Pharyngocutaneous Fistula after Laryngectomy: An Umbrella Systematic Review to Uncover Lacunae in Meta-Analyses
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Search Syntax
2.3. Data Screening and Selection
2.4. Inclusion Criteria
- Total laryngectomy/laryngopharyngectomy for laryngeal and hypopharyngeal cancer;
- Laryngeal or hypopharyngeal cancers with total laryngectomy/laryngopharyngectomy (with or without neck dissection) as primary or salvage therapy;
- A meta-analysis published in peer-reviewed journals;
- Meta-analysis must report on pharyngocutaneous fistula following total laryngectomy/laryngopharyngectomy.
2.5. Exclusion Criteria
- Non-human studies;
- Laryngectomy/laryngopharyngectomy for non-oncological reason;
- Not reported—regarding operative outcomes;
- Review articles, meeting abstracts, case reports, editorial letters, as well as other forms of publication;
- Incomplete data or insufficient information.
2.6. Data Extraction
2.7. Statistical Analysis
3. Results
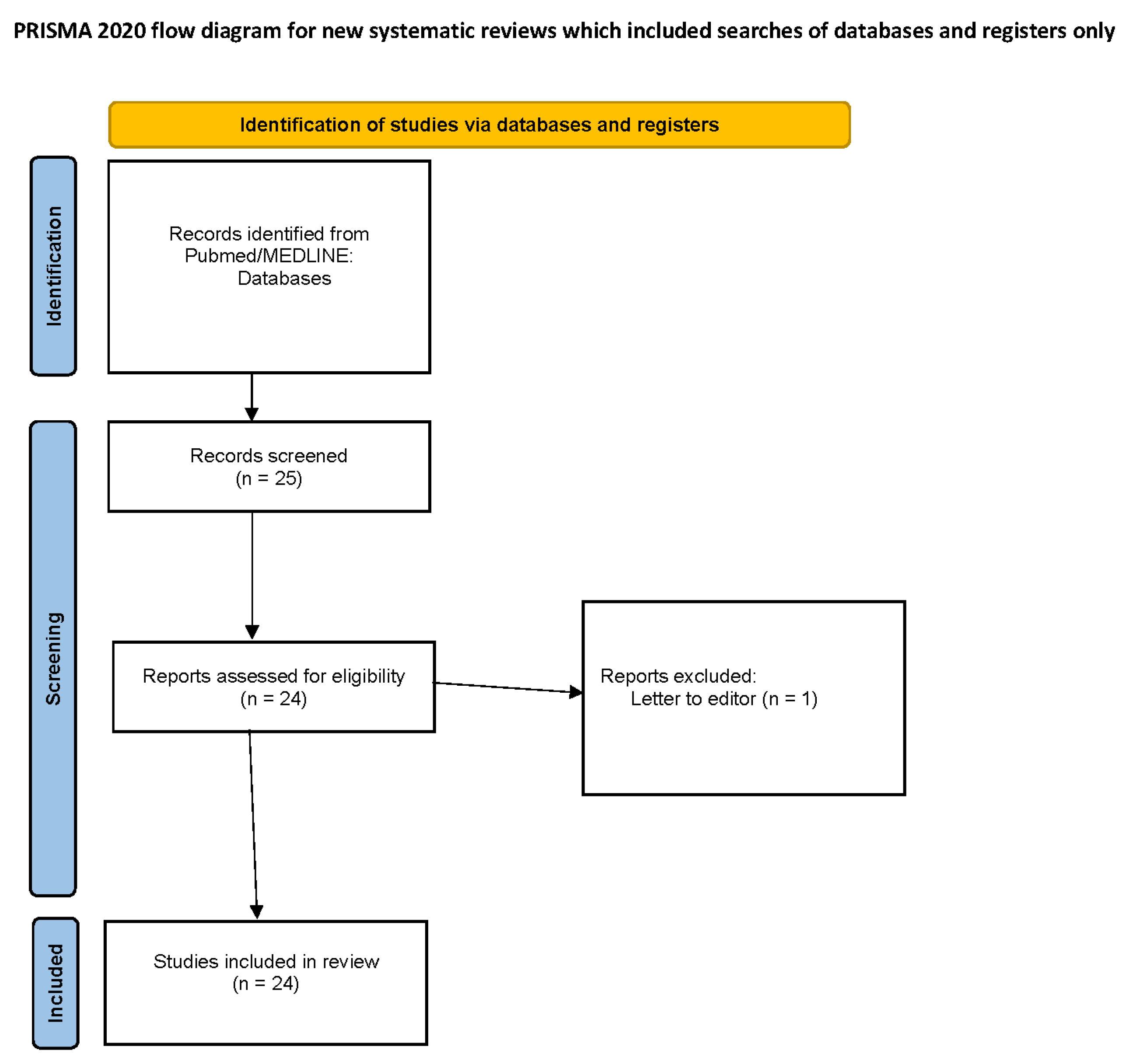
3.1. Literature Retrieval and Data Extraction
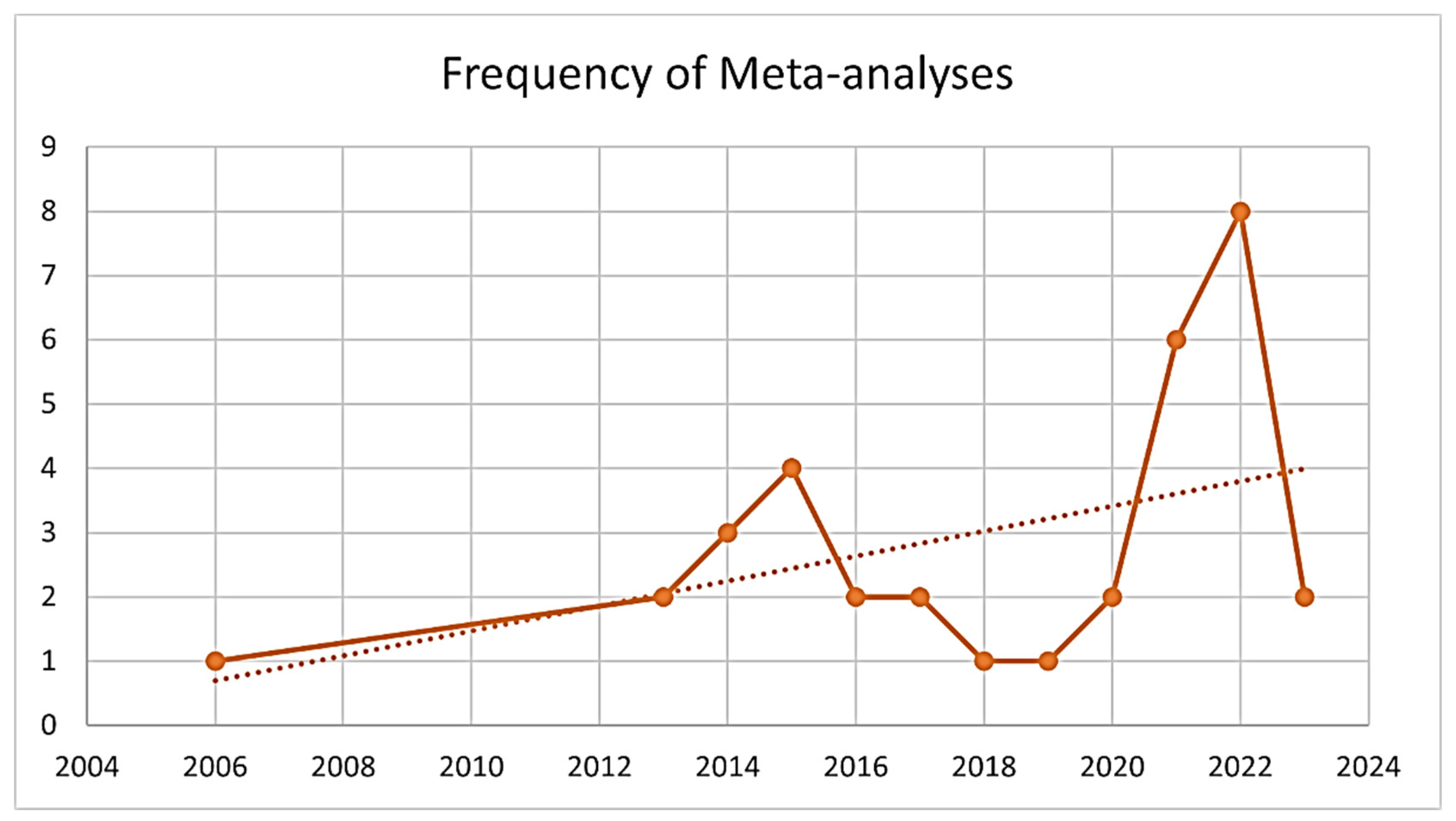
3.2. Year of Publication
3.3. Country of Origin
3.4. Type of Laryngectomy
3.5. Journal
3.6. Research Question
3.7. Outcomes
- Risk factors for PCF was found to be age [3,14], smoking [14], low hemoglobin [3,7,14,19,20,24], low albumin [7,14], comorbidities [3,7,14,19], diabetes [3,7], chronic obstructive pulmonary disease [14,19], coronary artery disease [14], tumor site [3,14,19,20], hypopharyngeal involvement [7,19], previous radiation therapy [3,14,19,20,24], margins [7,19,20], type of pharyngeal closure [7,14], TEP [3], neck dissection [19,24], and blood transfusion [19];
- Salivary bypass tube usage following TL led to lower rates of PCF [4];
