Monitoring Older Adults’ Health Information Using Mobile Technology: A Systematic Literature Review †
Abstract
1. Introduction
2. Background
2.1. Self-Reporting
2.2. Data Visualization
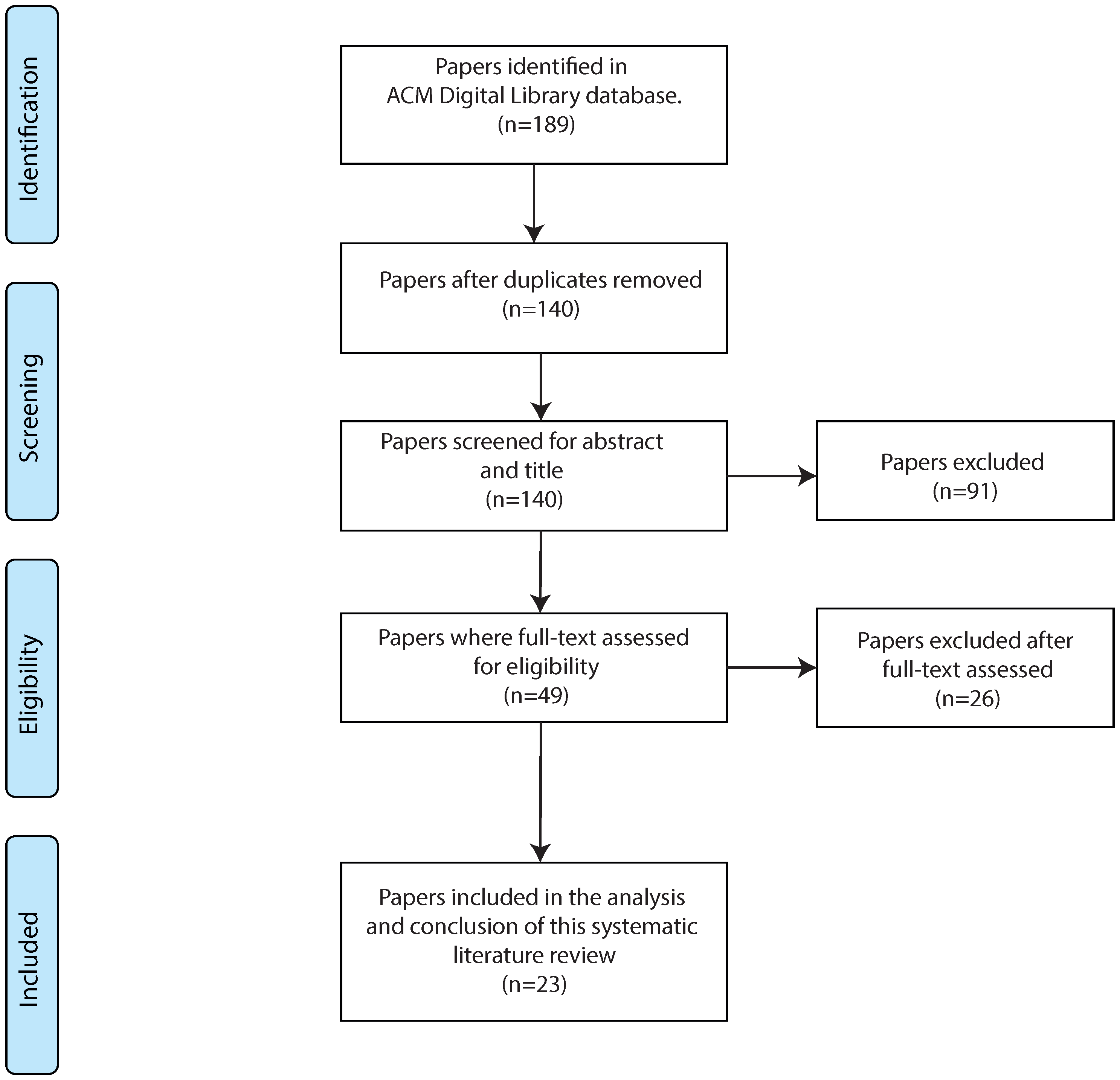
3. Systematic Literature Review Methodology
3.1. Literature Review Methodology
- RQ1 Which types of mobile health technologies have been used to monitor older adults’ health information?
