Micromachined Tube Type Thermal Flow Sensor for Adult-Sized Tracheal Intubation Tube †
Abstract
:1. Introduction
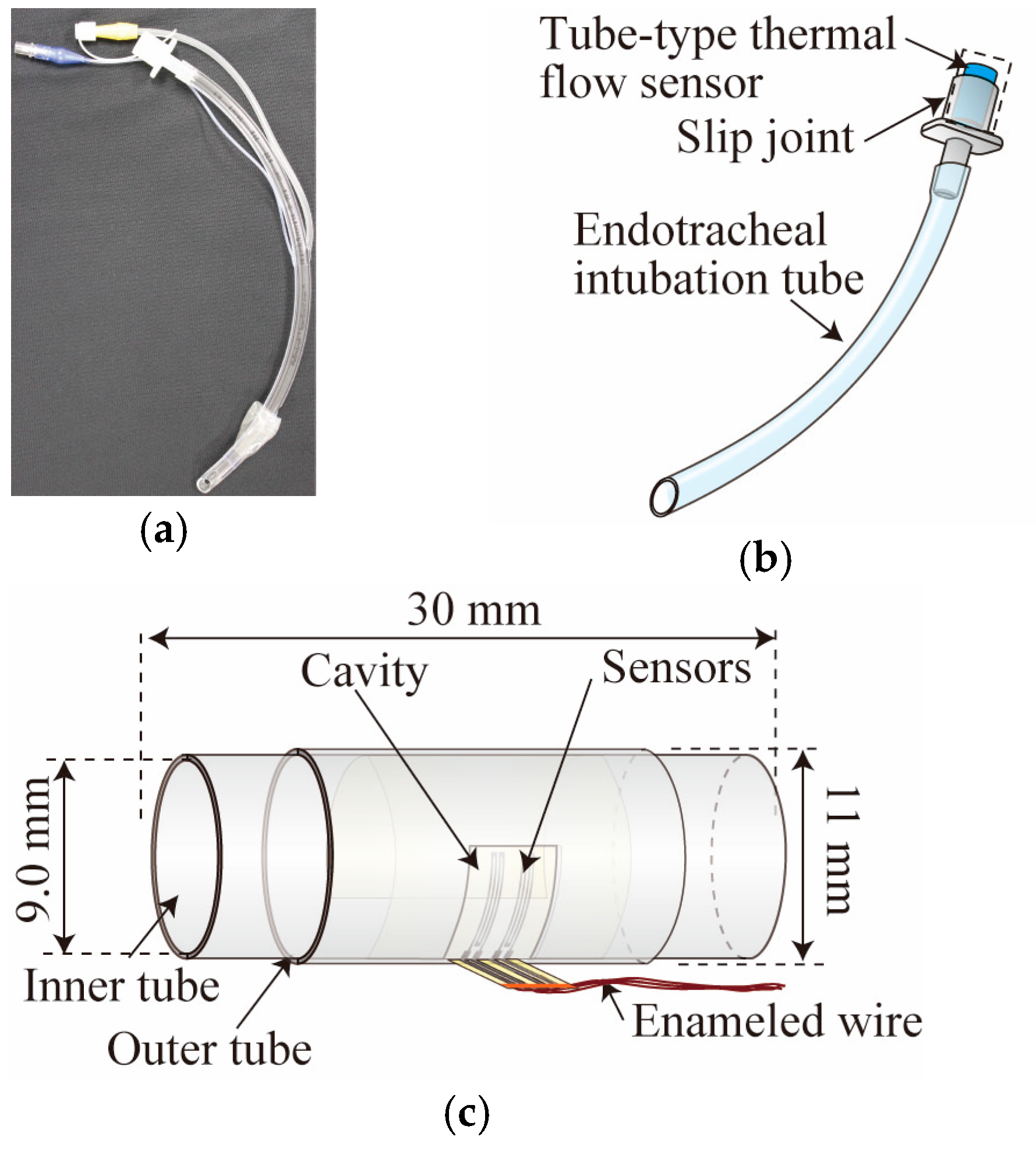
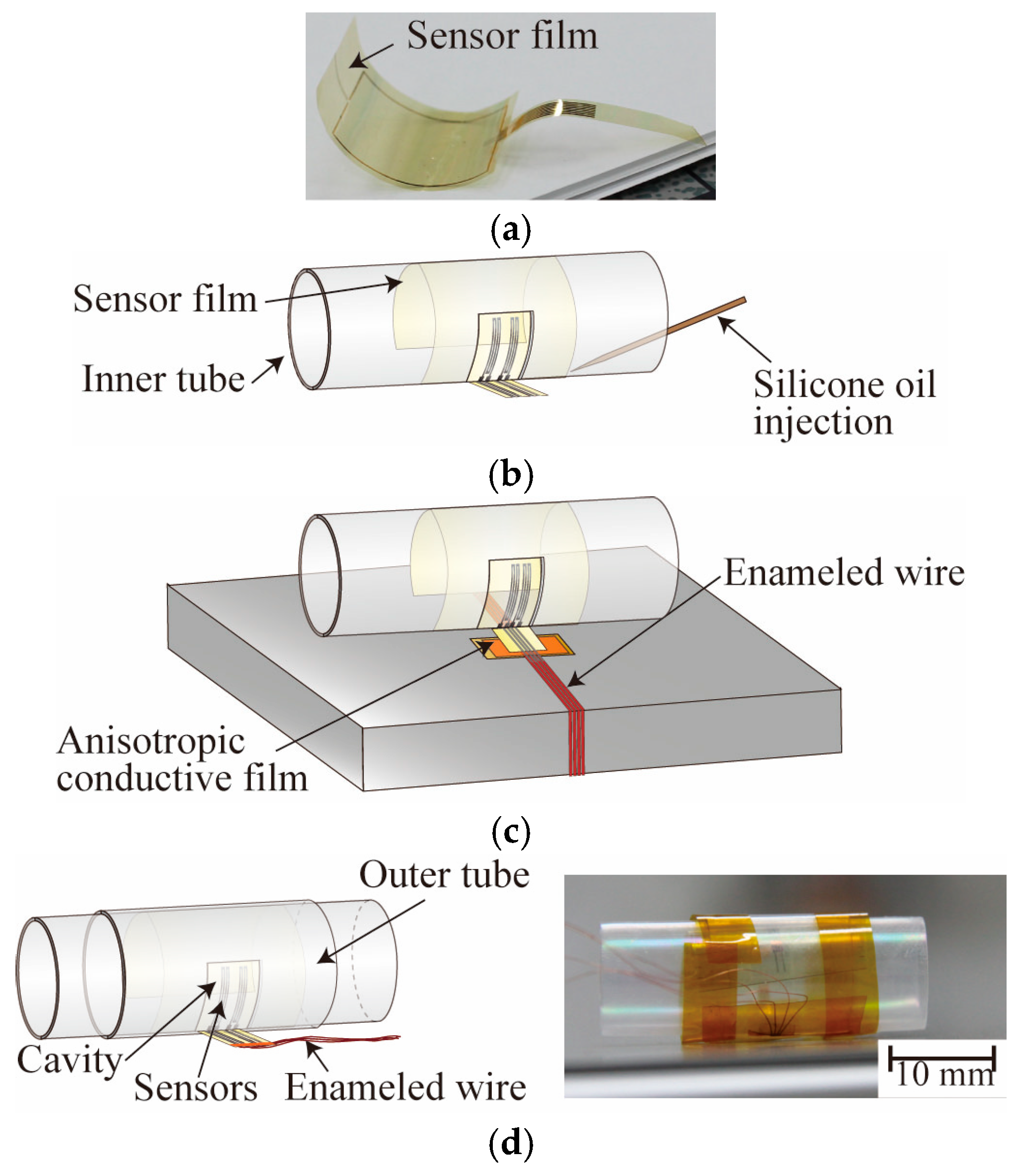
2. Tube-Type Thermal Flow Sensor
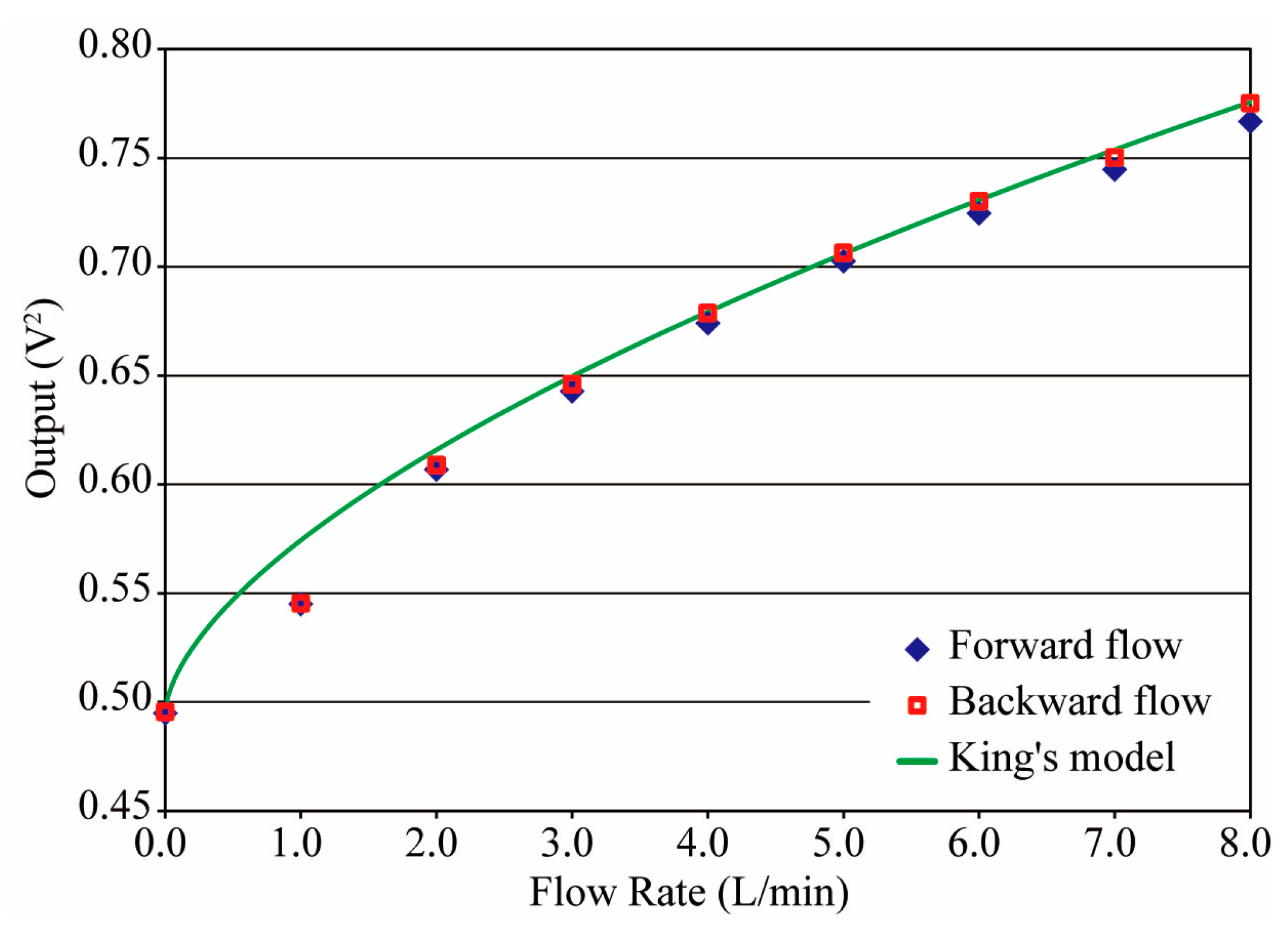
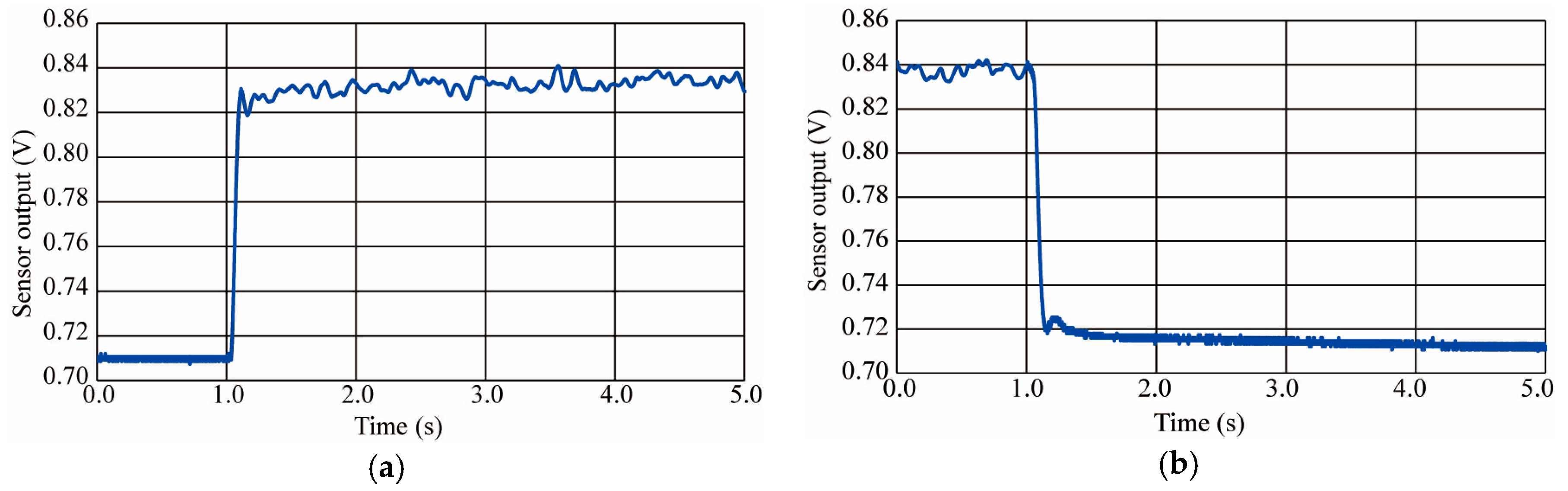
3. Characteristics
4. Conclusions
Acknowledgments
Conflicts of Interest
References
- YAO TOKUSYUKAI General Hospital ICU Manual, version 2009.
