Case Report and Literature Review on Tongue Schwannoma
Abstract
1. Introduction
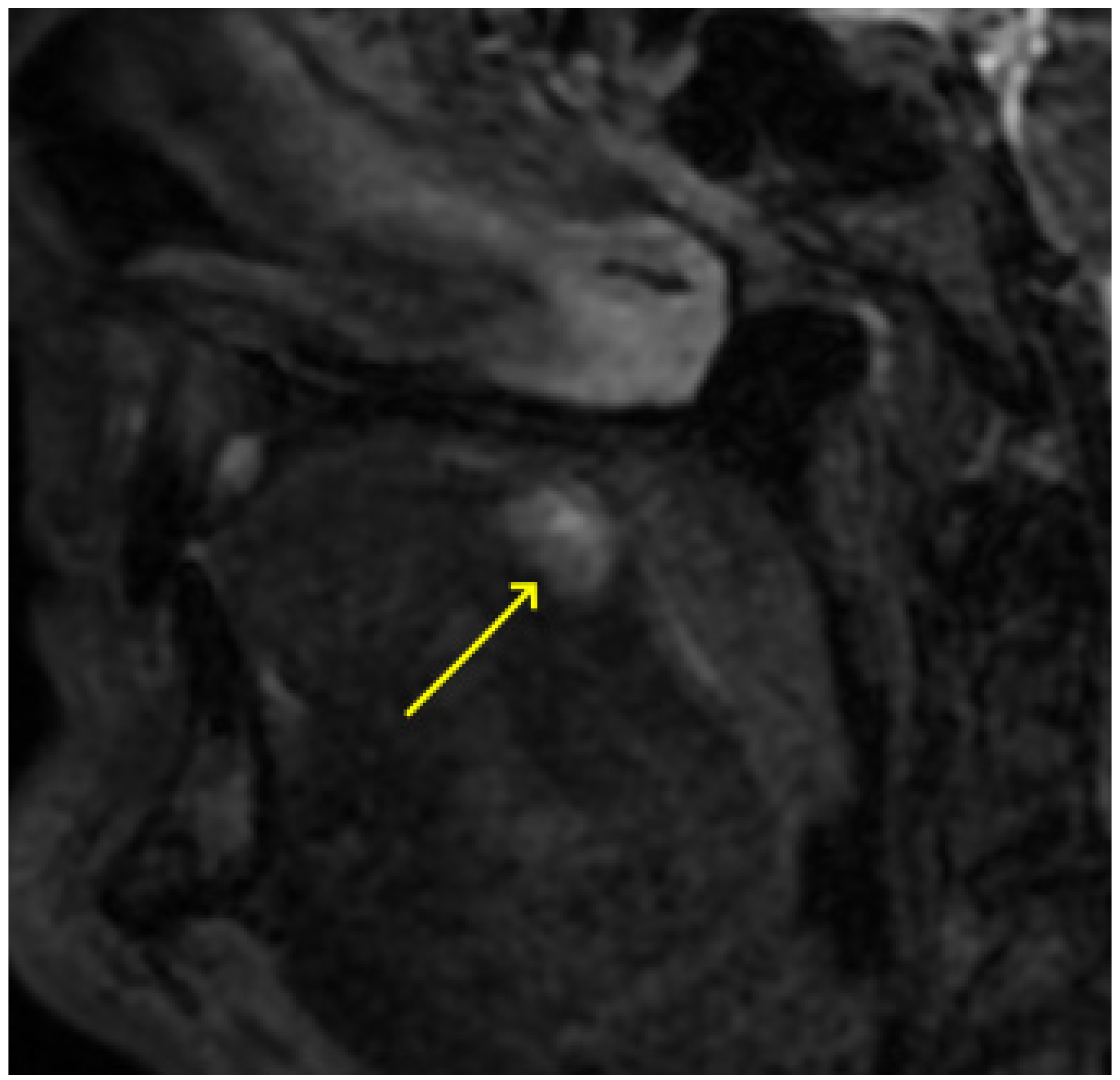
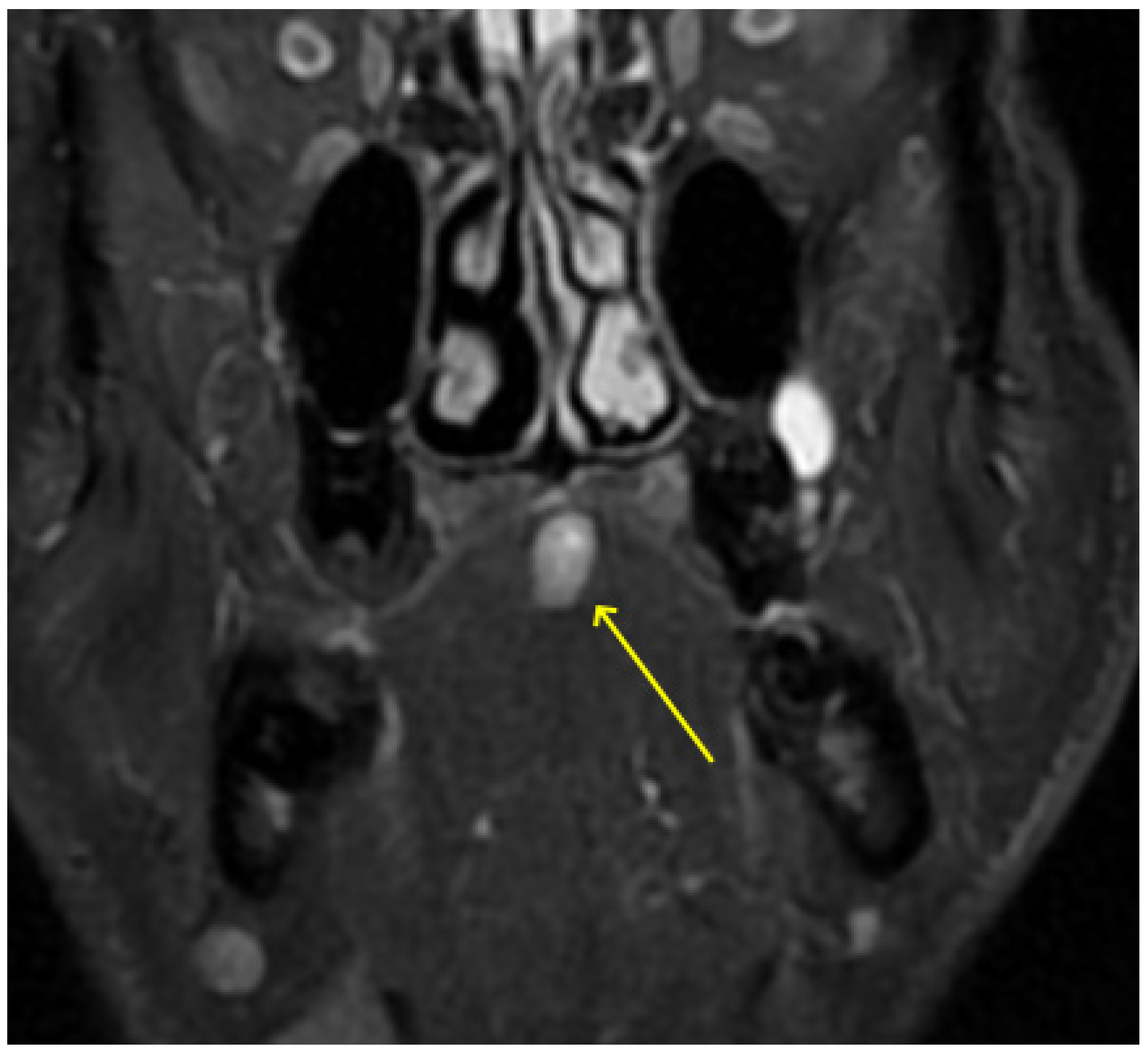
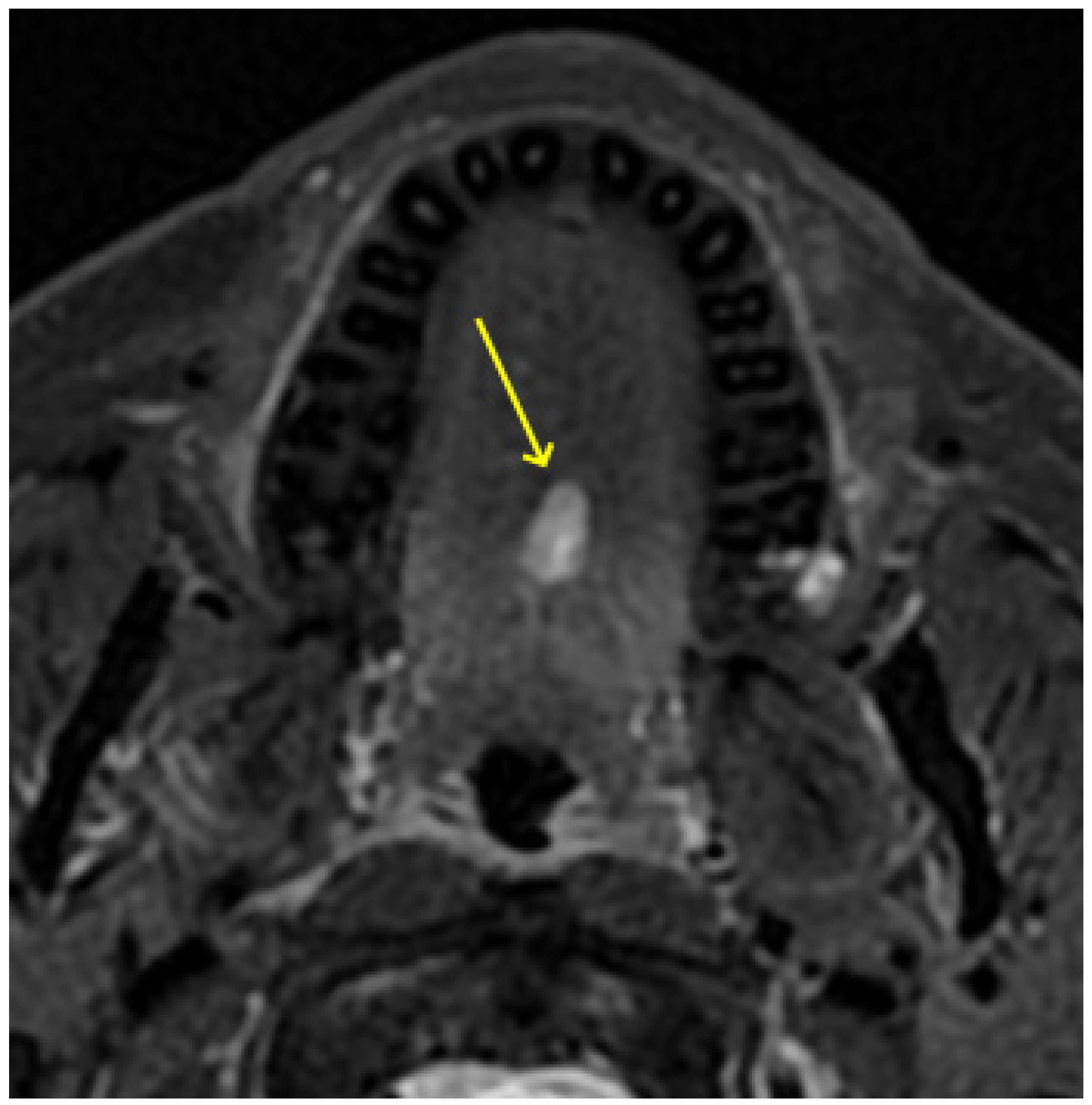
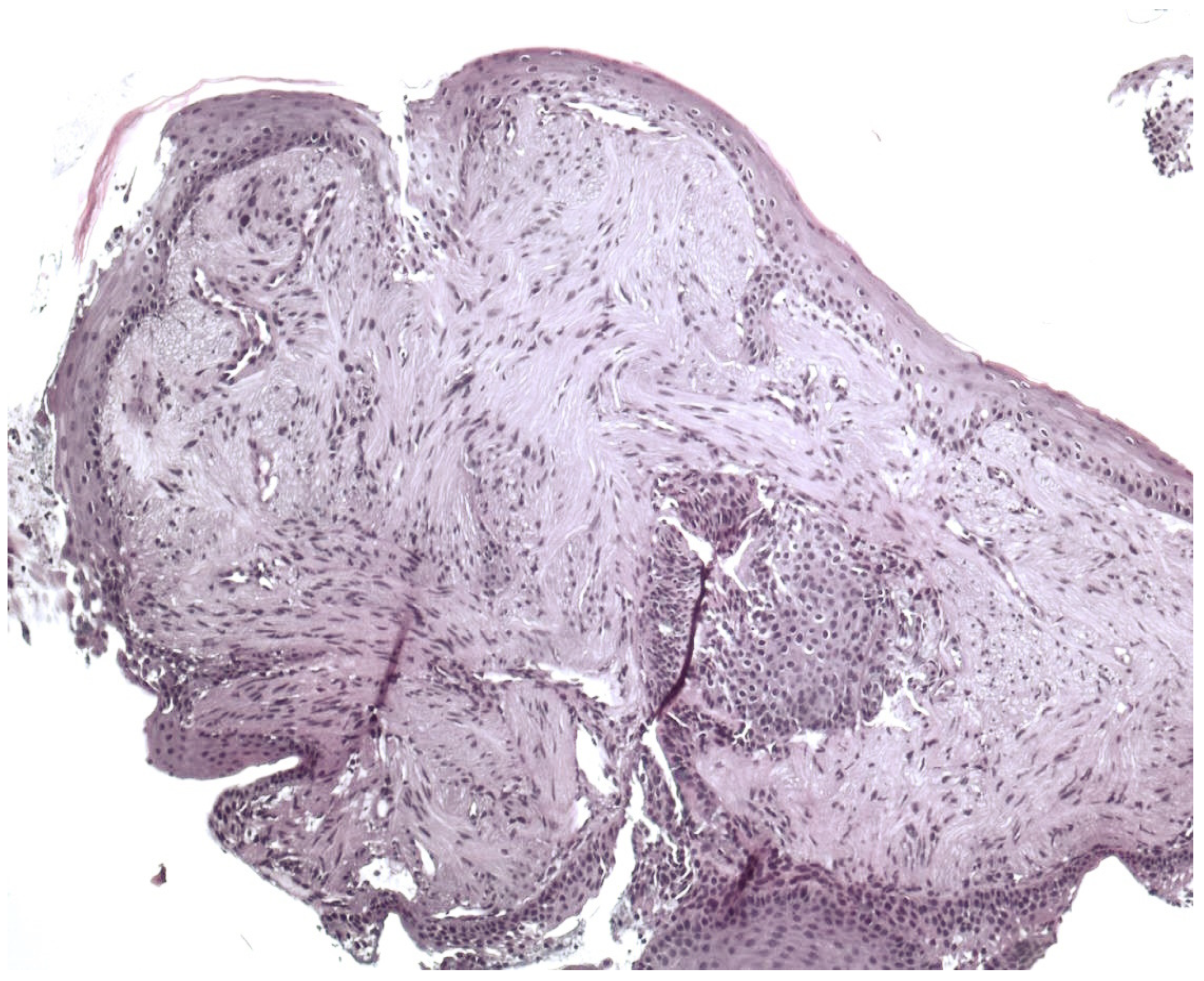
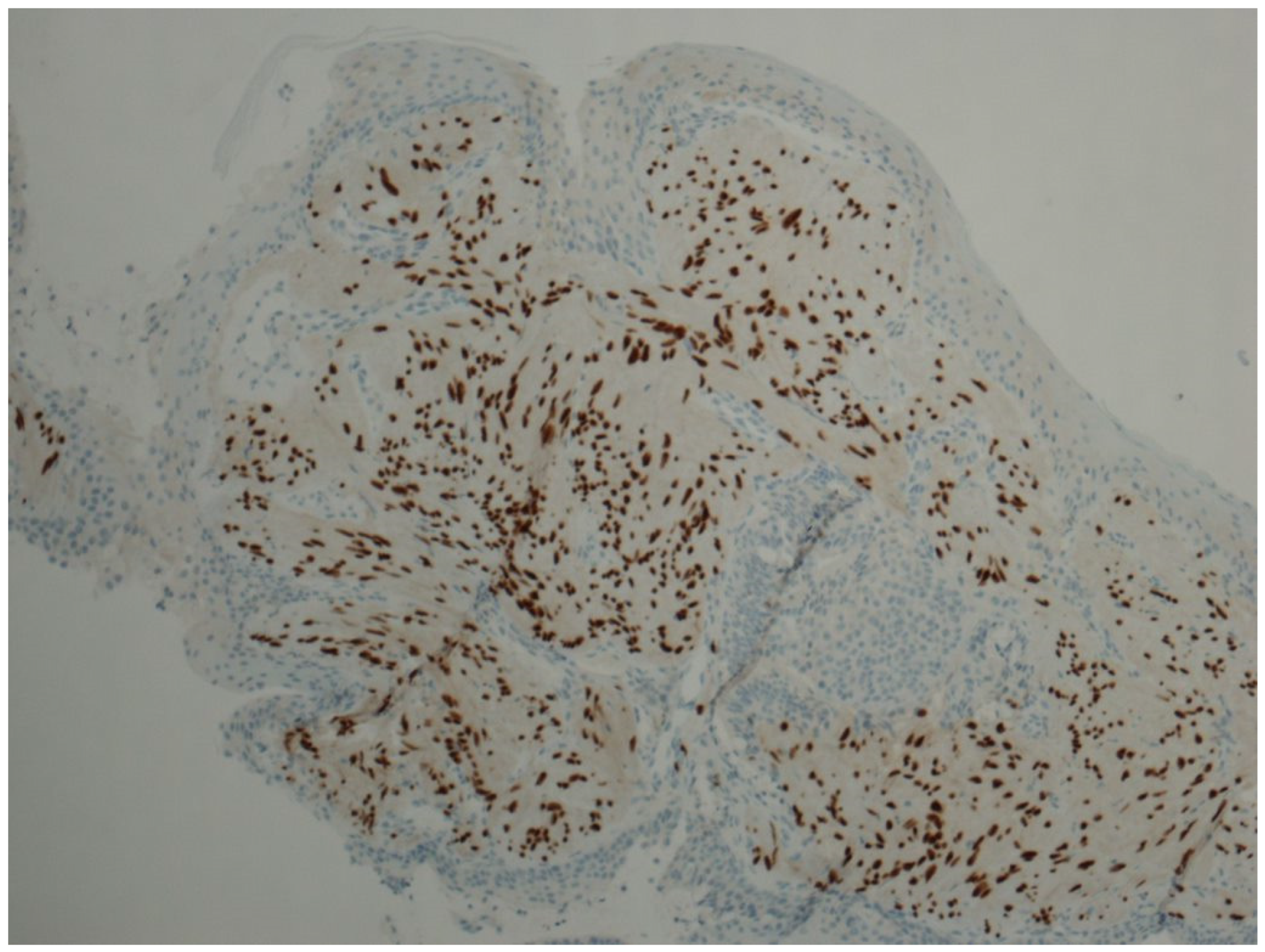
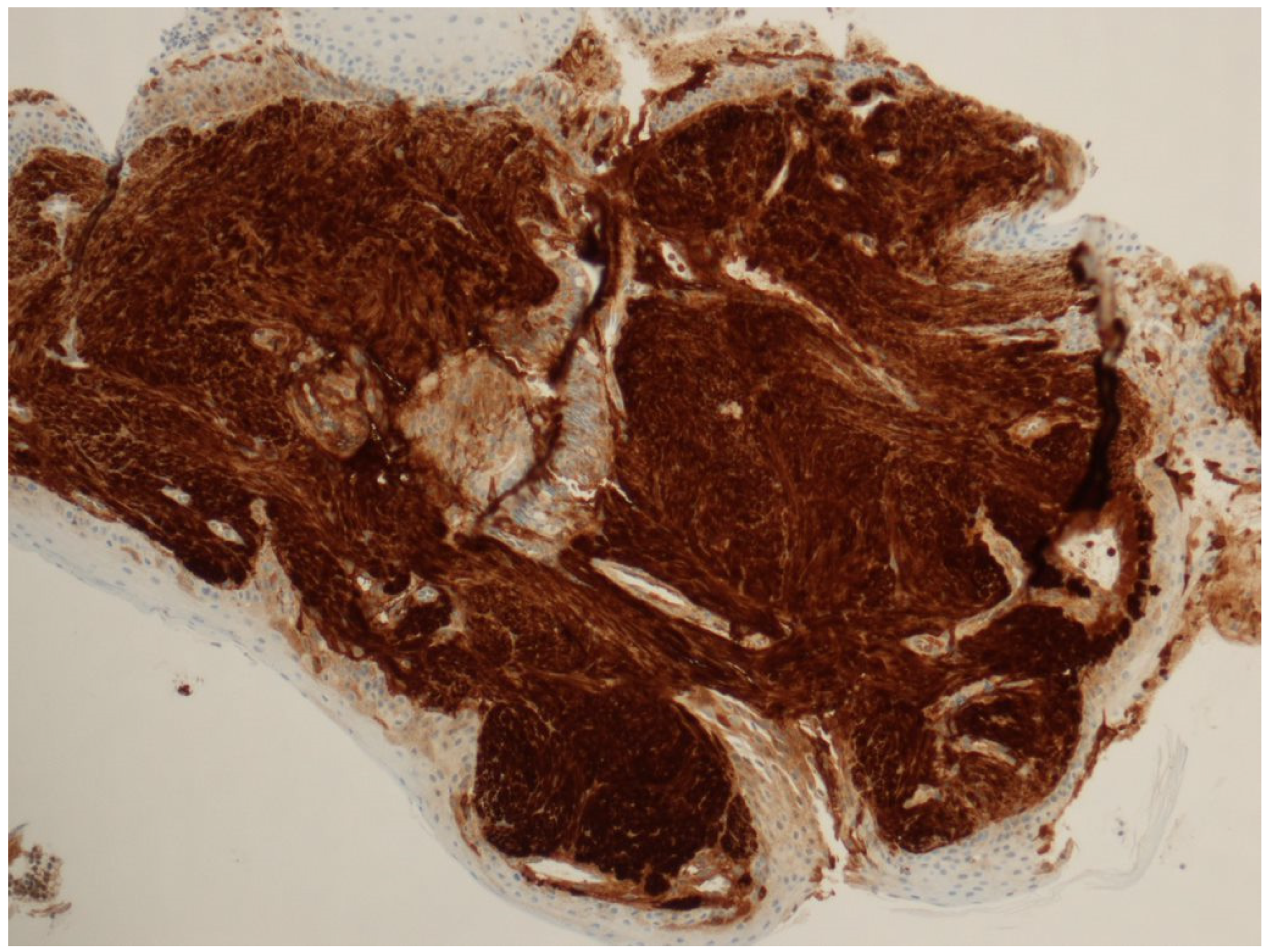
2. Detailed Case Description
3. Discussion
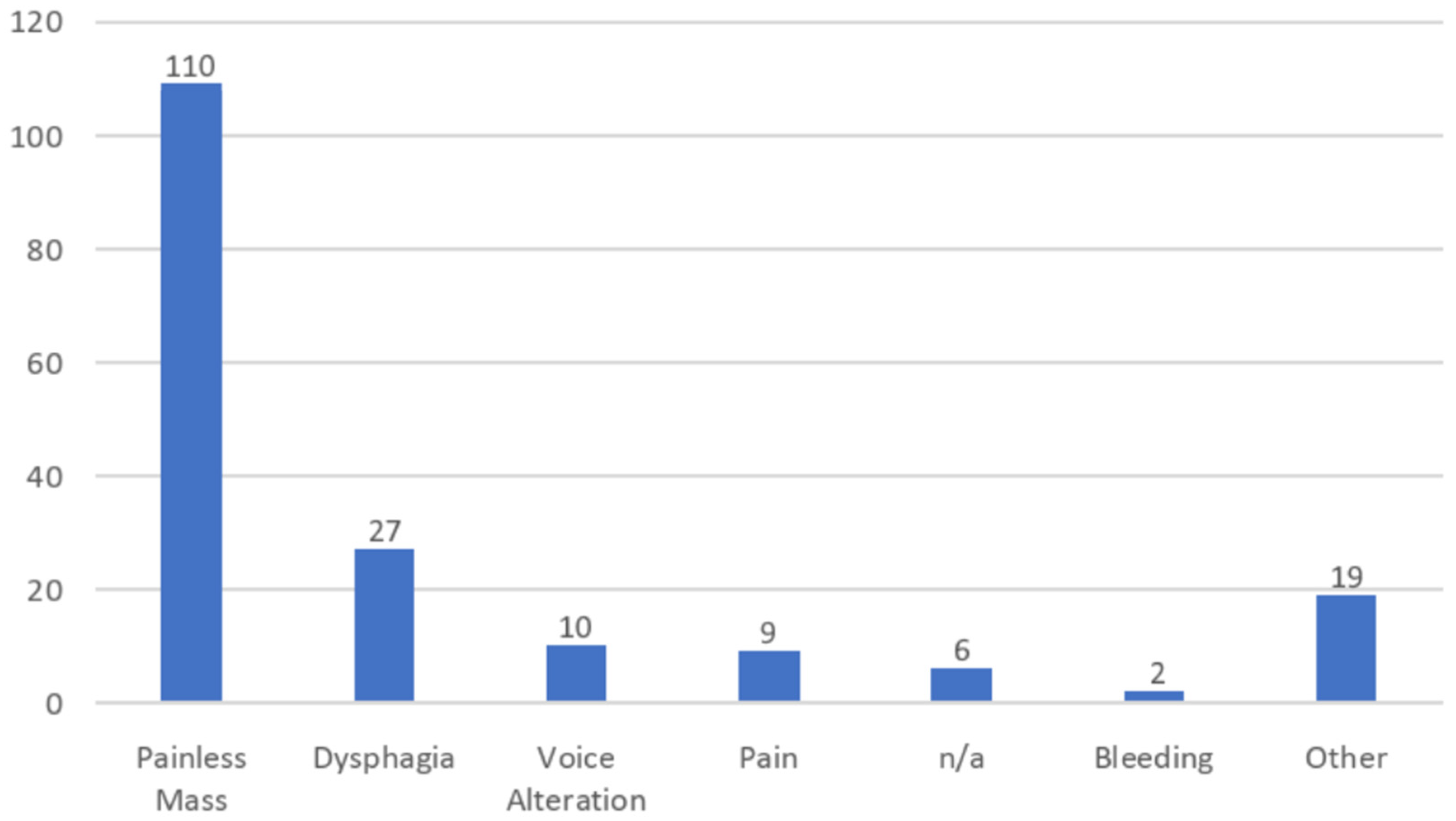
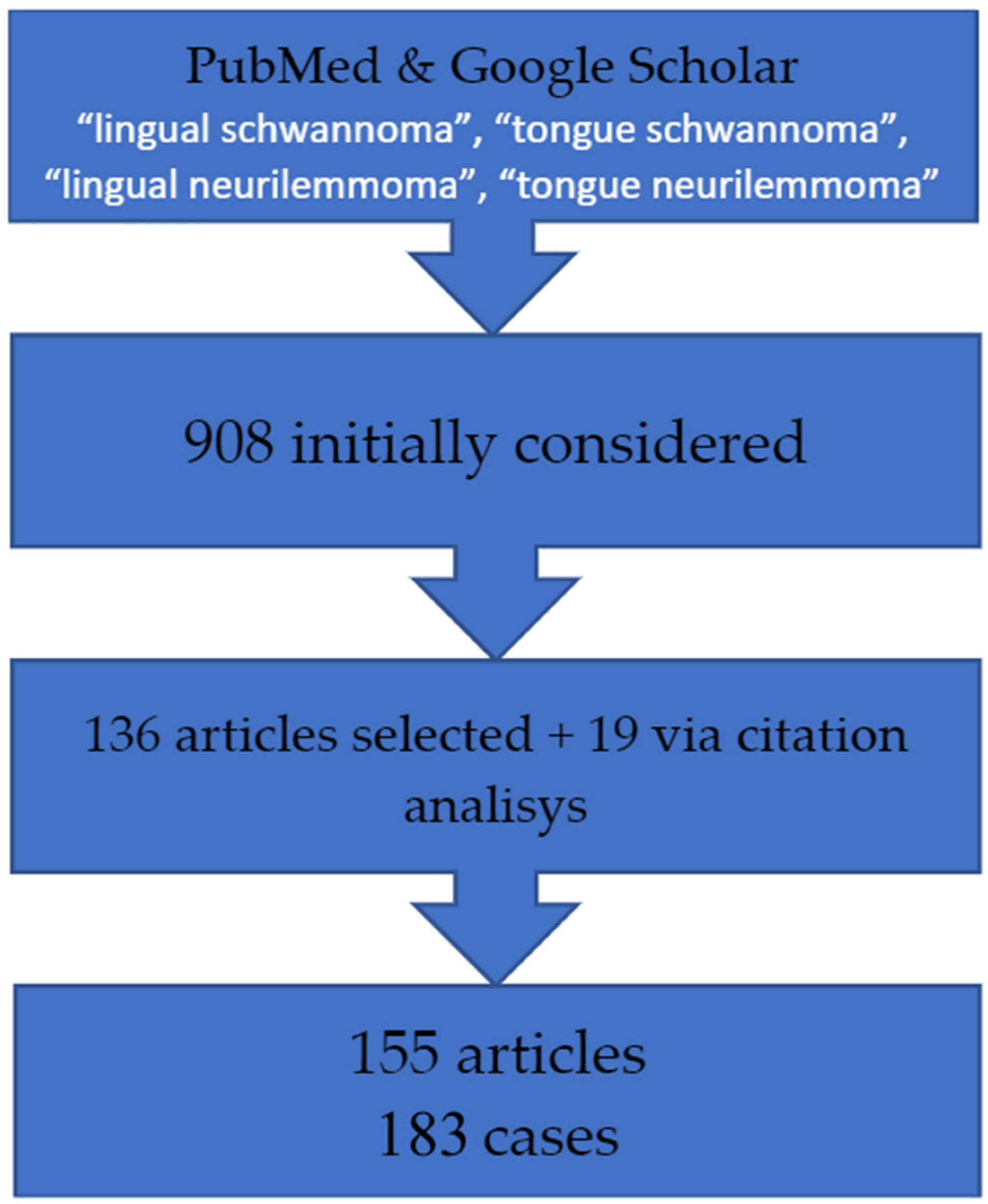
3.1. Literature Review
3.2. Pathology Presentation


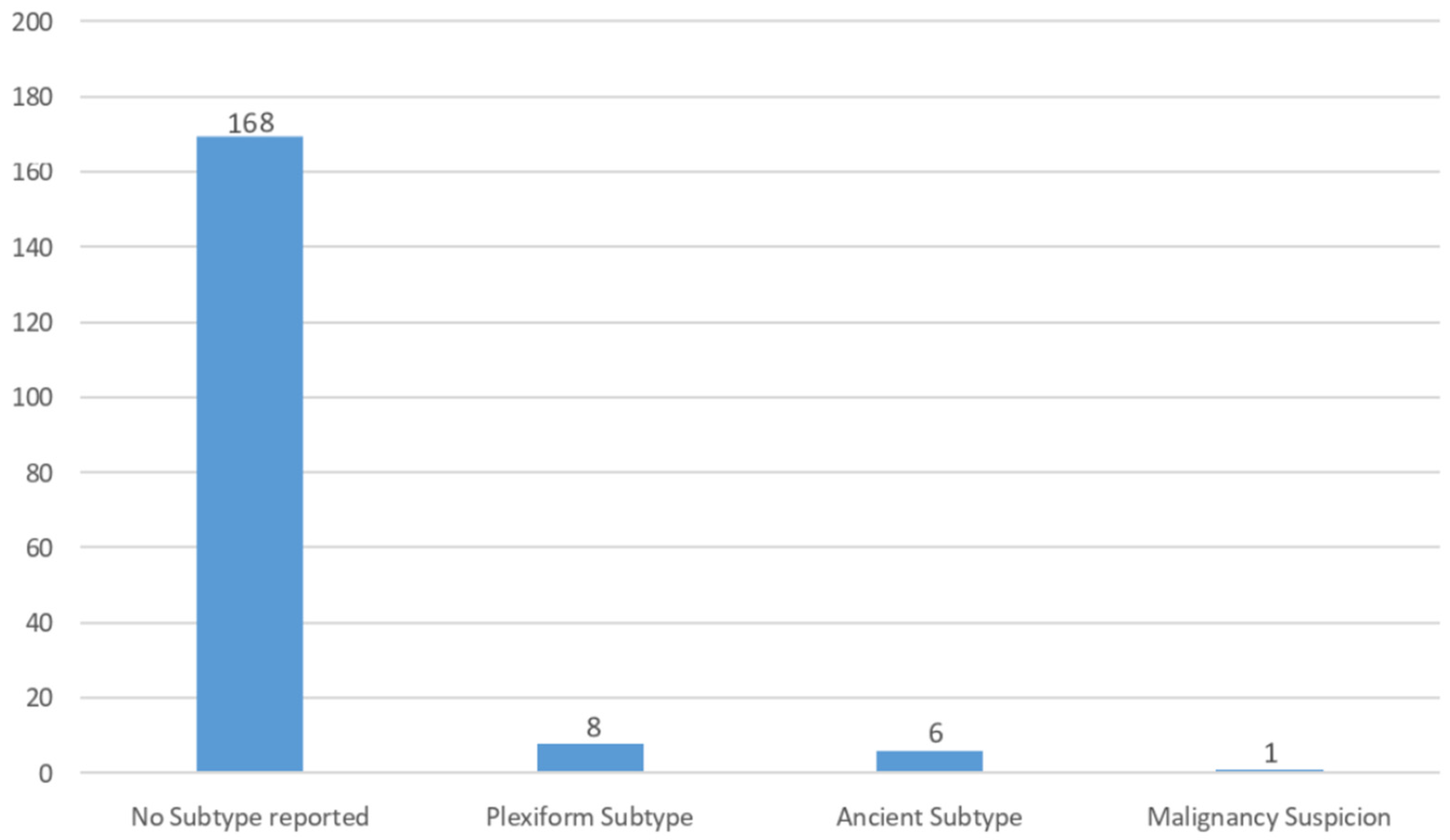
3.3. Histological Variants
3.4. Surgery and Anaesthesia Techniques
3.5. Strengths and Limitations
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Verocay, J. Zur Kennntnis der ‘neurofibrome’. Beitr. Pathol. Anat. 1910, 48, 1–69. [Google Scholar]
- Hilton, D.A.; Hanemann, C.O. Schwannomas and their pathogenesis. Brain Pathol. 2014, 24, 205–220. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Akheel, M.; Athar, I.M.; Ashmi, W. Schwannomas of the head and neck region: A report of two cases with a narrative review of the literature. Cancer Res. Stat. Tr. 2020, 3, 517–525. [Google Scholar] [CrossRef]
- Batsakis, J.G.; Sneige, N. Parapharyngeal and retropharyngeal space diseases. Ann. Otol. Rhinol. Laryngol. 1989, 98 Pt 1, 320–321. [Google Scholar] [CrossRef] [PubMed]
- Magro, G.; Broggi, G.; Angelico, G.; Puzzo, L.; Vecchio, G.M.; Virzì, V.; Salvatorelli, L.; Ruggieri, M. Practical Approach to Histological Diagnosis of Peripheral Nerve Sheath Tumors: An Update. Diagnostics 2022, 12, 1463. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Woertler, K. Tumors and tumor–like lesions of peripheral nerves. Semin. Musculoskelet. Radiol. 2010, 14, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Alexiev, B.A.; Chou, P.M.; Jennings, L.J. Pathology of Melanotic Schwannoma. Arch. Pathol. Lab. Med. 2018, 142, 1517–1523. [Google Scholar] [CrossRef] [PubMed]
- Carney, J.A. Psammomatous melanotic schwannoma. A distinctive, heritable tumor with special associations, including cardiac myxoma and the Cushing syndrome. Am. J. Surg. Pathol. 1990, 14, 206–222. [Google Scholar] [CrossRef] [PubMed]
- Thakur, V.K.; Rahul, S.K.; Kumar, B.; Hasan, Z.; Yadav, R.; Chaubey, D.; Prasad, R.; Keshri, R. Lingual schwannoma in a 4-year-old female baby. J. Indira Gandhi Inst. Med. Sci. 2021, 7, 64–66. [Google Scholar] [CrossRef]
- Crippa, R.; Angiero, F.; Calcagnile, F.; Stefani, M. Diode Laser Surgery on Schwannoma of the Tongue: Case Report. J. Oral Laser Appl. 2004, 4, 285–289. [Google Scholar]
- Al–Mahdi, A.H.; Al-Khurrhi, L.E.; Atto, G.Z.; Dhaher, A. Plexiform Hypoglossal Schwannoma of the Tongue and the Submandibular Region. J. Craniofacial Surg. 2012, 23, 1563–1565. [Google Scholar] [CrossRef]
- Nakayama, H.; Gobara, Y.; Shimamoto, F.; Kajihara, H. Ancient Schwannoma of the Oral Floor and Ventricular Portion of the Tongue: A Case Report and Review of the Literature. Jpn. J. Clin. Onc. 1996, 26, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Bilici, S.; Akpınar, M.; Yiğit, O.; Günver, F. Ancient schwannoma of the tongue: A case report. Kulak Burun Bogaz Ihtis Derg. 2011, 21, 234–236. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Guledgud, M.V.; Degala, S.; Patil, K.; Maruthi, M. Ancient Schwannoma of the tongue. J. Med. Radiol. Pathol. Surg. 2016, 2, 20–23. [Google Scholar] [CrossRef]
- Shashikumar, T.; Tejaswini, J.S.; Bellad, S.; Hajare, P.S.; Mudhol, R.S.; Soni, S.; Pathak, K. Ancient Schwannoma: A Rare Intramural Intra-Lingual Lesion. Indian J. Otolaryngol. Head Neck Surg. 2019, 71 (Suppl. S1), 816–819. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Miniksar, O.H.; Kayhan, G.E.; Toy, E.; Demir, I. Anesthesia management of a patient with schwannoma of tongue base. Ann. Med. Res. 2019, 26, 1436–1437. [Google Scholar] [CrossRef]
