Context-Specific Challenges, Opportunities, and Ethics of Drones for Healthcare Delivery in the Eyes of Program Managers and Field Staff: A Multi-Site Qualitative Study
Abstract
1. Introduction
2. Methods
2.1. Recruitment and Sampling
2.2. Data Collection
2.3. Data Analysis
2.4. Ethics
3. Results
3.1. Overview of Participants and Project Details
3.2. Benefits of Drones for Health Projects
3.2.1. Direct Benefits
3.2.2. Indirect Benefits
3.3. Concerns Surrounding the Implementation of Drones for Health Projects
3.3.1. Privacy and Security Concerns
3.3.2. Safety Concerns
3.3.3. The Importance of Context
3.4. Practical Challenges of Implementing Drones for Health Projects
3.4.1. Skepticism of Drone Technology
3.4.2. Lack of Resources
3.4.3. Technical Challenges
3.4.4. Lack of Guidelines and Regulations
3.4.5. Inability to Access Appropriate Stakeholders
3.5. Ethical Complexities in Implementing Drones for Health Projects
3.5.1. Complexities of Informed Consent
3.5.2. Individuals’ Perceived Limited Understanding of Drones for Health Projects
3.5.3. Aligning with Community Priorities
3.5.4. Transparency and Honesty in Project Management
4. Discussion
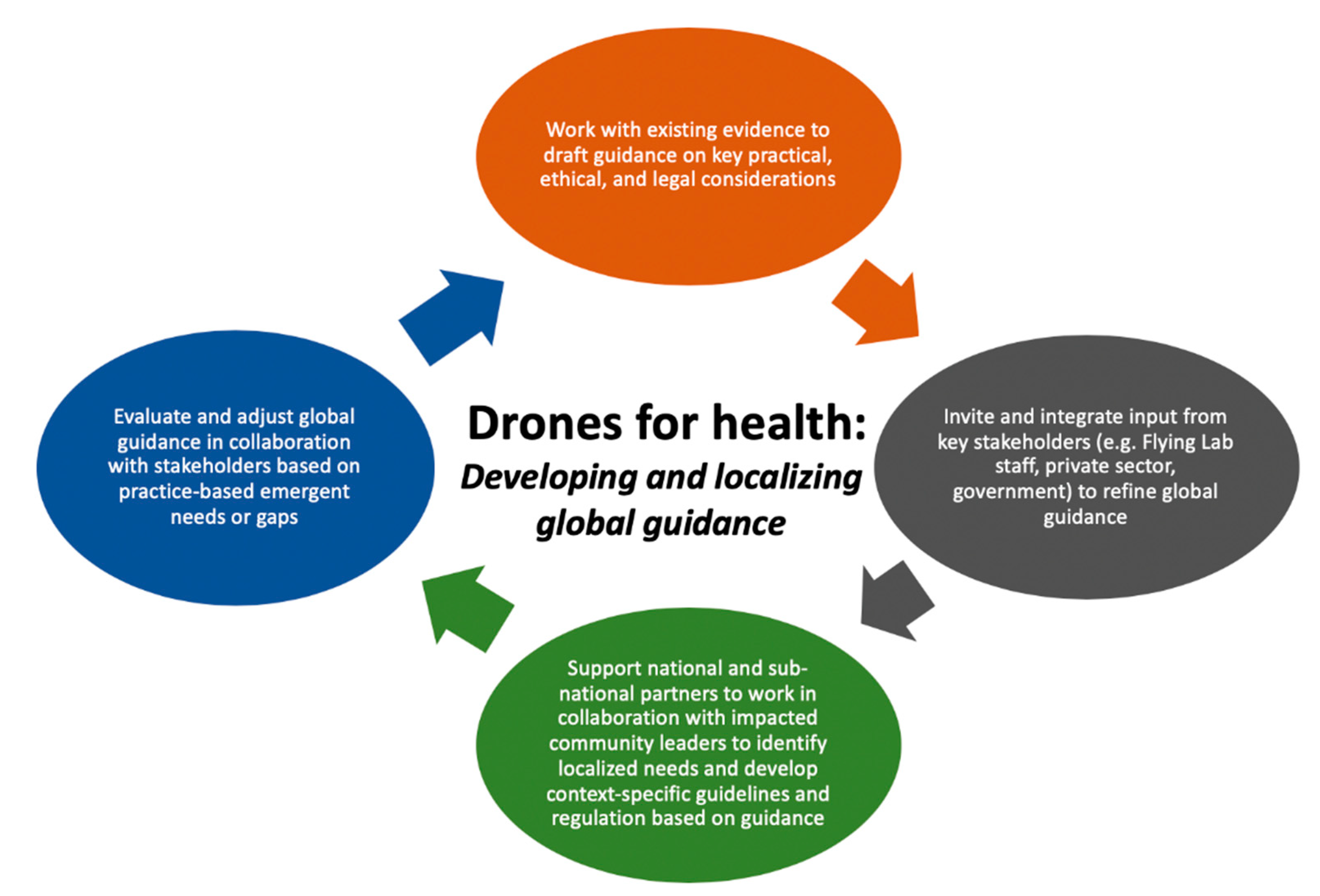
5. Conclusions
6. Study limitations
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Harnett, B.M.; Doarn, C.R.; Rosen, J.; Hannaford, B.; Broderick, T.J. Evaluation of unmanned airborne vehicles and mobile robotic telesurgery in an extreme environment. Telemed. E-Health 2008, 14, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Claesson, A.; Fredman, D.; Svensson, L.; Ringh, M.; Hollenberg, J.; Nordberg, P.; Rosenqvist, M.; Djarv, T.; Österberg, S.; Lennartsson, J.; et al. Unmanned aerial vehicles (drones) in out-of-hospital-cardiac-arrest. Scand. J. Trauma Resusc. Emerg. Med. 2016, 24, 124. [Google Scholar] [CrossRef] [PubMed]
