications that represent a combination of different septal pathologies. Nevertheless, using validated classification systems for nasal septal deviations has previously been recommended to improve comparability between individual studies and facilitate future research [8].
Group comparison revealed that Baumann’s type 2 and type 3 septal deviations were significantly more common among revision patients, whereas type 1 septal deviations were found more frequently in patients undergoing primary surgery. Our group comparison analysis of the individual anatomical pathologies without using a classification system revealed that ipsilateral septal crests and vomeral spurs were identified more frequently in patients undergoing primary surgery. In contrast, two pathologies were significantly more common in patients undergoing revision septoplasty: septal perforation and high septal deviation. This comes as no surprise, as septal perforation is a possible complication of septoplasty. Therefore, in most cases, it is not a primary cause of poor outcome after septoplasty but is instead caused by primary surgery itself [18]. The second factor, high septal deviation, was also identified more frequently in revision cases. This is in accordance with previous studies that reported high septal deviations ranking among the most difficult-to-treat septal deviations [19]. This may be caused by the fact that high septal deviations can contribute to the narrowing of the internal nasal valve, which is often associated with breathing difficulties, and additionally, high deviations require more surgical experience to facilitate correction at the first go [13]. However, nasal alar collapse was only found in 1.5% of cases. This low number may be due to the fact that patients with nasal alar collapse or nasal valve collapse often require septorhinoplasty in order to properly improve their breathing difficulties, as septoplasty alone often does not sufficiently improve nasal breathing for patients presenting with this type of pathology.
Although this study obtained important information regarding risk factors for revision surgery in patients with septal deviations, there were some limitations. This study followed a cross-sectional retrospective study design, which only allowed for an assessment of patients at a one-time point (i.e., surgery). For this reason, pathologies in revision cases prior to their primary surgery are unknown. Another aspect one has to take into account is the fact that septal deviation is not the only cause of nasal obstruction and breathing difficulties. A number of other pathologies and co-morbidities, such as chronic rhinosinusitis or allergies, also contribute to nasal obstruction [20]. This study did not focus on other influencing factors, which could also potentially contribute to dissatisfactory results after primary surgery. Furthermore, as this was a single-center study, patients who proceeded to undergo revision surgery in other hospitals could not be included. Future studies following a longitudinal study design could facilitate a more precise assessment of the outcome and revision rates after septoplasty and possible causal factors. Moreover, using revision surgery as the outcome implies a bias in itself. Some patients may require revision septoplasty but refrain from undergoing surgery for various reasons like risk or fear of complications, medical conditions, or inability to undergo anesthesia. Nevertheless, this study obtained important information for the assessment of patients undergoing septoplasty.
This study revealed that type 1 was the most common and type 6 the least common Baumann type of septal deviations among all patients. The rates of concha bullosa (i.e., ipsilateral and contralateral), turbinal hyperplasia (i.e., ipsilateral, contralateral, bilateral, and absent), and nasal alar collapse were similar in the primary and revision groups. Analysis of individual septal pathologies revealed that high septal deviations (as included in Baumann’s type 3 septal deviations) were significantly more common among revision patients, while many other septal pathologies that are also included in the Baumann classification failed to reach significance when assessed individually.
5. Conclusions
In conclusion, our data allowed for new insights into nasal septal deviations, the different nasal pathologies, types of septal deviations, and their occurrence rates. The results of this study suggest that classifying septal deviations preoperatively by using validated classification systems allows for a more comprehensive assessment of septal deviations than just identifying individual septal pathologies alone. Investigating risk factors for revision septoplasty is necessary to recognize complex cases and consequently adapt surgical techniques to improve the individual patient’s outcome and counseling.
Author Contributions
Conceptualization, K.B., D.T.L., G.B. and C.A.M.; methodology, K.B. and D.T.L.; software, K.B. and D.T.L.; validation, D.T.L. and C.A.M.; formal analysis, K.B. and D.T.L.; investigation, M.H., J.B.-P. and F.F.B.; resources, D.T.L. and K.B.; data curation, J.B.-P. and K.B.; writing—original draft preparation, K.B.; writing—review and editing, D.T.L. and K.B.; visualization, K.B.; supervision, D.T.L.; project administration, D.T.L., K.B. and C.A.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Medical University of Vienna (Approval number: 1737/2020).