- Yaslikaya, S.; Kizilay, A.; Şamdanci, E. Endoscopic Transoral Resection of Tongue Base Ancient Schwannoma. J. Craniofacial Surg. 2020, 31, e409–e411. [Google Scholar] [CrossRef] [PubMed]
- Nisa, L.; von Büren, T.; Tiab, A.; Giger, R. Giant plexiform schwannoma of the tongue. Case Rep. Otolaryngol. 2011, 2011, 762524. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chi, A.C.; Neville, B.W.; Cheng, L. Plexiform Schwannoma of the Oral Cavity: Report of Eight Cases and a Review of the Literature. Head Neck Pathol. 2021, 15, 288–297. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Behrad, S.; Sohanian, S.; Ghanbarzadegan, A. Solitary intraosseous neurofibroma of the mandible: Report of an extremely rare histopathologic feature. Indian J. Pathol. Microbiol. 2020, 63, 276–278. [Google Scholar]
- Amer, S.M.; Ukudeyeva, A.; Pine, H.S.; Campbell, G.A.; Clement, C.G. Plexiform Schwannoma of the Tongue in a Pediatric Patient with Neurofibromatosis Type 2: A Case Report and Review of Literature. Case Rep. Pathol. 2018, 2018, 9814591. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Patel, N.N.; Upile, T.; Zaman, A.; Chowdhury, C.R.; Bhattacharyya, A.K. Malignant schwannoma of the lingual nerve: A case report. Indian J. Otolaryngol. Head Neck Surg. 2000, 52, 382–385. [Google Scholar] [CrossRef] [PubMed]
- Petruzzi, G.; Costantino, A.; Arosio, A.D.; De Virgilio, A.; Pichi, B.; Zocchi, J.; Mercante, G.; Spriano, G.; Pellini, R. Transoral Robotic Surgery in the Management of a Tongue Base Schwannoma. J. Craniofacial Surg. 2020, 31, e411–e413. [Google Scholar] [CrossRef] [PubMed]
- Ballesteros, F.; Vilaseca, I.; Blanch, J.L.; Gaspa, A.; Bernal-Sprekelsen, M. Base of tongue neurilemmoma: Excision by transoral laser microsurgery. Acta Otolaryngol. 2007, 127, 1005–1007. [Google Scholar] [CrossRef] [PubMed]
- Munjal, M.; Arora, A.; Singh, D.; Talwar, G.; Nagpal, J. Lingual Schwannoma: A Case Report. Ann. Appl. Bio-Sci. 2017, 4, C16–C17, ISSN: 2455-0396 (print), ISSN: 2349-6991 (electronic). [Google Scholar] [CrossRef][Green Version]
- de Bree, R.; Westerveld, G.J.; Smeele, L.E. Submandibular approach for excision of a large schwannoma in the base of the tongue. Eur. Arch. Otorhinolaryngol. 2000, 257, 283–286. [Google Scholar] [CrossRef] [PubMed]
- Sawhney, R.; Carron, M.A.; Mathog, R.H. Tongue base schwannoma: Report, review, and unique surgical approach. Am. J. Otolaryngol. 2008, 29, 119–122. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.B.; Labrador, A.J.; Molina, R.; Kessler, H.P. Oral and maxillofacial pathology case of the month: Schwannoma. Tex. Dent. J. 2017, 134, 10–61. [Google Scholar] [PubMed]
- George, N.A.; Wagh, M.; Balagopal, P.G.; Gupta, S.; Sukumaran, R.; Sebastian, P. Schwannoma base tongue: Case report and review of literature. Gulf J. Oncolog. 2014, 1, 94–100. [Google Scholar] [PubMed]
- Medhi, J.; Laskar, H.A.; Das, D.J.; Shunyu, N.B.; Jitani, A.; Raphael, V.; Thabah, R. Management of Large Tongue Schwannoma—A Short Report. Iran J. Otorhinolaryngol. 2016, 28, 168. [Google Scholar] [PubMed] [PubMed Central]
- Kurup, S.; Thankappan, K.; Krishnan, N.; Nair, P.P. Intraoral schwannoma—A report of two cases. BMJ Case Rep. 2012, 2012, bcr1220115389. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tandon, S.; Meher, R.; Chopra, A.; Raj, A.; Wadhwa, V.; Mahajan, N.; Jain, A. Tongue Base Schwannoma. Indian J. Otolaryngol. Head Neck Surg. 2019, 71 (Suppl. S1), 70–73. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ying, Y.L.; Zimmer, L.A.; Myers, E.N. Base of tongue schwannoma: A case report. Laryngoscope 2006, 116, 1284–1287. [Google Scholar] [CrossRef] [PubMed]
- Hsu, Y.C.; Hwang, C.F.; Hsu, R.F.; Kuo, F.Y.; Chien, C.Y. Schwannoma (neurilemmoma) of the tongue. Acta Otolaryngol. 2006, 126, 861–865. [Google Scholar] [CrossRef] [PubMed]
- Chandak, N.K.; Harkut, R.R. Neurilemmoma of Posterior Third of Tongue. Ind. J. Otol. 1972, XXIV, 118–120. [Google Scholar] [CrossRef]