- -
- Do mobile health technologies for older adults include data visualization?
- -
- Do mobile health technologies for older adults include self-reporting?
- RQ2 Which health information about older adults is usually monitored?
- RQ3 How are mobile health technologies for older adults evaluated?
3.2. Search Terms
3.3. Inclusion/Exclusion Criteria
3.4. Data Extraction and Synthesis
4. Results
4.1. Data Extraction and Synthesis
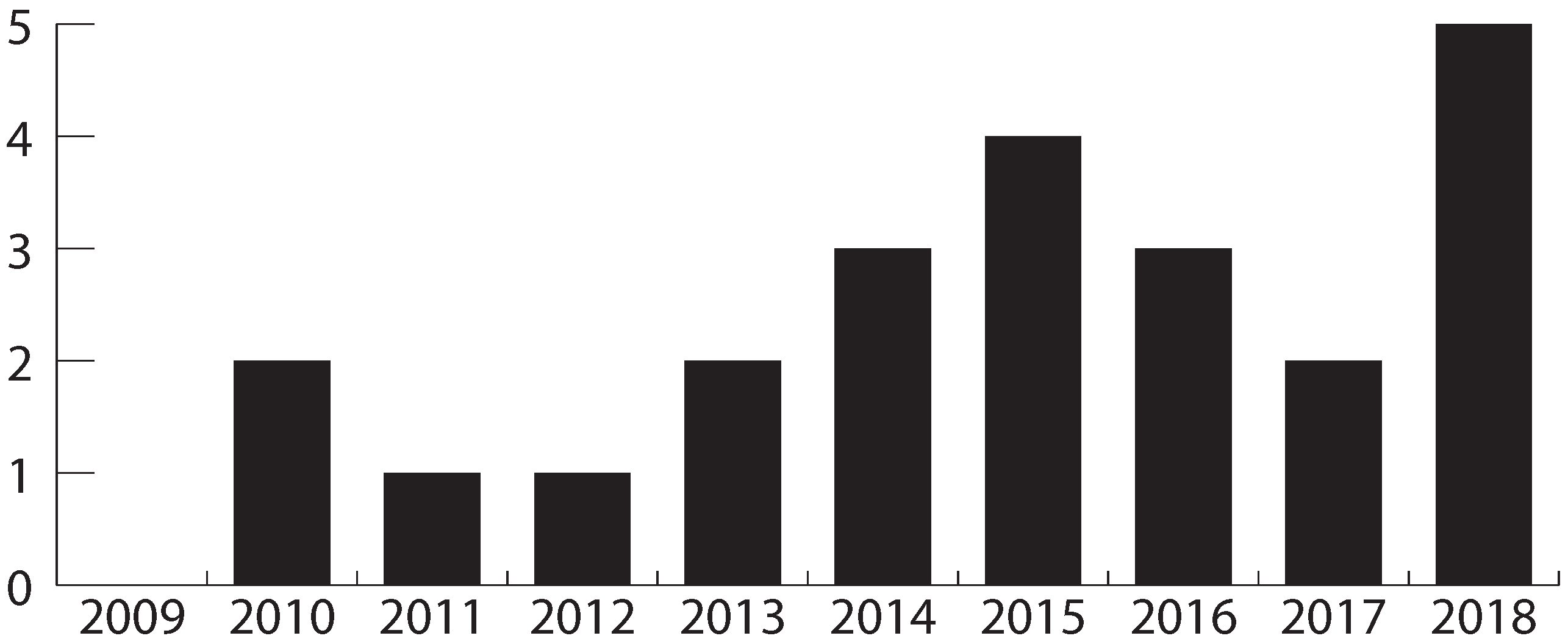
4.2. Characteristics of Included Studies
4.3. RQ1 Which Types of Mobile Health Technologies have been Used to Monitor Older Adults’ Health Information?
4.4. RQ2 Which Health Information about Older Adults is Usually Monitored?
| Study | Type of Technology | Location | Self- Reporting | Data Visualization | ||||
|---|---|---|---|---|---|---|---|---|
| Smart Phone | Smart Bracelet | Accelero- Meter | Heart Rate Sensor | Oximeter | ||||
| [15] | Y | waist | Y | Y | ||||
| [40] | Y | walker | ||||||
| [37] | Y | Y | Y | trunk wrist waist | ||||
| [42] | Y | Y | trunk finger | Y | ||||
| [22] | Y | waist | Y | |||||
| [45] | Y | hand | Y | |||||
| [46] | Y | Y | Y | |||||
| [47] | Y | waist | Y | Y | ||||
| [48] | Y | hand | Y | Y | ||||
| [27] | Y | wrist | Y | Y | ||||
| [30] | Y | wrist | Y | |||||
| [38] | Y | wrist | Y | Y | ||||
| [49] | Y | wrist | ||||||
| [50] | Y | chest | ||||||
| [51] | Y | trunk waist | ||||||
| [16] | Y | wrist | Y | |||||
| [39] | Y | Y | Y | wheelchair | Y | Y | ||
| [32] | Y | hand | Y | Y | ||||
| [44] | Y | hand | Y | |||||
| [52] | Y | chest knee | ||||||
| [41] | Y | Y | wrist waist | Y | Y | |||
| [53] | Y | hand | ||||||
| [43] | Y | Y | Y | chest wrist finger | Y | |||
| Data Monitored | Study | Definition |
|---|---|---|
| Position | [15,40,41,43] | Location on the map |
| Activity time | [15] | Activity duration |
| Acceleration | [15,22,30,38,45,46] [16,41,49,50,51,52] | Change of velocity of an object with respect to time |
| Heart rate | [30,37,39,42,43] | Heartbeat counting |
| Oxygen level | [37,42,43] | Oxygen saturation level |