- Matsuyama, T.; Yoshikawa, K.; Yamazaki, Y.; Shikida, M.; Matsushima, M.; Kawabe, T. Integration of catheter flow sensor onto tracheal intubation tube sys-tem. In Proceedings of the Tech. Digest. MEMS Conference, Taipei, Taiwan, 20–24 January 2013; pp. 567–570. [Google Scholar]
- Shikida, M.; Yoshikawa, K.; Matsuyama, T.; Yamazaki, Y.; Matsushima, M.; Kawabe, T. Catheter flow sensor with temperature compensation for tracheal intubation tube system. Sens. Actuators A 2014, 215, 155–160. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Watanabe, S.; Hasegawa, Y.; Matsushima, M.; Kawabe, T.; Shikida, M. Micromachined Tube Type Thermal Flow Sensor for Adult-Sized Tracheal Intubation Tube. Proceedings 2017, 1, 357. https://doi.org/10.3390/proceedings1040357
Watanabe S, Hasegawa Y, Matsushima M, Kawabe T, Shikida M. Micromachined Tube Type Thermal Flow Sensor for Adult-Sized Tracheal Intubation Tube. Proceedings. 2017; 1(4):357. https://doi.org/10.3390/proceedings1040357
Chicago/Turabian StyleWatanabe, Shun, Yoshihiro Hasegawa, Miyoko Matsushima, Tsutomu Kawabe, and Mitsuhiro Shikida. 2017. "Micromachined Tube Type Thermal Flow Sensor for Adult-Sized Tracheal Intubation Tube" Proceedings 1, no. 4: 357. https://doi.org/10.3390/proceedings1040357
APA StyleWatanabe, S., Hasegawa, Y., Matsushima, M., Kawabe, T., & Shikida, M. (2017). Micromachined Tube Type Thermal Flow Sensor for Adult-Sized Tracheal Intubation Tube. Proceedings, 1(4), 357. https://doi.org/10.3390/proceedings1040357