- Diplan, J.; Cavallo, P.; de Los Santos, S. Anterior Midline Glossotomy Approach for Large Schwannoma of the Tongue: Case Report. Clin. Med. Insights Ear Nose Throat 2018, 11, 1179550618786935. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Moussa, M.A.; Ahmed, M.E.; Hamed, M.A.; Ahmed, A.R. Transoral approach of Tongue base schwannoma. Laryngo-Rhino-Otologie 2019, 98, 11045. [Google Scholar]
- Batra, U.B.; Usha, G.; Gogia, A.R. Anesthetic management of schwannoma of the base of the tongue. J. Anaesthesiol. Clin. Pharmacol. 2011, 27, 241–243. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Scarano, A.; Murmura, G.; Artese, L.; Carinci, F.; Lauritano, D. Schwannoma of the posterior tongue in a thirteen-year old child. Eur. J. Inflamm. 2012, 10, 43–47. [Google Scholar]
- Erkul, E.; Cıncık, H.; Haholu, A.; Çekin, E.; Güngör, A. Schwannoma of the tongue: A report of two cases and review. Gulhane Med. J. 2013, 55, 135–140. [Google Scholar] [CrossRef]
- Bhola, N.; Jadhav, A.; Borle, R.; Khemka, G.; Bhutekar, U.; Kumar, S. Schwannoma of the tongue in a paediatric patient: A case report and 20-year review. Case Rep. Dent. 2014, 2014, 780762. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rana, S.S.; Ohri, N. Schwannoma of the base of the tongue mimicking fibroma. SRM J. Res. Dent. Sci. 2018, 9, 202–204. [Google Scholar] [CrossRef]
- Ahmed, S.; Al Dayel, O.; Tabassum, N.; Al Qanabr, M.H.; Ali, H.A.; Mathekor, N.; Albannawi, G.A.; Al Taqi, F.Z.; Al Shehri, A.H.; Shaker, S.M. Lingual schwannoma in an adolescent girl—A diagnostic challenge. J. Fam. Med. Prim. Care 2020, 9, 1775–1777. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sayad, Z. Lingual Schwannoma: A Diagnostic to Remember. A Case Report with Review of Literature. Sch. J. App. Med. Sci. 2021, 3, 309–311. [Google Scholar] [CrossRef]
- Stout, A.P.; Carson, W. The periferal manifestation of the specific nerve sheat tumor (neurilemoma). Amer. J. Can. 1935, 24, 751–780. [Google Scholar] [CrossRef]
- Robertson, A.S. Neurilemmoma of the tongue. Br. J. Surg. 1952, 40, 284–285. [Google Scholar] [CrossRef] [PubMed]
- Cameron, I.W. A case of neurilemmoma (schwannoma) of the tongue. Oral Surg. Oral Med. Oral Pathol. 1959, 12, 1464–1467. [Google Scholar] [CrossRef] [PubMed]
- Mercantini, E.S.; Mopper, C. Neurilemmoma of the Tongue. AMA Arch. Derm. 1959, 79, 542–544. [Google Scholar] [CrossRef] [PubMed]
- Chadwick, D.L. Neurilemmoma of the Tongue. J. Laryngol. Otol. 1964, 78, 959–962. [Google Scholar] [CrossRef]
- Craig, D. Neurilemmoma of the tongue. Arch. Dis. Child. 1964, 39, 297–298. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chhatbar, D.R. A Case of Neurilemmoma of the Tongue. J. Laryngol. Otol. 1965, 79, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Pantazopoulos, P.E. Schwannomas of nose, oral cavity and pharynx. Acta Otolaryngol. 1965, 60, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Firfer, H.; Sohn, D.; Heurlin, R.; Stuteville, O.H. Neurilemmoma of the tongue. Oral Surg. Oral Med. Oral Pathol. 1966, 21, 139–142. [Google Scholar] [CrossRef] [PubMed]
- Hatziotis, J.C.; Asprides, H. Neurilemoma (schwannoma) of the oral cavity. Oral Surg. Oral Med. Oral Pathol. 1967, 24, 510–526. [Google Scholar] [CrossRef] [PubMed]
- Oles, R.D.; Wertheimer, F.W. Case report: Neurilemmoma of the tongue. J. Mich. State Dent. Assoc. 1967, 49, 7–8. [Google Scholar] [PubMed]
- Paliwal, Y.D.; Kapur, V.L.; Singh, R.P. Neurilemoma of the tongue: Case report. Int. Surg. 1967, 47, 503–506. [Google Scholar] [PubMed]
- Crawford, W.H., Jr.; Korchin, L.; Greskovich, F.J., Jr. Neurilemmomas of the oral cavity: Report of five cases. J. Oral Surg. 1968, 26, 651–658. [Google Scholar] [PubMed]
- Bititci, O.Ö. Neurilemmoma of the Tongue. J. Laryngol. Otol. 1969, 83, 201–204. [Google Scholar] [CrossRef] [PubMed]
- Gupta, T.K.; Brasfield, R.D.; Strong, E.W.; Hajdu, S.I. Benign solitary schwannomas (neurilemomas). Cancer 1969, 24, 355–366. [Google Scholar] [CrossRef]