| Medical appointments | [48] | Planning for a visit to a health care professional |
| Chronic pain | [27] | Usually chronic pain is because of an illness |
| Emotions | [27] | Feelings in a certain context |
| Sleep patterns | [30] | Characteristics of sleep including cycle, intensity, quality |
| Pulse | [39,43] | Mechanical vibration of blood flow |
| Medication management | [32,44] | Regulation of the quantity and frequency of medications |
| Energy consumption | [41] | Amount of energy or power used |
4.5. RQ3 How Are Mobile Health Technologies for Older Adults Evaluated?
5. Discussion
6. Conclusions and Future Work
Funding
Conflicts of Interest
References
- Katzmarzyk, P.T.; Mason, C. The physical activity transition. J. Phys. Act. Health 2009, 6, 269–280. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.Y.; Lee, J. Smart devices for older adults managing chronic disease: A scoping review. JMIR MHealth UHealth 2017, 5, e69. [Google Scholar] [CrossRef] [PubMed]
- Joe, J.; Demiris, G. Older adults and mobile phones for health: A review. J. Biomed. Inform. 2013, 46, 947–954. [Google Scholar] [CrossRef]
- Kuerbis, A.; Mulliken, A.; Muench, F.; Moore, A.A.; Gardner, D. Older adults and mobile technology: Factors that enhance and inhibit utilization in the context of behavioral health. Ment. Health Addict. Res. 2017, 2, 1–11. [Google Scholar] [CrossRef]
- Patel, K.V.; Guralnik, J.M.; Dansie, E.J.; Turk, D.C. Prevalence and impact of pain among older adults in the United States: Findings from the 2011 National Health and Aging Trends Study. Pain 2013, 154, 2649–2657. [Google Scholar] [CrossRef]
- Stedmon, A.W.; Howells, H.; Wilson, J.R.; Dianat, I. Ergonomics/human factors needs of an ageing workforce in the manufacturing sector. Health Promot. Perspect. 2012, 2, 112. [Google Scholar]
- OECD. Skills Matter: Further Results from the Survey of Adult Skills. In series: OECD Skills Studies, 2016. Available online: https://www.oecd.org/skills/piaac/Skills_Matter_Further_Results_from_the_Survey_of_Adult_Skills.pdf (accessed on 1 July 2019).