- Claesson, A.; Bäckman, A.; Ringh, M.; Svensson, L.; Nordberg, P.; Djärv, T.; Hollenberg, J. Time to delivery of an automated external defibrillator using a drone for simulated out-of-hospital cardiac arrests vs. emergency medical services. JAMA 2017, 317, 2332–2334. [Google Scholar] [CrossRef]
- Drone Delivery Canada. Drone Delivery Canada Signs $2.5 Million Commercial Agreement with Moose Cree First Nation To Deploy DDC’s Drone Delivery Platform. Available online: https://dronedeliverycanada.com/resources/drone-delivery-canada-signs-2-5-million-commercial-agreement-with-moose-cree-first-nation-to-deploy-ddcs-drone-delivery-platform/ (accessed on 30 July 2020).
- Fornace, K.M.; Drakeley, C.J.; William, T.; Espino, F.; Cox, J. Mapping infectious disease landscapes: Unmanned aerial vehicles and epidemiology. Trends Parasitol. 2014, 30, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Gardner, T. Drone-Delivered Health Care in Rural Appalachia. Available online: https://www.clinicaladvisor.com/home/topics/practice-management-information-center/drone-delivered-health-care-in-rural-appalachia/ (accessed on 30 July 2020).
- Polanco González, C.; Islas Vazquez, I.; Castañón González, J.; Buhse, T.; Arias-Estrada, M. Electronic devices that identify individuals with fever in crowded places: A prototype. Micromachines 2017, 8, 202. [Google Scholar] [CrossRef]
- Healthcare IT News Australia. Puerto Rico Piloting Drones to Deliver Emergency Medical Supplies. Available online: https://www.healthcareitnews.com/news/puerto-rico-piloting-drones-deliver-emergency-medical-supplies (accessed on 30 July 2020).