- Eversole, L.R.; Howell, R.M. Ancient neurilemmoma of the oral cavity. Oral Surg. Oral Med. Oral Pathol. 1971, 32, 440–443. [Google Scholar] [CrossRef] [PubMed]
- Sinha, S.N.; Samuel, K.C. Neurilemmoma of tongue. J. Laryngol. Otol. 1971, 85, 623–626. [Google Scholar] [CrossRef] [PubMed]
- Mosadomi, A. Neurilemmoma of the tongue. J. Oral Med. 1975, 30, 44–46. [Google Scholar] [PubMed]
- Swangsilpa, K.; Winther, J.E.; Nybroe, L. Neurilemmomas in the oral cavity. J. Dent. 1976, 4, 237–241. [Google Scholar] [CrossRef] [PubMed]
- Sharan, R.; Akhtar, M.P. Neurilemmoma of tongue. J. Indian Med. Assoc. 1978, 71, 290–291. [Google Scholar] [PubMed]
- Chari, P.S.; Balakrishnan, C. Neurilemmoma of the base of the tongue. Indian J. Otolaryngol. 1979, 31, 133. [Google Scholar] [CrossRef]
- Barbosa, J.; Hansen, L.S. Solitary multilobular schwannoma of the oral cavity. J. Oral Med. 1984, 39, 232–235. [Google Scholar] [PubMed]
- Chanduri, J.N.; Banerjee, S.; Chatterji, P.; Khatri, B.B. Neurilemmoma of the Tongue. Indian J. Otolaryngol. 1985, 37, 167–168. [Google Scholar]
- Akimoto, Y.; Yamamoto, H.; Nishimura, H.; Komiya, M.; Kaneko, K. Neurilemmoma in the oral cavity. J. Nihon Univ. Sch. Dent. 1987, 29, 203–205. [Google Scholar] [CrossRef] [PubMed]
- Malden, N.J. Neurilemmoma of the tongue. Dent Update 1988, 15, 170. [Google Scholar] [PubMed]
- Siar, C.H.; Ng, K.H.; Chia, T.Y.; Kulkarni, M.G. Atypical neurilemmomas of the tongue––Report of two cases. Singap. Med. J. 1988, 29, 83–85. [Google Scholar] [PubMed]
- Flickinger, F.W.; Lozano, R.L.; Yuh, W.T.C.; Sachs, M.A. Neurilemoma of the Tongue: MR Findings. J. Comput. Assist. Tomogr. 1989, 13, 886–888. [Google Scholar] [CrossRef] [PubMed]
- Talmi, Y.P.; Gal, R.; Finkelstein, Y.; Shvilli, Y.; Zohar, Y. Pathologic quiz case 1. Benign Schwannoma of tongue. Arch. Otolaryngol. Head Neck Surg. 1991, 117, 926–928. [Google Scholar] [PubMed]
- Kumar, S.; Kochhar, L.K.; De Ka, R.C. Neurilemmoma of the tongue. Ind. J. Otolaryngol. 1991, 43, 28–29. [Google Scholar] [CrossRef]
- López, J.I.; Ballestin, C. Intraoral schwannoma. A clinicopathologic and immunohistochemical study of nine cases. Arch. Anat. Cytol. Pathol. 1993, 41, 18–23. [Google Scholar] [PubMed]
- Williams, H.K.; Cannell, H.; Silvester, K.; Williams, D.M. Neurilemmoma of the head and neck. Br. J. Oral Maxillofac. Surg. 1993, 31, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Haring, J.I. Case #10. Neurilemoma. RDH 1994, 14, 12. [Google Scholar] [PubMed]
- Verghese, S.; Rupa, V.; Kurian, S. Schwannoma of the base of tongue. IJO HNS 1996, 48, 228–229. [Google Scholar] [CrossRef]
- Spandow, O.; Fagerlund, M.; Bergmark, L.; Boquist, L. Clinical and histopathological features of a large parapharyngeal neurilemmoma located at the base of the tongue. ORL J. Otorhinolaryngol. Relat. Spec. 1999, 61, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Pfeifle, R.; Baur, D.A.; Paulino, A.; Helman, J. Schwannoma of the tongue: Report of 2 cases. J. Oral Maxillofac. Surg. 2001, 59, 802–804. [Google Scholar] [CrossRef] [PubMed]
- Mevio, E.; Gorini, E.; Lenzi, A.; Migliorini, L. Schwannoma of the tongue: One case report. Rev. Laryngol. Otol. Rhinol. 2002, 123, 259–261. [Google Scholar] [PubMed]
- Arda, H.N.; Akdogan, O.; Arda, N.; Sarikaya, Y. An unusual site for an intraoral schwannoma: A case report. Am. J. Otolaryngol. 2003, 24, 348–350. [Google Scholar] [CrossRef] [PubMed]
- Pahwa, R.; Khurana, N.; Chaturvedi, K.U.; Raj, A. Neurilemmoma of tongue. Indian J. Otolaryngol. Head Neck Surg. 2003, 55, 193–194. [Google Scholar] [CrossRef] [PubMed]
- Cinar, F.; Cinar, S.; Harman, G. Schwannoma of the tip of the tongue in a child. Plast. Reconstr. Surg. 2004, 114, 1657–1658. [Google Scholar] [PubMed]
- Bassichis, B.A.; McClay, J.E. Pedunculated neurilemmoma of the tongue base. Otolaryngol. Head Neck Surg. 2004, 130, 639–641. [Google Scholar] [CrossRef] [PubMed]