Informed Consent Statement
Patient consent was waived due to retrospective data collection.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to ongoing research.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- van Egmond, M.M.H.T.; Rovers, M.M.; Tillema, A.H.J.; van Neerbeek, N. Septoplasty for nasal obstruction due to a deviated nasal septum in adults: A systematic review. Rhinology 2018, 56, 195–208. [Google Scholar] [CrossRef] [PubMed]
- Manoukian, P.D.; Wyatt, J.R.; Leopold, D.A.; Bass, E.B. Recent Trends in Utilization of Procedures in Otolaryngology-Head and Neck Surgery. Laryngoscope 1997, 107, 472–477. [Google Scholar] [CrossRef] [PubMed]
- Youn, G.M.; Shah, J.P.; Wei, E.X.; Kandathil, C.; Most, S.P. Revision Rates of Septoplasty in the United States. Facial Plast. Surg. Aesthetic Med. 2023, 25, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, T.R.; Shakeel, M.; Al-Adhami, A.; Suhailee, S.; Ram, B.; Ah-See, K.W. Revision nasal surgery after septoplasty: Trainees versus trainers. Eur. Arch. Oto-Rhino-Laryngol. 2013, 270, 3063–3067. [Google Scholar] [CrossRef] [PubMed]
- Gillman, G.S.; Egloff, A.M.; Rivera-Serrano, C.M. Revision septoplasty: A prospective disease-specific outcome study. Laryngoscope 2014, 124, 1290–1295. [Google Scholar] [CrossRef] [PubMed]
- van Egmond, M.M.H.T.; Rovers, M.M.; Hannink, G.; Hendriks, C.T.M.; van Heerbeek, N. Septoplasty with or without concurrent turbinate surgery versus non-surgical management for nasal obstruction in adults with a deviated septum: A pragmatic, randomised controlled trial. Lancet 2019, 394, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Erdivanli, O.C.; Coskun, Z.O.; Ozgur, A.; Ogurlu, M.; Demirci, M.; Dursun, E. Comparison of Quality of Life Before and After Septoplasty With Short Form-36. J. Craniofac. Surg. 2020, 31, 832–835. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, J.; Certal, V.; Chang, E.T.; Camacho, M. Nasal Septal Deviations: A Systematic Review of Classification Systems. Plast. Surg. Int. 2016, 2016, 7089123. [Google Scholar] [CrossRef] [PubMed]
- Lawson, V.G. Management of the twisted nose. J. Otolaryngol. 1978, 7, 56–66. [Google Scholar] [PubMed]
- Mladina, R.; Cujić, E.; Subarić, M.; Vuković, K. Nasal septal deformities in ear, nose, and throat patients: An international study. Am. J. Otolaryngol. 2008, 29, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Baumann, I.; Baumann, H. A new classification of septal deviations. Rhinology 2007, 45, 220–223 PMID: 17956023. [Google Scholar] [PubMed]
- Jin, H.R.; Kim, D.W.; Jung, H.J. Common Sites, Etiology, and Solutions of Persistent Septal Deviation in Revision Septoplasty. Clin. Exp. Otorhinolaryngol. 2018, 11, 288–292. [Google Scholar] [CrossRef] [PubMed]
- Most, S.P.; Rudy, S.F. Septoplasty: Basic and Advanced Techniques. Facial Plast. Surg. Clin. N. Am. 2017, 25, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Haack, J.; Papel, I.D. Caudal Septal Deviation. Otolaryngol. Clin. N. Am. 2009, 42, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.S.; Dobratz, E.J.; Stowell, N.; Barker, D.; Park, S.S. Revision septoplasty: Review of sources of persistent nasal obstruction. Am. J. Rhinol. 2008, 22, 440–444. [Google Scholar] [CrossRef] [PubMed]
- Schultz-Coulon, H.-J. Comments on septoplasty. HNO 2006, 54, 59–69, quiz 70. [Google Scholar] [CrossRef] [PubMed]
- Dąbrowska-Bień, J.; Skarżyński, P.H.; Gwizdalska, I.; Łazęcka, K.; Skarżyński, H. Complications in septoplasty based on a large group of 5639 patients. Eur. Arch. Oto-Rhino-Laryngol. 2018, 275, 1789–1794. [Google Scholar] [CrossRef] [PubMed]
- Ketcham, A.S.; Han, J.K. Complications and management of septoplasty. Otolaryngol. Clin. N. Am. 2010, 43, 897–904. [Google Scholar] [CrossRef] [PubMed]
- Şevik Eliçora, S.; Erdem, D.; Işık, H.; Damar, M.; Dinç, A.E. Difficult septal deviation cases: Open or closed technique? Braz. J. Otorhinolaryngol. 2017, 83, 256–260. [Google Scholar] [CrossRef] [PubMed]
- Costache, A.; Berghi, O.N.; Cergan, R.; Dumitru, M.; Neagos, A.; Popa, L.G.; Giurcaneanu, C.; Vrinceanu, D. Respiratory allergies: Salicaceae sensitization (Review). Exp. Ther. Med. 2021, 21, 609. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).