- Katariya, M.; Chung, D.C.K.; Minife, T.; Gupta, H.; Zahidi, A.A.A.; Liew, O.W.; Ng, T.W. Drone inflight mixing of biochemical samples. Anal. Biochem. 2018, 545, 1–3. [Google Scholar] [CrossRef]
- Latimer, A.J.; McCoy, A.M.; Sayre, M.R. Emerging and future technologies in out-of-hospital cardiac arrest care. Cardiol. Clin. 2018, 36, 429–441. [Google Scholar] [CrossRef]
- Médecins Sans Frontières. Papua New Guinea: Innovating to Reach Remote TB Patients and Improve Access to Treatment. Available online: https://www.msf.org/papua-new-guinea-innovating-reach-remote-tb-patients-and-improve-access-treatment (accessed on 30 July 2020).
- Merchant, R.M.; Groeneveld, P.W. Neighborhood-level disparities in resuscitation and the potential of connected health. JAMA Cardiol. 2017, 2, 1118–1119. [Google Scholar] [CrossRef]
- Nouvet, E.; Knoblauch, A.M.; Passe, I.; Andriamiadanarivo, A.; Ravelona, M.; Ainanomena Ramtariharisoa, F.; Razafimdriana, K.; Wright, P.C.; McKinney, J.; Small, P.M.; et al. Perceptions of drones, digital adherence monitoring technologies and educational videos for tuberculosis control in remote Madagascar: A mixed-method study protocol. BMJ Open 2019, 9, e028073. [Google Scholar] [CrossRef]
- Rosen, J.W. Zipline’s Ambitious Medical Drone Delivery in Africa. Available online: https://www.technologyreview.com/2017/06/08/151339/blood-from-the-sky-ziplines-ambitious-medical-drone-delivery-in-africa/ (accessed on 30 July 2020).
- Shakhatreh, H.; Sawalmeh, A.H.; Al-Fuqaha, A.; Dou, Z.; Almaita, E.; Khalil, I.; Othman, N.S.; Khreishah, A.; Guizani, M. Unmanned aerial vehicles (UAVs): A survey on civil applications and key research challenges. IEEE Access 2019, 7, 48572–48634. [Google Scholar] [CrossRef]
- Stahl, B.C.; Timmermans, J.; Flick, C. Ethics of emerging information and communication technologies: On the implementation of responsible research and innovation. Sci. Public Policy 2016, scw069. [Google Scholar] [CrossRef]
- UN’s Children Fund. Vanuatu Announces Drone Trial Participants to Assess Vaccine Delivery in Remote Islands—Vanuatu. Available online: https://reliefweb.int/report/vanuatu/vanuatu-announces-drone-trial-participants-assess-vaccine-delivery-remote-islands (accessed on 30 July 2020).
- Van de Voorde, P.; Gautama, S.; Momont, A.; Ionescu, C.M.; De Paepe, P.; Fraeyman, N. The drone ambulance [A-UAS]: Golden bullet or just a blank? Resuscitation 2017, 116, 46–48. [Google Scholar] [CrossRef] [PubMed]
- Moreno, E.L. Concepts, Definitions and Data Sources for the Study of Urbanization: The 2030 Agenda for Sustainable Development. Available online: https://www.un.org/en/development/desa/population/events/pdf/expert/27/papers/II/paper-Moreno-final.pdf (accessed on 6 July 2020).
- United Nations Statistics Division. Population Density and Urbanization. Available online: https://unstats.un.org/unsd/demographic/sconcerns/densurb/densurbmethods.htm (accessed on 30 July 2020).
- Health Canada. A Statistical Profile on the Health of First Nations in Canada: Determinants of Health, 2006–2010; Ministry of Health: Ottawa, ON, Canada, 2014.
- Scheil-Adlung, C. Global Evidence of Inequities in Rural Health Protection. New Data on Rural Deficits in Health Coverage for 174 Countries. Available online: https://reliefweb.int/sites/reliefweb.int/files/resources/RessourcePDF.pdf (accessed on 6 July 2020).