- Tamaki, J.; Uchiyama, Y.; Ozono, K.; Gamoh, S.; Chien, C.C.C.; Kishino, M.; Kakimoto, N.; Murakami, S. A case of schwannoma in the tongue diagnosed with enhanced magnetic resonance image. Oral Radiol. 2004, 20, 83–86. [Google Scholar] [CrossRef]
- Chuang, H.-C.; Su, C.-Y.; Lui, C.-C.; Hwang, C.-F.; Chien, C.-Y. Lingual nerve neurilemmoma. J. Otolaryngol. 2004, 33, 132–134. [Google Scholar] [CrossRef]
- Vafiadis, M.; Fiska, A.; Panopoulou, M.; Assimakopoulos, D. A clinical case report of a Schwannoma on the tip of the tongue. B-ENT 2005, 1, 201–204. [Google Scholar] [PubMed]
- Hwang, K.; Kim, S.G.; Ahn, S.I.; Lee, S.I. Neurilemmoma of the tongue. J. Craniofac. Surg. 2005, 16, 859–861. [Google Scholar] [CrossRef] [PubMed]
- Nakasato, T.; Kamada, Y.; Ehara, S.; Miura, Y. Multilobular neurilemmoma of the tongue in a child. AJNR Am. J. Neuroradiol. 2005, 26, 421–423. [Google Scholar] [PubMed] [PubMed Central]
- López-Jornet, P.; Bermejo-Fenoll, A. Neurilemmoma of the tongue. Oral Oncol. Extra 2005, 41, 154–157. [Google Scholar] [CrossRef][Green Version]
- Bansal, R.; Trivedi, P.; Patel, S. Schwannoma of the tongue. Oral Oncol. Extra 2005, 41, 15–17. [Google Scholar] [CrossRef]
- Enoz, M.; Suoglu, Y.; Ilhan, R. Lingual schwannoma. J. Cancer Res. Ther. 2006, 2, 76–78. [Google Scholar] [CrossRef] [PubMed]
- Mehrzad, H.; Persaud, R.; Papadimitriou, N.; Kaniyur, S.; Mochloulis, G. Schwannoma of tongue base treated with transoral carbon dioxide laser. Lasers Med. Sci. 2006, 21, 235–237. [Google Scholar] [CrossRef] [PubMed]
- Batra, K.; Rai, A.K.; Chaudhary, N.; Topno, S. Two cases of neurilemmoma of the tongue. Ear Nose Throat J. 2007, 86, 679–681. [Google Scholar] [CrossRef] [PubMed]
- Farzadnia, M.; Bakhshaee, M.; Badiei, R. Schwannoma of the tongue base: A case report. Iran. J. Pathol. 2007, 2, 119–122. [Google Scholar]
- Ferreti Bonan, P.R.; Martelli, H., Jr.; Nogueira Dos Santos, L.A.; Comini Mol, V.; Paes De Almeida, O. Multinodular neurilemmoma of the tongue: A case report with differential immunohistochemical profile. Minerva Stomatol. 2008, 57, 71–75. [Google Scholar] [PubMed]
- Pereira, L.J.; Pereira, P.P.; dos Santos, J.D.P.; Reis Filho, V.F.; Dominguete, P.R.; Pereira, A.A. Lingual schwannoma involving the posterior lateral border of the tongue in a young individual: Case report. J. Clin. Pediatr. Dent. 2008, 33, 59–62. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.; Garg, A.; Dhingra, K.K.; Jain, D.; Kohli, K.; Khurana, N. Schwannoma tongue: A rare entity. ANZ J. Surg. 2009, 79, 93–94. [Google Scholar] [CrossRef] [PubMed]
- Cohen, M.; Wang, M.B. Schwannoma of the tongue: Two case reports and review of the literature. Eur. Arch. Otorhinolaryngol. 2009, 266, 1823–1829. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rahbar, M.; Mardanpour, K. Lingual Schwannoma: A case report. Iran. Red. Cresc. Med. J. 2009, 11, 454–456. [Google Scholar]
- Naidu, G.S.; Sinha, S.M. Schwannoma of the tongue: An unusual presentation in a child. Indian J. Dent. Res. 2010, 21, 457–459. [Google Scholar] [CrossRef] [PubMed]
- Karaca, C.T.; Habesoglu, T.E.; Naiboglu, B.; Habesoglu, M.; Oysu, C.; Egeli, E.; Tosun, I. Schwannoma of the tongue in a child. Am. J. Otolaryngol. 2010, 31, 46–48. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jeffcoat, B.T.; Pitman, K.T.; Brown, A.S.; Baliga, M. Schwannoma of the oral tongue. Laryngoscope 2010, 120 (Suppl. S4), S154. [Google Scholar] [CrossRef] [PubMed]
- Moreno-García, C.; Pons-García, M.A.; González-García, R.; Monje-Gil, F. Schwannoma of tongue. J. Maxillofac. Oral Surg. 2014, 13, 217–221. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Husain, S.; Yunus, M.R.; Ramli, R.; Athar, P.P. Schwannoma of the tongue in a ten-year old child. J. Pak. Med. Assoc. 2011, 61, 500–501. [Google Scholar] [PubMed]
- Ferrari, L.; Fonseca, J.J. Schwannoma of the tongue with a happy ending. Int. J. Surg. Pathol. 2011, 19, 497–498. [Google Scholar] [CrossRef] [PubMed]