- The horizontal method of pharyngeal closure following TL led to lower rates of PCF [6].
- Organ preservation protocols led to higher rates of PCF [16];
- Primary and secondary TEP—no difference was found in the rates of PCF between primary and secondary TEP insertion [15];
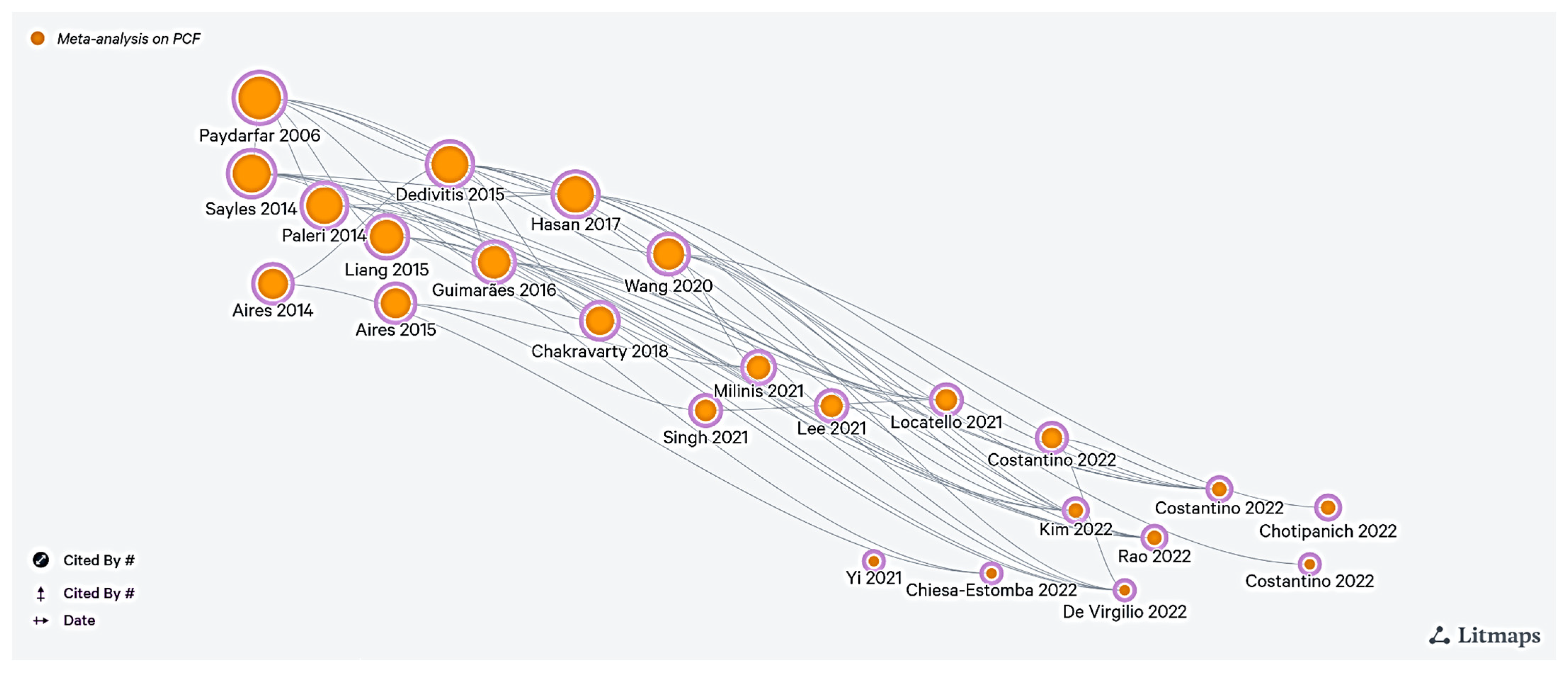
3.8. Citation Network
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Costantino, A.; Festa, B.M.; Kim, S.H.; Baik, F.M.; Wang, C.C.; Pirola, F.; Malvezzi, L.; Spriano, G.; Mercante, G.; De Virgilio, A. Complications of pectoralis major myo-cutaneous flap, anterolateral thigh flap and radial forearm free flap after total laryngectomy with partial pharyngectomy: A systematic review and network meta-analysis. Microsurgery 2023, 43, 286–296. [Google Scholar] [CrossRef] [PubMed]
- Costantino, A.; Festa, B.M.; Ferreli, F.; Russo, E.; Malvezzi, L.; Giannitto, C.; Spriano, G.; Mercante, G.; De Virgilio, A. Circumferential pharyngeal reconstruction after total laryngopharyngectomy: A systematic review and network meta-analysis. Oral Oncol. 2022, 127, 105809. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Kim, S.W.; Hwang, S.H. Predictive Value of Risk Factors for Pharyngocutaneous Fistula After Total Laryngectomy. Laryngoscope 2023, 133, 742–754. [Google Scholar] [CrossRef] [PubMed]
- Costantino, A.; Pace, G.M.; Festa, B.M.; Ferreli, F.; Malvezzi, L.; Spriano, G.; Mercante, G.; De Virgilio, A. Salivary bypass tube in total laryngectomy: Systematic review and meta-analysis. Head Neck 2022, 44, 2608–2620. [Google Scholar] [CrossRef]
- Chiesa-Estomba, C.M.; Mayo-Yanez, M.; Palacios-García, J.M.; Lechien, J.R.; Viljoen, G.; Karkos, P.D.; Barillari, M.R.; González-García, J.A.; Sistiaga-Suarez, J.A.; González-Botas, J.H.; et al. Stapler-Assisted Pharyngeal Closure After Total Laryngectomy: A Systematic Review and Meta-Analysis. Oncol. Ther. 2022, 10, 241–252. [Google Scholar] [CrossRef]