- Bhattarai, P.; Phillips, J.L. The role of digital health technologies in management of pain in older people: An integrative review. Arch. Gerontol. Geriatr. 2017, 68, 14–24. [Google Scholar] [CrossRef]
- Van Deursen, A.J.; Helsper, E.J. A nuanced understanding of Internet use and non-use among the elderly. Eur. J. Commun. 2015, 30, 171–187. [Google Scholar] [CrossRef]
- Harjumaa, M.; Isomursu, M. Field Work With Older Users-Challenges in Design and Evaluation of Information Systems. Electron. J. Inf. Syst. Eval. 2012, 15, 50–62. [Google Scholar]
- dos Santos, T.D.; Santana, V.F.D. Computer Anxiety and Interaction: A Systematic Review. In Proceedings of the Internet of Accessible Things, Lyon, France, 23–25 April 2018; pp. 18:1–18:10. [Google Scholar] [CrossRef]
- Holgersson, J.; Söderström, E. Bridging the gap: Exploring elderly citizens’ perceptions of digital exclusion. In Proceedings of the 27th European Conference on Information Systems (ECIS), Stockholm & Uppsala, Sweden, 8–14 June 2019. [Google Scholar]
- Yin, D.; Chen, K. The essential mechanisms of aging: Irreparable damage accumulation of biochemical side-reactions. Exp. Gerontol. 2005, 40, 455–465. [Google Scholar] [CrossRef]
- Searcy, R.P.; Summapund, J.; Estrin, D.; Pollak, J.P.; Schoenthaler, A.; Troxel, A.B.; Dodson, J.A. Mobile Health Technologies for Older Adults with Cardiovascular Disease: Current Evidence and Future Directions. Curr. Geriatr. Rep. 2019, 8, 31–42. [Google Scholar] [CrossRef]
- Castro, L.A.; Favela, J.; Quintana, E.; Perez, M. Behavioral data gathering for assessing functional status and health in older adults using mobile phones. Pers. Ubiquitous Comput. 2015, 19, 379–391. [Google Scholar] [CrossRef]
- Matthies, D.J.; Haescher, M.; Nanayakkara, S.; Bieber, G. Step Detection for Rollator Users with Smartwatches. In Proceedings of the Symposium on Spatial User Interaction, Berlin, Germany, 13–14 October 2018; pp. 163–167. [Google Scholar]
- Cook, E.J.; Randhawa, G.; Sharp, C.; Ali, N.; Guppy, A.; Barton, G.; Bateman, A.; Crawford-White, J. Exploring the factors that influence the decision to adopt and engage with an integrated assistive telehealth and telecare service in Cambridgeshire, UK: A nested qualitative study of patient ‘users’ and ‘non-users’. BMC Health Serv. Res. 2016, 16, 137. [Google Scholar] [CrossRef]
- Gokalp, H.; Clarke, M. Monitoring activities of daily living of the elderly and the potential for its use in telecare and telehealth: A review. Telemed. E-Health 2013, 19, 910–923. [Google Scholar] [CrossRef]
- Cajamarca, G.; Rodríguez, I.; Herskovic, V.; Campos, M.; Riofrío, J. StraightenUp+: Monitoring of Posture during Daily Activities for Older Persons Using Wearable Sensors. Sensors 2018, 18, 3409. [Google Scholar] [CrossRef]
- Villalba, E.; Salvi, D.; Ottaviano, M.; Peinado, I.; Arredondo, M.T.; Akay, A. Wearable and mobile system to manage remotely heart failure. IEEE Trans. Inf. Technol. Biomed. 2009, 13, 990–996. [Google Scholar] [CrossRef] [PubMed]
- Simpson, L.; Maharaj, M.M.; Mobbs, R.J. The role of wearables in spinal posture analysis: A systematic review. BMC Musculoskelet. Disord. 2019, 20, 55. [Google Scholar] [CrossRef] [PubMed]
- Dai, J.; Bai, X.; Yang, Z.; Shen, Z.; Xuan, D. Mobile phone-based pervasive fall detection. Pers. Ubiquitous Comput. 2010, 14, 633–643. [Google Scholar] [CrossRef]
- Bush, T.L.; Miller, S.R.; Golden, A.L.; Hale, W.E. Self-report and medical record report agreement of selected medical conditions in the elderly. Am. J. Public Health 1989, 79, 1554–1556. [Google Scholar] [CrossRef] [PubMed]
- Schootman, M.; Jeffe, D.B.; West, M.M.; Aft, R. Self-report by elderly breast cancer patients was an acceptable alternative to surveillance, epidemiology, and end results (SEER) abstract data. J. Clin. Epidemiol. 2005, 58, 1316–1319. [Google Scholar] [CrossRef]