- Catalfamo, L.; Lombardo, G.; Nava, C.; Familiari, E.; Petrocelli, M.; Iudicello, V.; Ieni, A.; Barresi, V.; De Ponte, F.S. Tongue schwannoma: Clinicopathological findings. J. Craniofac. Surg. 2011, 22, 1158–1161. [Google Scholar] [CrossRef] [PubMed]
- Verma, R.K.; Dhingra, S.; Gupta, K.; Panda, N.K. Lingual schwannoma—A case report. Oral Surg. 2011, 4, 82–85. [Google Scholar] [CrossRef]
- Hirbod, H.; Husain, S.; Ami, M.B. Lingual Schwannoma. Rawal. Med. J. 2011, 36, 60–61. [Google Scholar]
- Lukšić, I.; Müller, D.; Virag, M.; Manojlović, S.; Ostović, K.T. Schwannoma of the tongue in a child. J. Craniomaxillofac. Surg. 2011, 39, 441–444. [Google Scholar] [CrossRef] [PubMed]
- Manna, F.; Barbi, E.; Murru, F.; Bussani, R. Lingual schwannoma in pediatric patients. J. Craniofacial Surg. 2012, 23, e454–e456. [Google Scholar] [CrossRef] [PubMed]
- Mirza, A.; Iqbal, I.; Kishore, A.; Qzai, S.; Sheetal, K. Lingual Schwannoma: Our experience. Online J. Otolaryngol. 2012, 2, 59. [Google Scholar]
- Zaifullah, S.; Aboud, S.K.; Yunus, M.R.M.; Rose, I.M.; Nasseri, Z. Schwannoma of the tongue: A case report. Rawal Med. J. 2012, 37, 12–15. [Google Scholar]
- Ferreira, D.C.; Nogueira, G.; Cancio, V.A.; Cavalcante, F.S.; Godefroy, P.; Sousa, D.S.; Hespanhol, W.; dos Santos, K.R.; Cavalcante, M.A. Loss of lingual sensitivity and slightly increased size signaling schwannoma in a patient with mixed conjunctive tissue disease. Spec. Care Dent. 2013, 33, 301–303. [Google Scholar] [CrossRef] [PubMed]
- Lykke, E.; Noergaard, T.; Rasmussen, E.R. Lingual neurofibroma causing dysaesthesia of the tongue. BMJ Case Rep. 2013, 2013, bcr2013010440. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, S.J.; Kim, Y.; Leem, D.H.; Baek, J.A.; Shin, H.K.; Ko, S.O. Ancient schwannoma misdiagnosed as a hemangioma in the ventral tongue. Maxillofac. Plast. Reconstr. Surg. 2013, 35, 402–407. [Google Scholar] [CrossRef][Green Version]
- Özcan, C.; Görür, K.; Ünal, M.; Polatm, A. Benign schwannoma of the tongue with sudden enlargement. Ann. Med. Sci. 2001, 10, 133–134. [Google Scholar]
- Kamath, M.P.; Kini, H.; Shenoy, S.V.; Deviprasad, D.; Prakash, N.; Pai, R. Schwannoma of the base of tongue—A rare presentation. Egypt. J. Ear Nose Throat Allied Sci. 2014, 15, 61–64. [Google Scholar] [CrossRef]
- Rao, S.S.; Ahmed, J.M.; Ingale, A. Schwannoma of the tongue—A case report. J. Ev. Med. Sci. 2013, 2, 9150–9153. [Google Scholar]
- Monga, S.; Malik, J.N.; Sharma, A.P. Schwannoma Tongue. J. Case Rep. 2013, 3, 220–222. [Google Scholar] [CrossRef]
- Sanchis, J.M.; Navarro, C.M.; Bagán, J.V.; Onofre, M.A.; Murillo, J.; De-Andrade, C.R.; Díaz, J.M.; Pereira-Filho, V.A. Intraoral schwannomas: Presentation of a series of 12 cases. J. Clin. Exp. Dent. 2013, 5, e192. [Google Scholar] [CrossRef]
- Feltes-Ochoa, R.A.; Maseda-Pedrero, R.; Ruíz-Burguillos, E. Schwannoma of the Tongue. Actas Dermosifiliogr. 2015, 106, 512–514. [Google Scholar] [CrossRef] [PubMed]
- Nibhoria, S.; Tiwana, K.; Phutela, R.; Kaur, J. Schwannoma of tongue: A rare case presentation with review of literature. IJSS 2015, 3, 147–149. [Google Scholar]
- Ashish, G.; Sundereshan, R.S.; Philip, A. Transoral Laser Excision of Schwannoma in Base of Tongue: A Case Report with Review of Literature. Otorhinolaryngol. Clin. Int. J. 2015, 7, 68–71. [Google Scholar] [CrossRef]
- Sharma, S.; Rai, G. Schwannoma (Neurilemmoma) on the Base of the Tongue: A Rare Clinical Case. Am. J. Case Rep. 2016, 17, 203–206. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kavčič, J.; Božič, M. Schwannoma of the tongue. BMJ Case Rep. 2016, 2016, bcr2016215799. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, J.S.; Minh, P.N.; Hong, K.H. Huge Tongue Base Neurilemmoma: Excision by Intraoral Coblation. J. Clin. Otolaryngol. Head Neck Surg. 2016, 27, 384–387. [Google Scholar] [CrossRef]