- Chotipanich, A.; Wongmanee, S. Incidence of Pharyngocutaneous Fistula After Total Laryngectomy and Its Relationship With the Shapes of Mucosa Closure: A Meta-Analysis. Cureus 2022, 14, e28822. [Google Scholar] [CrossRef]
- Rao, K.N.; Arora, R.D.; Singh, A.; Nagarkar, N.M.; Aggarwal, A. Pharyngocutaneous Fistula Following Primary Total Laryngectomy: A Meta-analysis. Indian J. Surg. Oncol. 2022, 13, 797–808. [Google Scholar] [CrossRef]
- De Virgilio, A.; Costantino, A.; Festa, B.M.; Russo, E.; Malvezzi, L.; Pellini, R.; Colombo, G.; Spriano, G.; Mercante, G.; Ferreli, F. Surgical prevention of pharyngocutaneous fistula in salvage total laryngectomy: A systematic review and network meta-analysis. Eur. Arch. Oto-Rhino-Laryngol. 2022, 279, 5839–5849. [Google Scholar] [CrossRef]
- Singh, R.; Karantanis, W.; Fadhil, M.; Dow, C.; Fuzi, J.; Robinson, R.; Jacobson, I. Meta-analysis on the rate of pharyngocutaneous fistula in early oral feeding in laryngectomy patients. Am. J. Otolaryngol. 2021, 42, 102748. [Google Scholar] [CrossRef]
- Yi, X.; Hu, C.; Peng, Y.; Wen, Z.; Li, X.; Ye, L.; Huang, Q. Meta-analysis on the safety and efficacy of early oral feeding after total laryngectomy. J. BUON Off. J. Balk. Union. Oncol. 2021, 26, 2019–2025. [Google Scholar]
- Locatello, L.G.; Licci, G.; Maggiore, G.; Gallo, O. Non-Surgical Strategies for Assisting Closure of Pharyngocutaneous Fistula after Total Laryngectomy: A Systematic Review of the Literature. J. Clin. Med. 2021, 11, 100. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.C.; Fang, T.J.; Kuo, I.C.; Tsai, Y.T.; Hsin, L.J. Stapler closure versus manual closure in total laryngectomy for laryngeal cancer: A systematic review and meta-analysis. Clin. Otolaryngol. 2021, 46, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Milinis, K.; Gaskell, P.; Lau, A.; Lancaster, J.; Jones, T. Early versus late oral feeding following total (pharyngo)laryngectomy: Systematic review and meta-analysis. Head Neck 2021, 43, 1359–1368. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Xun, Y.; Wang, K.; Lu, L.; Yu, A.; Guan, B.; Yu, C. Risk factors of pharyngocutaneous fistula after total laryngectomy: A systematic review and meta-analysis. Eur. Arch. Oto-Rhino-Laryngol. 2020, 277, 585–599. [Google Scholar] [CrossRef] [PubMed]
- Chakravarty, P.D.; McMurran, A.E.L.; Banigo, A.; Shakeel, M.; Ah-See, K.W. Primary versus secondary tracheoesophageal puncture: Systematic review and meta-analysis. J. Laryngol. Otol. 2018, 132, 14–21. [Google Scholar] [CrossRef]
- Hasan, Z.; Dwivedi, R.C.; Gunaratne, D.A.; Virk, S.A.; Palme, C.E.; Riffat, F. Systematic review and meta-analysis of the complications of salvage total laryngectomy. Eur. J. Surg. Oncol. J. Eur. Soc. Surg. Oncol. Br. Assoc. Surg. Oncol. 2017, 43, 42–51. [Google Scholar] [CrossRef]
- Guimarães, A.V.; Aires, F.T.; Dedivitis, R.A.; Kulcsar, M.A.V.; Ramos, D.M.; Cernea, C.R.; Brandão, L.G. Efficacy of pectoralis major muscle flap for pharyngocutaneous fistula prevention in salvage total laryngectomy: A systematic review. Head Neck 2016, 38 (Suppl. S1), E2317–E2321. [Google Scholar] [CrossRef]
- Aires, F.T.; Dedivitis, R.A.; Petrarolha, S.M.P.; Bernardo, W.M.; Cernea, C.R.; Brandão, L.G. Early oral feeding after total laryngectomy: A systematic review. Head Neck 2015, 37, 1532–1535. [Google Scholar] [CrossRef]