- Skinner, K.M.; Miller, D.R.; Lincoln, E.; Lee, A.; Kazis, L.E. Concordance between respondent self-reports and medical records for chronic conditions: Experience from the Veterans Health Study. J. Ambul. Care Manag. 2005, 28, 102–110. [Google Scholar] [CrossRef]
- Rozario, P.A.; Morrow-Howell, N.; Proctor, E. Comparing the congruency of self-report and provider records of depressed elders’ service use by provider type. Med. Care 2004, 42, 952–959. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rodriguez, I.; Herskovic, V.; Fuentes, C.; Campos, M. B-ePain: A wearable interface to self-report pain and emotions. In Proceedings of the 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing: Adjunct, Heidelberg, Germany, 12–16 September 2016; pp. 1120–1125. [Google Scholar]
- Hawthorn, D. Possible implications of aging for interface designers. Interact. Comput. 2000, 12, 507–528. [Google Scholar] [CrossRef]
- Le, T.; Chi, N.C.; Chaudhuri, S.; Thompson, H.J.; Demiris, G. Understanding older adult use of data visualizations as a resource for maintaining health and wellness. J. Appl. Gerontol. 2018, 37, 922–939. [Google Scholar] [CrossRef] [PubMed]
- Hu, R.; Pham, H.; Buluschek, P.; Gatica-Perez, D. Elderly people living alone: Detecting home visits with ambient and wearable sensing. In Proceedings of the 2nd International Workshop on Multimedia for Personal Health and Health Care, Mountain View, CA, USA, 23 October 2017; pp. 85–88. [Google Scholar]
- Macdonald, A.S.; Loudon, D.; Rowe, P.J.; Samuel, D.; Hood, V.; Nicol, A.C.; Grealy, M.A.; Conway, B.A. Towards a design tool for visualizing the functional demand placed on older adults by everyday living tasks. Univers. Access Inf. Soc. 2007, 6, 137–144. [Google Scholar] [CrossRef]
- Hamid, A.; Sym, F.P. Designing for patient-centred factors in medical adherence technology. In Proceedings of the 6th International Conference on Rehabilitation Engineering & Assistive Technology, Tampines, Singapore, 24–26 July 2012; p. 40. [Google Scholar]
- Skubic, M.; Guevara, R.D.; Rantz, M. Automated health alerts using in-home sensor data for embedded health assessment. IEEE J. Transl. Eng. Health Med. 2015, 3, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Reeder, B.; Chung, J.; Le, T.; Thompson, H.; Demiris, G. Assessing older adults’ perceptions of sensor data and designing visual displays for ambient environments. Methods Inf. Med. 2014, 53, 152–159. [Google Scholar] [PubMed]
- Le, T.; Reeder, B.; Thompson, H.; Demiris, G. Health providers’ perceptions of novel approaches to visualizing integrated health information. Methods Inf. Med. 2013, 52, 250–258. [Google Scholar]
- Kitchenham, B.; Charters, S. Guidelines for Performing Systematic Literature Reviews in Software Engineering; Technical Report EBSE 2007-01; Keele University and Durham University: Keele, UK, 2007. [Google Scholar]
- Juen, J.; Cheng, Q.; Schatz, B. Towards a natural walking monitor for pulmonary patients using simple smart phones. In Proceedings of the 5th ACM Conference on Bioinformatics, Computational Biology, and Health Informatics, Newport Beach, CA, USA, 20–23 September 2014; pp. 53–62. [Google Scholar]
- Cherian, J.; Rajanna, V.; Goldberg, D.; Hammond, T. Did you remember to brush?: A noninvasive wearable approach to recognizing brushing teeth for elderly care. In Proceedings of the 11th EAI International Conference on Pervasive Computing Technologies for Healthcare, Barcelona, Spain, 23–26 May 2017; pp. 48–57. [Google Scholar]
- Wong, S.F.; Hoi, W.K.; Wan, I.K. Advanced Smart Wheelchair Design in Enhancing Quality of Life for Elder and Handicapped People. In Proceedings of the 4th International Conference on Industrial and Business Engineering, Macau, Macao, 24–26 October 2018; pp. 203–210. [Google Scholar]