- Qayoom, S.; Khan, S.; Bahadur, S.; Jetley, S. Lingual schwannoma: A cytological diagnosis. J. Cytol. 2016, 33, 111–112. [Google Scholar]
- Sharma, S.; Sharma, A.; Kumar, A.; Ahlawat, B.; Sharma, R. Schwannoma of Tongue in a Child. Ann Woman Child Health 2016, 2, 5–8. [Google Scholar]
- Gopalakrishnan, S.N.; Jayaraman, N.K.; Lourdes Albina, S.A. Schwannoma over tongue base–Case report and review. Online J. Otolaryngol. 2016, 6, 1–7. [Google Scholar]
- Purohit, J.P.; Selvaraj, S.; Purohit, K.; Kumar, V.; Moshahary, S. Atypical presentation of neurilemmoma of base of tongue—A case report. J. Evol. Med. Dent. Sci. 2017, 6, 255–257. [Google Scholar] [CrossRef]
- Indrasari, S.R.; Fedriani, J. Base of tongue schwannoma on a 22 year old lady: A rare case. Int. J. Otorhinolaryngol. Head Neck Surg. 2017, 4, 247. [Google Scholar] [CrossRef][Green Version]
- de Olivera, R.F.; de Lima, J.M.G.; Melo, V.; Pinheiro, T.N. Schwannoma of the Tongue. OMP 2017, 2, e68. [Google Scholar] [CrossRef]
- Lee, E.Y.; Kim, J.J.; Seok, H.; Lee, J.Y. Schwannoma of the tongue: A case report with review of literature. Maxillofac. Plast. Reconstr. Surg. 2017, 39, 17. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Abreu, I.; Roriz, D.; Rodrigues, P.; Moreira, Â.; Marques, C.; Alves, F.C. Schwannoma of the tongue—A common tumour in a rare location: A case report. Eur. J. Radiol. Open 2017, 4, 1–3. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nair, V.; Dey, B.; Deshpande, A.H.; Nigam, J.S. Cystic Schwannoma of Tongue Masquerading as Mucocele: A Cytological Pitfall. J. Cytol. 2018, 35, 125–126. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sanches, G.T.; Yanaguizawa, W.H.; Da Silva, E.F.P.; Sugaya, N.N.; Martins, M.T. Neurilemmoma of the Dorsaltongue: Atypical Clinical and Pathological Presentation. OMP 2018, 126, 114. [Google Scholar]
- Sharma, P.; Zaheer, S.; Goyal, S.; Ahluwalia, C.; Goyal, A.; Bhuyan, G.; Mandal, A.K. Clinicopathological analysis of extracranial head and neck schwannoma: A case series. J. Cancer Res. Ther. 2019, 15, 659–664. [Google Scholar] [CrossRef] [PubMed]
- Shimomura-Kurihara, M.; Yamamoto, K.; Shimomura, T.; Horita, S.; Yagyuu, T.; Shimomura, H.; Kirita, T. Giant Schwannoma of the tongue accompanied by difficulty in closing the mouth and dysarthria: A case report. J. Oral Maxillofac. Surg. Med. Pathol. 2019, 31, 264–268. [Google Scholar] [CrossRef]
- Kim, T.K.; Kim, H.Y.; Yu, I.K.; Son, H.J.; Chang, D.S.; Do Jang, Y. Schwannoma of the tongue base with imaging features and differential diagnosis: A rare case report and literature review. Investig. Magn. Reson. Imaging 2019, 23, 385–389. [Google Scholar] [CrossRef]
- Murgod, P.S.; Doshi, P.R.; Doshi, R.S. Schwannoma of tongue with review of literature. Indian J. Pathol. Oncol. 2019, 6, 413–416. [Google Scholar]
- Soliman, Z.R.; Mobashir, M.K.; Askar, S.M. Trans–oral, Carbon Dioxide–Assisted Excision of an Unusual Schwannoma of the Tongue Base: Case Report and Review of the Literature. Int. Arch. Otorhinolaryngol. 2019, 23, e354–e359. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barca, I.; Novembre, D.; Elvis, K.; Zuccalà, V.; Cristofaro, M.G. A rare case of ancient schwannoma of the tongue. Ann. Ital. Chir. 2020, 9, S2239253X20033897. [Google Scholar] [PubMed]
- Keshwar, S.; Shrestha, A.; Jaisani, M.R.; Acharya, P. An Uncommon Pathology “Schwannoma of the Tongue” in Young Adult–A Case Report. J. Adv. Med. Dent. Sci. Res. 2020, 8, 45–47. [Google Scholar]
- Alrohaimi, F.A.; Alsadah, S.A.; Althaqib, G.A. Lingual schwannoma in an adolescent boy: A case report. Ann. Med. Surg. 2021, 65, 102216. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Haider, M.Y.; Rahim, M.; Bashar, N.M.K.; Hossain, M.Z.; Islam, S.M.J. Schwannoma of the Base of the Tongue: A Case Report of a Rare Disease and Review of Literatures. Case Rep. Surg. 2020, 2020, 7942062. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sousa, A.A.; Porto, J.G. Schwannoma of the oral tongue. Arch. Head Neck Surg. 2020, 49, e00212020. [Google Scholar] [CrossRef]