- Dedivitis, R.A.; Aires, F.T.; Cernea, C.R.; Brandão, L.G. Pharyngocutaneous fistula after total laryngectomy: Systematic review of risk factors. Head Neck 2015, 37, 1691–1697. [Google Scholar] [CrossRef]
- Liang, J.W.; Li, Z.D.; Li, S.C.; Fang, F.Q.; Zhao, Y.J.; Li, Y.G. Pharyngocutaneous fistula after total laryngectomy: A systematic review and meta-analysis of risk factors. Auris Nasus Larynx 2015, 42, 353–359. [Google Scholar] [CrossRef]
- Aires, F.T.; Dedivitis, R.A.; Castro, M.A.F.; Bernardo, W.M.; Cernea, C.R.; Brandão, L.G. Efficacy of stapler pharyngeal closure after total laryngectomy: A systematic review. Head Neck 2014, 36, 739–742. [Google Scholar] [CrossRef] [PubMed]
- Sayles, M.; Grant, D.G. Preventing pharyngo-cutaneous fistula in total laryngectomy: A systematic review and meta-analysis. Laryngoscope 2014, 124, 1150–1163. [Google Scholar] [CrossRef] [PubMed]
- Paleri, V.; Drinnan, M.; van den Brekel, M.W.M.; Hinni, M.L.; Bradley, P.J.; Wolf, G.T.; De Bree, R.; Fagan, J.J.; Hamoir, M.; Strojan, P.; et al. Vascularized tissue to reduce fistula following salvage total laryngectomy: A systematic review. Laryngoscope 2014, 124, 1848–1853. [Google Scholar] [CrossRef]
- Paydarfar, J.A.; Birkmeyer, N.J. Complications in head and neck surgery: A meta-analysis of postlaryngectomy pharyngocutaneous fistula. Arch. Otolaryngol. Head Neck Surg. 2006, 132, 67–72. [Google Scholar] [CrossRef]
- Litmaps [Internet]. Litmaps. Available online: https://app.litmaps.com (accessed on 7 May 2023).
- Ljumanovic, R.; Langendijk, J.A.; Hoekstra, O.S.; Knol, D.L.; Leemans, C.R.; Castelijns, J.A. Pre- and post-radiotherapy MRI results as a predictive model for response in laryngeal carcinoma. Eur. Radiol. 2008, 18, 2231–2240. [Google Scholar] [CrossRef][Green Version]