- Ojeda, M.; Cortés, A.; Béjar, J.; Cortés, U. Automatic classification of gait patterns using a smart rollator and the BOSS model. In Proceedings of the 11th PErvasive Technologies Related to Assistive Environments Conference, Corfu, Greece, 26–29 June 2018; pp. 384–390. [Google Scholar]
- Nakagawa, E.; Moriya, K.; Suwa, H.; Fujimoto, M.; Arakawa, Y.; Hatta, T.; Miwa, S.; Yasumoto, K. Investigating recognition accuracy improvement by adding user’s acceleration data to location and power consumption-based in-home activity recognition system. In Proceedings of the Adjunct Proceedings of the 13th International Conference on Mobile and Ubiquitous Systems: Computing Networking and Services, Hiroshima, Japan, 28 November–1 December 2016; pp. 100–105. [Google Scholar]
- Cheng, Q.; Juen, J.; Schatz, B.R. Using mobile phones to simulate pulse oximeters: Gait analysis predicts oxygen saturation. In Proceedings of the 5th ACM Conference on Bioinformatics, Computational Biology, and Health Informatics, Newport Beach, CA, USA, 20–23 September 2014; pp. 331–340. [Google Scholar]
- Nazário, D.C.; de Andrade, A.; Borges, L.; Ramos, W.R.; Todesco, J.L.; Dantas, M.A.R. An Enhanced Quality of Context Evaluating Approach in the e-Health Sensor Platform. In Proceedings of the 11th ACM Symposium on QoS and Security for Wireless and Mobile Networks, Cancun, Mexico, 2–6 November 2015; pp. 1–7. [Google Scholar]
- Rodríguez, M.D.; García-Vázquez, J.P.; Andrade, Á.G. Design dimensions of ambient information systems to facilitate the development of AAL environments. In Proceedings of the 4th International Conference on PErvasive Technologies Related to Assistive Environments, Heraklion, Crete, Greece, 25–27 May 2011; p. 4. [Google Scholar]
- Sunwoo, J.; Yuen, W.; Lutteroth, C.; Wünsche, B. Mobile games for elderly healthcare. In Proceedings of the 11th International Conference of the NZ Chapter of the ACM Special Interest Group on Human-Computer Interaction, Auckland, New Zealand, 8–9 July 2010; pp. 73–76. [Google Scholar]
- Martín, H.; Bernardos, A.M.; Iglesias, J.; Casar, J.R. Activity logging using lightweight classification techniques in mobile devices. Pers. Ubiquitous Comput. 2013, 17, 675–695. [Google Scholar] [CrossRef]
- Fontecha, J.; Navarro, F.J.; Hervás, R.; Bravo, J. Elderly frailty detection by using accelerometer-enabled smartphones and clinical information records. Pers. Ubiquitous Comput. 2013, 17, 1073–1083. [Google Scholar] [CrossRef]
- Monteiro, J.M.; Lopes, C.T. HealthTalks-A Mobile App to Improve Health Communication and Personal Information Management. In Proceedings of the 2018 Conference on Human Information Interaction & Retrieval, New Brunswick, NJ, USA, 11–15 March 2018; pp. 329–332. [Google Scholar]
- Bieber, G.; Haescher, M.; Hanschmann, P.; Matthies, D.J. Exploring Accelerometer-based Step Detection By using a Wheeled Walking Frame. In Proceedings of the 5th international Workshop on Sensor-based Activity Recognition and Interaction, Berlin, Germany, 20–21 September 2018; p. 8. [Google Scholar]
- Fourlas, G.K.; Maglogiannis, I. Human movement detection using attitude and heading reference system. In Proceedings of the 7th International Conference on PErvasive Technologies Related to Assistive Environments, Rhodes, Greece, 27–30 May 2014; p. 30. [Google Scholar]
- Alemdar, H.Ö.; Yavuz, G.R.; Özen, M.O.; Kara, Y.E.; Incel, Ö.D.; Akarun, L.; Ersoy, C. Multi-modal fall detection within the WeCare framework. In Proceedings of the 9th ACM/IEEE International Conference on Information Processing in Sensor Networks, Stockholm, Sweden, 12–16 April 2010; pp. 436–437. [Google Scholar]