- D’Onfro, J.; Matternet, U.A.V. Delivery Drones—Business Insider. Available online: https://www.businessinsider.com/matternet-uav-delivery-drones-2014-11 (accessed on 30 July 2020).
- Fondation Suisse de Déminage. Case Study No. 2: Delivery- Using Drones for Medical Payload Delivery in Papua New Guinea. Available online: https://reliefweb.int/sites/reliefweb.int/files/resources/2%20Case-Study-No2-PapuaNewGuinea.pdf (accessed on 6 July 2020).
- Subbarao, I.; Cooper, G.P. Drone-based telemedicine: A brave but necessary new world. J. Am. Osteopath. Assoc. 2015, 115, 700–701. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bailey, S. Drones Could Help Fight Coronavirus by Air-Dropping Medical Supplies. Available online: https://edition.cnn.com/2020/04/28/tech/zipline-drones-coronavirus-spc-intl/index.html (accessed on 30 July 2020).
- Sherwood, D. Chilean Seniors Look to the Sky for Medicine and Masks. Available online: https://www.usnews.com/news/world/articles/2020-04-20/chilean-seniors-look-to-the-sky-for-medicine-and-masks (accessed on 30 July 2020).
- MacFarland, M. North Carolina Hospital Turns to Drones to Aid COVID-19 Response—CNN. Available online: https://www.cnn.com/2020/05/28/tech/drones-covid-19-hospital/index.html (accessed on 30 July 2020).
- Wood, C. Spain’s Police Are Flying Drones with Speakers around Public Places to Warn Citizens on Coronavirus Lockdown to Get inside. Available online: https://www.businessinsider.com/spanish-police-using-drones-to-ask-people-stay-at-home-2020-3 (accessed on 30 July 2020).
- Peckham, R.; Sinha, R. Anarchitectures of health: Futures for the biomedical drone. Glob. Public Health 2019, 14, 1204–1219. [Google Scholar] [CrossRef] [PubMed]
- Chafe, R. The value of qualitative description in health services and policy research. Healthc. Policy Polit. Sante 2017, 12, 12–18. [Google Scholar] [CrossRef]
- Pope, C.; Mays, N. Qualitative research: Reaching the parts other methods cannot reach: An introduction to qualitative methods in health and health services research. BMJ 1995, 311, 42–45. [Google Scholar] [CrossRef]
- Nouvet, E.; Abu-Sada, C.; de Laat, S.; Wang, C.; Schwartz, L. Opportunities, limits and challenges of perceptions studies for humanitarian contexts. Can. J. Dev. Stud. Rev. Can. Détudes Dév. 2016, 37, 358–377. [Google Scholar] [CrossRef]
- Nouvet, E.; Schwartz, L. From the front lines: Trialing research ethics in the time of ebola. Prehospital Disaster Med. 2017, 32, S47. [Google Scholar] [CrossRef][Green Version]
- Nouvet, E.; Chan, E.; Schwartz, L.J. Looking good but doing harm? Perceptions of short-term medical missions in Nicaragua. Glob. Public Health 2018, 13, 456–472. [Google Scholar] [CrossRef]
- Alrashdi, I.; Al Qasmi, A. Staff perception of relative importance of quality dimensions for patients atTertiary public services in Oman. Oman Med. J. 2012, 27, 396–401. [Google Scholar] [CrossRef]
- Staňková, P.; Papadaki, Š.; Dvorský, J. Comparative analysis of perception of advantages and disadvantages of integration of hospitals. Em Ekon. Manag. 2018, 21, 101–115. [Google Scholar] [CrossRef]
- Tabler, J.; Scammon, D.L.; Kim, J.; Farrell, T.; Tomoaia-Cotisel, A.; Magill, M.K. Patient care experiences and perceptions of the patient-provider relationship: A mixed method study. Patient Exp. J. 2014, 1, 75–87. [Google Scholar] [CrossRef]
- WeRobotics. Flying Labs. Available online: https://werobotics.org/flying-labs/#:~:text=We%20co%2Dcreate%20and%20facilitate,development%20and%20environmental%20solutions%20locally (accessed on 6 July 2020).