- Nauta, T.D.; van Hinsbergh, V.W.M.; Koolwijk, P. Hypoxic Signaling During Tissue Repair and Regenerative Medicine. Int. J. Mol. Sci. 2014, 15, 19791–19815. [Google Scholar] [CrossRef] [PubMed]
- Sheaff, M.; Baithun, S. Pathological effects of ionizing radiation. Curr. Diagn. Pathol. 1997, 4, 106–115. [Google Scholar] [CrossRef]
- Hefermehl, L.J.; Largo, R.A.; Hermanns, T.; Poyet, C.; Sulser, T.; Eberli, D. Lateral temperature spread of monopolar, bipolar and ultrasonic instruments for robot-assisted laparoscopic surgery. BJU Int. 2014, 114, 245–252. [Google Scholar] [CrossRef]
- Haksever, M.; Akduman, D.; Aslan, S.; Solmaz, F.; Ozmen, S. Modified Continuous Mucosal Connell Suture for the Pharyngeal Closure After Total Laryngectomy: Zipper Suture. Clin. Exp. Otorhinolaryngol. 2015, 8, 281–288. [Google Scholar] [CrossRef]
- Feng, F.; Sun, L.; Xu, G.; Hong, L.; Yang, J.; Cai, L.; Li, G.; Guo, M.; Lian, X.; Zhang, H. Albert-Lembert versus hybrid-layered suture in hand sewn end-to-end cervical esophagogastric anastomosis after esophageal squamous cell carcinoma resection. J. Thorac. Dis. 2015, 7, 1917–1926. [Google Scholar]
- Lafreniere, R.; Ketcham, A.S. A single layer open anastomosis for all intestinal structures. Am. J. Surg. 1985, 149, 797–798. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine (US) Council on Health Care Technology; Sox, H.; Stern, S.; Owens, D.; Abrams, H.L. Problems of Multi-Institutional Studies. In Assessment of Diagnostic Technology in Health Care: Rationale, Methods, Problems, and Directions: Monograph of the Council on Health Care Technology [Internet]; National Academies Press (US): Washington, DC, USA, 1989. Available online: https://www.ncbi.nlm.nih.gov/books/NBK235189/ (accessed on 1 May 2023).