- Ojetola, O.; Gaura, E.; Brusey, J. Data set for fall events and daily activities from inertial sensors. In Proceedings of the 6th ACM multimedia systems conference, Portland, OR, USA, 18–20 March 2015; pp. 243–248. [Google Scholar]
- Fareed, U. Smartphone sensor fusion based activity recognition system for elderly healthcare. In Proceedings of the 2015 Workshop on Pervasive Wireless Healthcare, Hangzhou, China, 22 June 2015; pp. 29–34. [Google Scholar]
- Delbaere, K.; Valenzuela, T.; Woodbury, A.; Davies, T.A.; Yeong, J.J.; Steffens, D.; Miles, L.; Pickett, L.; Zijlstra, G.A.R.; Clemson, L.; et al. Evaluating the effectiveness of a home-based exercise programme delivered through a tablet computer for preventing falls in older community-dwelling people over 2 years: Study protocol for the Standing Tall randomised controlled trial. BMJ Open 2015, 5, e009173. [Google Scholar] [CrossRef]
- Arkkukangas, M.; Söderlund, A.; Eriksson, S.; Johansson, A.C. Fall Preventive Exercise With or Without Behavior Change Support for Community-Dwelling Older Adults: A Randomized Controlled Trial With Short-Term Follow-up. J. Geriatr. Phys. Ther. 2019, 42, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Lau, K.M.; Parikh, M.; Harvey, D.J.; Huang, C.J.; Farias, S.T. Early Cognitively Based Functional Limitations Predict Loss of Independence in Instrumental Activities of Daily Living in Older Adults. J. Int. Neuropsychol. Soc. 2015, 21, 688–698. [Google Scholar] [CrossRef] [PubMed]
- Kruse, C.S.; Mileski, M.; Moreno, J. Mobile health solutions for the aging population: A systematic narrative analysis. J. Telemed. Telecare 2017, 23, 439–451. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, I.; Herskovic, V.; Gerea, C.; Fuentes, C.; Rossel, P.O.; Marques, M.; Campos, M. Understanding Monitoring Technologies for Adults With Pain: Systematic Literature Review. J. Med Internet Res. 2017, 19, e364. [Google Scholar] [CrossRef]
- Roeing, K.L.; Hsieh, K.L.; Sosnoff, J.J. A systematic review of balance and fall risk assessments with mobile phone technology. Arch. Gerontol. Geriatr. 2017, 73, 222–226. [Google Scholar] [CrossRef]
- Elavsky, S.; Knapova, L.; Klocek, A.; Smahel, D. Mobile Health Interventions for Physical Activity, Sedentary Behavior, and Sleep in Adults Aged 50 Years and Older: A Systematic Literature Review. J. Aging Phys. Act. 2019, 27, 565–593. [Google Scholar] [CrossRef]

| Criteria | Description |
|---|---|
| Population | Older adults |
| Intervention | Mobile technologies for health monitoring developed specifically for older adults |
| Comparison | No comparison |
| Outcome | Identify and analyze mobile technologies for health monitoring focused on older adults |
| Context | Health monitoring |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cajamarca, G.; Herskovic, V.; Rossel, P.O. Monitoring Older Adults’ Health Information Using Mobile Technology: A Systematic Literature Review. Proceedings 2019, 31, 62. https://doi.org/10.3390/proceedings2019031062
Cajamarca G, Herskovic V, Rossel PO. Monitoring Older Adults’ Health Information Using Mobile Technology: A Systematic Literature Review. Proceedings. 2019; 31(1):62. https://doi.org/10.3390/proceedings2019031062
Chicago/Turabian StyleCajamarca, Gabriela, Valeria Herskovic, and Pedro O. Rossel. 2019. "Monitoring Older Adults’ Health Information Using Mobile Technology: A Systematic Literature Review" Proceedings 31, no. 1: 62. https://doi.org/10.3390/proceedings2019031062
APA StyleCajamarca, G., Herskovic, V., & Rossel, P. O. (2019). Monitoring Older Adults’ Health Information Using Mobile Technology: A Systematic Literature Review. Proceedings, 31(1), 62. https://doi.org/10.3390/proceedings2019031062