- Welsh, E. Dealing with data: Using NVivo in the qualitative data analysis process. Forum Qual. Soz. Forum Qual. Soc. Res. 2002, 3, 2. [Google Scholar] [CrossRef]
- Maguire, M. Doing a thematic analysis: A practical step-by-step guide for learning and teaching scholars. Irel. J. Teach. Learn. High. Educ. 2017, 3, 33501–33514. [Google Scholar]
- Thorne, S.E. Interpretive Description: Qualitative Research for Applied Practice, 2nd ed.; Routledge: New York, NY, USA, 2016; ISBN 978-1-62958-298-6. [Google Scholar]
- Roberts, K.; Dowell, A.; Nie, J.-B. Attempting rigour and replicability in thematic analysis of qualitative research data; a case study of codebook development. BMC Med. Res. Methodol. 2019, 19, 66. [Google Scholar] [CrossRef]
- Thorne, S.; Kirkham, S.R.; O’Flynn-Magee, K. The analytic challenge in interpretive description. Int. J. Qual. Methods 2004, 3, 1–11. [Google Scholar] [CrossRef]
- Alvial-Palavicino, C.; Garrido-Echeverría, N.; Jiménez-Estévez, G.; Reyes, L.; Palma-Behnke, R. A methodology for community engagement in the introduction of renewable based smart microgrid. Energy Sustain. Dev. 2011, 15, 314–323. [Google Scholar] [CrossRef]
- Gomez, R.; Reed, P.; Chae, H.Y. Assessment of community wellness outcomes to measure ICT impact. In Proceedings of the Sixth International Conference on Information and Communication Technologies and Development, Cape Town, South Africa, 7–10 December 2013. [Google Scholar]
- Heeks, R. Information and Communication Technology for Development (ICT4D); Routledge: New York, NY, USA, 2018; ISBN 978-1-138-10180-7. [Google Scholar]
- Federal Aviation Administration. Community Engagement Toolkits. Available online: https://www.faa.gov/uas/resources/community_engagement/ (accessed on 30 July 2020).
- UAViators Humanitarian UAV Code of Conduct & Guidelines. Available online: https://humanitariandronecode.files.wordpress.com/2017/12/uaviators-code-and-guidelines.pdf (accessed on 6 July 2020).
- Boucher, P. “You wouldn’t have your granny using them”: Drawing boundaries between acceptable and unacceptable applications of civil drones. Sci. Eng. Ethics 2016, 22, 1391–1418. [Google Scholar] [CrossRef]
- Dahl, J.Y.; Sætnan, A.R. “It all happened so slowly”—On controlling function creep in forensic DNA databases. Int. J. Law Crime Justice 2009, 37, 83–103. [Google Scholar] [CrossRef]
- Kindervater, K.H. The emergence of lethal surveillance: Watching and killing in the history of drone technology. Secur. Dialogue 2016, 47, 223–238. [Google Scholar] [CrossRef]
- Hainsworth, J. Vancouver Police Adding Drones to Crime Prevention Arsenal. Available online: https://www.vancouverisawesome.com/vancouver-news/drones-crime-prevention-police-vancouver-1943807 (accessed on 30 July 2020).
- Laksham, K. Unmanned aerial vehicle (drones) in public health: A SWOT analysis. J. Fam. Med. Prim. Care 2019, 8, 342–346. [Google Scholar] [CrossRef] [PubMed]
- Cawthorne, D.; Robbins-van Wynsberghe, A. An ethical framework for the design, development, implementation, and assessment of drones used in public healthcare. Sci. Eng. Ethics 2020, 1–25. [Google Scholar] [CrossRef]
- Powers, R.C. Identifying the Community Power Structure. Available online: http://jonathanstray.com/papers/Identifying_The_Community_Power_Structure.pdf (accessed on 6 July 2020).