- Paradis, C. Bias in surgical research. Ann. Surg. 2008, 248, 180–188. [Google Scholar] [CrossRef] [PubMed]
| Author | Country | Journal | Publication Year | Type of Laryngectomy | Research Question | Result |
|---|---|---|---|---|---|---|
| Costantino A [1] | Italy | Microsurgery | 2023 | Both | Type of reconstruction on PCF rates | FRAFF—low PCF |
| Kim DH [3] | South Korea | Laryngoscope | 2023 | Both | To determine the risk factors for PCF | Risk factors—age, low Hb, diabetes, tumour site, previous RT, previous tracheostomy, primary vs. salvage TL, TEP, and low albumin |
| Costantino A [4] | Italy | Head Neck | 2022 | Both | Use of salivary bypass tube | Lower rates of PCF with salivary bypass tube |
| Costantino A [2] | Italy | Oral Oncol | 2022 | Both | Type of reconstruction following TP + TL | Free jejunal flap has lowest risk for PCF |
| Chiesa-Estomba CM [5] | Spain | Oncol Ther | 2022 | Both | Use of stapler for pharyngeal closure | Lower rates of PCF with stapler usage |
| Chotipanich A [6] | Thailand | Cureus | 2022 | Both | Type of pharyngeal closure | Horizontal closure—lower rates of PCF |
| Rao KN [7] | India | Indian J Surg Oncol | 2022 | PTL | To determine the risk factors for PCF | Comorbidities, hypopharyngeagal site, low Hb, low Alb, stapler use, and positive margins |
| De Virgilio A [8] | Italy | Eur Arch Otorhinolaryngol | 2022 | STL | Onlay vascular flap versus patch pharyngoplasty | Onlay vascular flap has lower PCF rates |
| Singh R [9] | Australia | Am J Otolaryngol | 2021 | Both | Time of oral feed Initiation | Early feeding led to higher PCF |
| Yi X [10] | China | J BUON | 2021 | Both | Time of oral feed Initiation | No significant difference between early and late feeds |
| Locatello LG [11] | Italy | J Clin Med | 2021 | Both | Non-surgical treatment of PCF | Promising outcomes but small sample size |
| Lee YC [12] | Taiwan | Clin Otolaryngol | 2021 | Both | Use of stapler for pharyngeal closure | Lower rates of PCF with stapler usage |
| Milinis K [13] | UK | Head Neck | 2021 | Both | Time of oral feed Initiation | No significant difference between early and late feeds |
| Wang M [14] | China | Eur Arch Otorhinolaryngol | 2020 | Both | To determine the risk factors for PCF | Risk factors—age, smoking, COPD, CAD, RT, low Hb, low albumin, site, treatment method |
| Chakravarty PD [15] | UK | J Laryngol Otol | 2018 | Both | PCF rates in primary and secondary TEP | Similar rates |
| Hasan Z [16] | Australia | Eur J Surg Oncol | 2017 | STL | Role of organ preservation protocols in PCF | Increased rates of PCF with salvage TL |
| Guimarães AV [17] | Brasil | Head Neck | 2016 | STL | Role of onlay vascular flap in PCF | Lower incidence of PCF with onlay vascular flap |
| Aires FT [18] | Brasil | Head Neck | 2015 | Both | Time of oral feed Initiation | No significant difference between early and late feeds |
| Dedivitis RA [19] | Brasil | Head Neck | 2015 | Both | To determine the risk factors for PCF | Risk factors—COPD, low Hb, blood transfusion, CTRT, T stage, subsite, hypopharyngeal site, margins, and neck dissection |