- Shibata, M.; Yagihara, K.; Yagishita, H.; Ishii, J.; Kim, Y.; Ishikawa, A. Schwannoma of the tongue: A case report with and review of the literature. Oral Sci. Int. 2021, 18, 78–87. [Google Scholar] [CrossRef]
- Gayen, S.; Kundu, S.; Das, S.K.; Mahmud, S.A.; Pal, M. Schwannoma of tongue—A case report. Oral Maxillofac. Pathol. J. 2020, 11, 42–44. [Google Scholar]
- Ohta, K.; Yoshimura, H. Schwannoma of the tongue. CMAJ 2021, 193, E98. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Agha-Hosseini, F.; Moosavi, M.S.; Aminishakib, P.; Yousefian, M. A fast-growing schwannoma of the tongue in a 15-year-old Iranian male: Review of literature and case report. Clin. Case Rep. 2021, 9, e04266. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Natarajan, K.; Sethuraman, S.N.; Sampathkumar, R.; Susruthan, A.R.; Kameswaran, M. KTP 532 laser excision of lingual schwannoma: A case report. Int. J. Otorhinolaryngol. Head Neck Surg. 2021, 7, 683. [Google Scholar] [CrossRef]
- Yun, C.B.; Kim, Y.M.; Choi, J.S.; Kim, J.W. Pediatric schwannoma of the tongue: A case report and review of literature. World J. Clin. Cases 2021, 9, 7212–7217. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Singh, A.; Kuzhikkali, V.; Kairo, A.K. Recurrent schwannoma of the tongue in a pediatric patient—Report of a rare case with an updated review of literature. Egypt. J. Otolaryngol. 2021, 37, 1–5. [Google Scholar] [CrossRef]
- Jagtap, S.V.; Jagtap, S.S.; Mishra, S.; Brahmbhatt, D.; Kaur, P. Schwannoma of the Tongue. Int. J. Health Sci. Res. 2021, 11, 151–154. [Google Scholar] [CrossRef]
- Husain, P.; Taparwal, A.; Ahmed, S.K.; Husain, B. Unusual Presentation of a Giant Schwannoma of Left Lateral Border of Tongue: A Rare Case Report. Indian J. Otolaryngol. Head Neck Surg. 2022, 74 (Suppl. S3), 5810–5813. [Google Scholar] [CrossRef]
- Hammood, Z.D.; Baba, H.O.; Saeed, Y.A.; Salih, A.M.; Noori, S.S.; Abdullah, H.O.; Tahir, S.H.; Kakamad, F.H. Cellular schwannoma of the posterior tongue: A rare case report with a literature review. IJS Short Rep. 2022, 7, e54. [Google Scholar] [CrossRef]
- Ali, S.; Vassiliou, L.; Stenhouse, P. Plexiform Schwannoma: A Report of Two Unusual Cases, and a Review of the Literature. Open J. Stomatol. 2014, 4, 174–178. [Google Scholar] [CrossRef][Green Version]
- Asadi, M.; Mohseni, M.; Jahanshahi, F.; Esmaeili, A.; Mohsenifar, Z. Schwannoma (neurilemmoma) of tongue: A rare case presentation and review of literature. Clin. Case Rep. 2023, 11, e7235. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Doshi, A.; Bhola, N. Neurilemmoma of Tongue in a Young Female: A Case Report. Cureus 2023, 15, e47438. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pierri, M.; Moffa, A.; Sabatino, L.; Iafrati, F.; Di Giovanni, S.; De Benedetto, L.; Casale, M. Case Report and Literature Review on Tongue Schwannoma. J. Otorhinolaryngol. Hear. Balance Med. 2024, 5, 11. https://doi.org/10.3390/ohbm5020011
Pierri M, Moffa A, Sabatino L, Iafrati F, Di Giovanni S, De Benedetto L, Casale M. Case Report and Literature Review on Tongue Schwannoma. Journal of Otorhinolaryngology, Hearing and Balance Medicine. 2024; 5(2):11. https://doi.org/10.3390/ohbm5020011
Chicago/Turabian StylePierri, Michelangelo, Antonio Moffa, Lorenzo Sabatino, Francesco Iafrati, Simone Di Giovanni, Luigi De Benedetto, and Manuele Casale. 2024. "Case Report and Literature Review on Tongue Schwannoma" Journal of Otorhinolaryngology, Hearing and Balance Medicine 5, no. 2: 11. https://doi.org/10.3390/ohbm5020011
APA StylePierri, M., Moffa, A., Sabatino, L., Iafrati, F., Di Giovanni, S., De Benedetto, L., & Casale, M. (2024). Case Report and Literature Review on Tongue Schwannoma. Journal of Otorhinolaryngology, Hearing and Balance Medicine, 5(2), 11. https://doi.org/10.3390/ohbm5020011