- Kuponiyi, F.A. Community power structure: The role of local leaders in community development decision making in Ajaawa, Oyo State, Nigeria. Anthropol. 2008, 10, 239–243. [Google Scholar] [CrossRef]
- United Nations Centre for Human Settlements. (Habitat) Nairobi Community Leadership and Self-Help Housing. Available online: http://www.chs.ubc.ca/archives/files/Community%20Leadership%20and%20Self-Help%20Housing.pdf (accessed on 6 July 2020).
- Brear, M. Ethical research practice or undue influence? Symbolic power in community- and individual-level informed consent processes in community-based participatory research in Swaziland. J. Empir. Res. Hum. Res. Ethics 2018, 13, 311–322. [Google Scholar] [CrossRef]
- Canadian Institute of Health Research; Natural Science and Engineering Research Council of Canada; Social Sciences and Humanities Research Council Tri-Council Policy Statement. Ethical Conduct for Research Involving Humans. Available online: https://ethics.gc.ca/eng/policy-politique_tcps2-eptc2_2018.html (accessed on 30 July 2020).
- Hudson, M. Think globally, act locally: Collective consent and the ethics of knowledge production. Int. Soc. Sci. J. 2009, 60, 125–133. [Google Scholar] [CrossRef]
- Resnik, D.B.; Elliott, K.C. Using Drones to Study Human Beings: Ethical and Regulatory Issues. Sci. Eng. Ethics 2019, 25, 707–718. [Google Scholar] [CrossRef]
- Berg, J.W. All for one and one for all: Informed consent and public health. Fac. Publ. 2012, 12, 1–40. [Google Scholar]
- Public Health Ontario. A Framework for the Ethical Conduct of Public Health Initiatives. Available online: https://www.publichealthontario.ca/-/media/documents/F/2012/framework-ethical-conduct.pdf?la=en (accessed on 7 July 2020).
| United Nation Region | Number of Countries | Number of Individuals |
|---|---|---|
| Latin America and the Caribbean | 2 | 2 |
| Melanesia | 1 | 2 |
| Northern America | 1 | 2 |
| Southern Asia | 1 | 4 |
| Sub-Saharan Africa | 4 | 6 |
| UN Region | Drone Need | Drone Use |
|---|---|---|
| Latin America and the Caribbean (n = 2) |
|
|
| Melanesia * (n = 2) |
|
|
| Northern America (n = 2) |
|
|
| Southern Asia (n = 4) |
|
|
| Sub-Saharan Africa (n = 6) |
|
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeyabalan, V.; Nouvet, E.; Meier, P.; Donelle, L. Context-Specific Challenges, Opportunities, and Ethics of Drones for Healthcare Delivery in the Eyes of Program Managers and Field Staff: A Multi-Site Qualitative Study. Drones 2020, 4, 44. https://doi.org/10.3390/drones4030044
Jeyabalan V, Nouvet E, Meier P, Donelle L. Context-Specific Challenges, Opportunities, and Ethics of Drones for Healthcare Delivery in the Eyes of Program Managers and Field Staff: A Multi-Site Qualitative Study. Drones. 2020; 4(3):44. https://doi.org/10.3390/drones4030044
Chicago/Turabian StyleJeyabalan, Vyshnave, Elysée Nouvet, Patrick Meier, and Lorie Donelle. 2020. "Context-Specific Challenges, Opportunities, and Ethics of Drones for Healthcare Delivery in the Eyes of Program Managers and Field Staff: A Multi-Site Qualitative Study" Drones 4, no. 3: 44. https://doi.org/10.3390/drones4030044
APA StyleJeyabalan, V., Nouvet, E., Meier, P., & Donelle, L. (2020). Context-Specific Challenges, Opportunities, and Ethics of Drones for Healthcare Delivery in the Eyes of Program Managers and Field Staff: A Multi-Site Qualitative Study. Drones, 4(3), 44. https://doi.org/10.3390/drones4030044