| Liang JW [20] | China | Auris Nasus Larynx | 2015 | Both | To determine the risk factors for PCF | Risk factors—tumour subsite, T stage, previous RT, low Hb, and margins |
| Aires FT [21] | Brasil | Head Neck | 2014 | Both | Use of stapler for pharyngeal closure | Lower rates of PCF with stapler usage |
| Sayles M [22] | UK | Laryngoscope | 2014 | Both | Role of onlay vascular flap in PCF | Lower incidence of PCF with onlay vascular flap |
| Paleri V [23] | UK | Laryngoscope | 2014 | STL | Role of onlay vascular flap in PCF | Lower incidence of PCF with onlay vascular flap |
| Paydarfar JA [24] | USA | Arch Otolaryngol Head Neck Surg | 2006 | Both | To determine the risk factors for PCF | Risk factors—low Hb, previous RT, neck dissection |
| Sl No | Lacunae | Methods to Resolve Lacunae |
|---|---|---|
| 1. | Lack of Focus on Primary vs. Salvage Total Laryngectomy | Conduct separate meta-analyses for primary and salvage laryngectomy to determine distinct risk factors. |
| 2. | Lack of Comparative Studies | Initiate high-quality comparative studies for factors like pharyngeal mucosal closure techniques, extent of laryngectomy, and antibiotic types. |
| 3. | Paucity of Literature on Specific Factors | Encourage researchers to publish case series and studies on specific risk factors. |
| 4. | Need for Multi-Institutional and Multinational Collaborations | Establish collaborative networks for data collection and analysis, enhancing sample size and statistical power. |
| 5. | Heterogeneity and Lack of Randomized Trials | Encourage researchers to conduct randomized controlled trials. Promote pre-registration of meta-analyses to avoid duplication. |
| 6. | Bias in Surgical Research | Implement rigorous peer review processes and ensure transparency in reporting surgical techniques. |
| 7. | Congruence in Results | Encourage replication studies and meta-analyses to validate findings and strengthen hypotheses. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rao, K.N.; Arora, R.; Singh, A.; Dange, P.; Nagarkar, N.M. Pharyngocutaneous Fistula after Laryngectomy: An Umbrella Systematic Review to Uncover Lacunae in Meta-Analyses. J. Otorhinolaryngol. Hear. Balance Med. 2023, 4, 11. https://doi.org/10.3390/ohbm4020011
Rao KN, Arora R, Singh A, Dange P, Nagarkar NM. Pharyngocutaneous Fistula after Laryngectomy: An Umbrella Systematic Review to Uncover Lacunae in Meta-Analyses. Journal of Otorhinolaryngology, Hearing and Balance Medicine. 2023; 4(2):11. https://doi.org/10.3390/ohbm4020011
Chicago/Turabian StyleRao, Karthik Nagaraja, Ripudaman Arora, Ambesh Singh, Prajwal Dange, and Nitin M. Nagarkar. 2023. "Pharyngocutaneous Fistula after Laryngectomy: An Umbrella Systematic Review to Uncover Lacunae in Meta-Analyses" Journal of Otorhinolaryngology, Hearing and Balance Medicine 4, no. 2: 11. https://doi.org/10.3390/ohbm4020011
APA StyleRao, K. N., Arora, R., Singh, A., Dange, P., & Nagarkar, N. M. (2023). Pharyngocutaneous Fistula after Laryngectomy: An Umbrella Systematic Review to Uncover Lacunae in Meta-Analyses. Journal of Otorhinolaryngology, Hearing and Balance Medicine, 4(2), 11. https://doi.org/10.3390/ohbm4020011